Author(s): Mukesh Kumar*, Fnu Sonia, Hamza Ahsan, Ahmed Abdul Rahman Abbasi and Kristin Swedish
Lung cancer is number one cause of cancer mortality in United States both in men and women. Lung cancer is uncommon in patients younger than 35 years with no smoking and family history. Malignancy from lung nodule depends on size, growth rate, borders, calcification and location. Appropriate follow up for lung nodules in older patient with risk factors has been well described in literature based on various researches. However there is very limited data regarding follow up and management of lung nodule in younger patient with risk factors. We describe a patient who was 30 year old when he presented with acute appendicitis and incidentally found to have lung nodule of 1.2 cm. It was decided that patient should follow up as an outpatient for lung nodule. As patient was uninsured with poor socioeconomic he never followed up as outpatient. After 2 years patient was diagnosed with stage IV lung adenocarcinoma and died shortly after. Guidelines should be used in the proper clinical context as a tool to help with patient management, though exceptions always exist. Some expert believe lung nodule between 8-30 mm in patient with poor follow-up due to socioeconomic status, psychological issues, or young age should get complete resection of nodule.
Lung cancer is uncommon in patients younger than 35 years old with no prior tobacco use history, environmental exposure, or family history. Adenocarcinoma, the most common type of lung cancer, most commonly presents as a pulmonary nodule. A pulmonary nodule is a rounded or irregular opacity, which may be well or poorly defined, measuring ≤3 cm in diameter [1]. Certain features of the nodule, including size and consistency, can be used to estimate the risk of progression to lung cancer. We discuss the case of a young patient who had a 12 mm lung nodule discovered incidentally on computerized tomography (CT) that developed to Stage IV adenocarcinoma in two years.
A 30-year-old man who presented with abdominal pain from appendicitis underwent abdominal CT scan and was incidentally found to have 12 mm irregularly bordered lung nodule. No prior chest imaging was available. Patient was discharged after an uneventful appendectomy and was advised to have follow-up imaging, but was thereafter lost to follow up due to lack of insurance. Two years later the patient presented with a productive cough and scant hemoptysis. A CT scan of the chest then revealed a 6.7 cm lung mass. Carcinoid tumor was suspected but octreotide scan was negative. A CT guided lung biopsy revealed adenocarcinoma positive for EGFR mutation. Patient was discharged with outpatient Oncology follow-up. Three weeks later, he was admitted with headache and right arm weakness. Magnetic resonance imaging (MRI) of the brain revealed left sided metastases in the parietal and occipital lobe, confirming stage IV disease. After resection of brain metastases, he was started on chemotherapy. Patient then had a rapid progression of disease with worsening CNS and bone metastasis. He died one year after diagnosis.
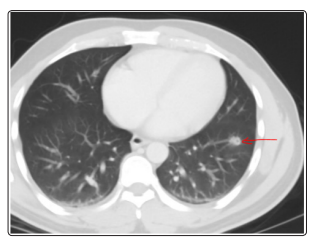
Image 1: 1.2 solid lung nodule at left lower Lobe (08/2016)
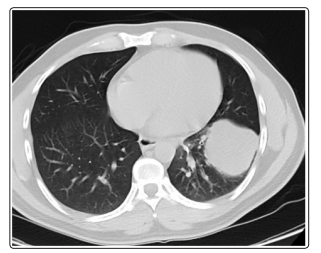
Image 2: 6.7 round parenchymal mass (09/2018)
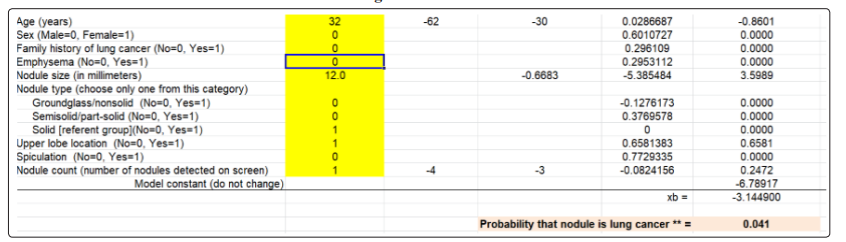
Risk of a lung nodule being malignant depends on size, consistency, and patient risk factors. According to some studies, the risk ofmalignancy in a nodule of 5 mm is < 1%, 5-9 mm is 2-6%, 8-20 mm is 18%, and > 20 mm is 50% [4-6]. Solid nodules have more risk than semi-solid and ground glass nodules [3]. Significant risk factors include cigarette smoking, age greater than 35 years, female gender, radiation history, exposure to environmental toxins, pulmonary fibrosis, alcohol consumption, and positive family history [5]. According to the Guidelines from Fleischner Society, management of solitary lung nodules depends on size of nodule and probability of malignancy. According to these guidelines, nodules are divided into low probability, intermediate probability, and high probability based on risk factors, nodule size, and type of nodule [5]. Solid nodules less than 6mm in low risk patients do not need further workup. Solid nodules more than 8mm are evaluated along with other risks, including age, smoking history, location within the lung, and presence of spiculation. Nodules more than 8mm in low- and intermediate risk patient patients should have CT chest at 3 months, PET scan or tissue sampling [2, 9]. Solid nodules more than 8 mm in high risk patients need immediate evaluation for resection or more aggressive measures. These guidelines are already set and applied to the general population, however in clinical practice management decisions are often influenced by multiple other factors, including cost, availability of testing and treatment modalities, socioeconomic status, and risk of not following up. According to one study, patients with early-stage lung cancer in the highest income decile were 45% more likely to receive surgical treatment and 102% more likely to attain 5-year survival than those in the lowest income decile [10].
Our patient was non documented, uninsured, and did not follow up. He had a 12 mm solid nodule on initial scan with a low probability of cancer according to one of the risk calculators for lung nodules, as shown in Table 1 [5].
Our patient should have received appropriate management, either PET scan or resection, as some experts suggest to do either nonsurgical biopsy or resection in patients with nodules between 8-30 mm and concern for poor follow-up (due to socioeconomic status, psychological issues, or young age). Lung adenocarcinoma diagnosed at Stage IV has a five year survival rate of 10% compared to five year survival of 60-80% when diagnosed at Stage I [7,8].
Guidelines should be used in the proper clinical context as a tool to help with patient management, though exceptions always exist. The patient in this case presented two years after the finding of an incidental nodule with cancer that had progressed to stage IV. A timely intervention with biopsy or resection of the nodule on the first presentation could have altered this course, knowing the patient will not be able to follow up due to his socioeconomic status.
