Author(s): TadaoTsuji*, G Sun, A Sugiyama, Y Amano, S Mano, T Shinobi, H Tanaka, M.Kubochi, Ohishi,Y Moriya, M Ono, T Masuda, H Shinozaki, H Kaneda, H Katsura,T Mizutani, K Miura, M Katoh, K Yamafuji, K Takeshima, N Okamoto and S Nyuhzuki
We have treated 47 cases of incomplete pancreatic divisum (IPD) in theses 7 years. They were classified by the modified“Hirooka’s classification”— stenotic fusion type I / II, ansa pancreatica type, branch fusion type I / II / III, and one was unclassified. 36 cases were treated by ESWL and/or endoscopy. In difficult cases, we performed our new endoscopic procedures-rendezvous precut method and reverse balloon dilation method, with good results. The therapeutic success rate of IPD via major papilla was 100% (10/10) and via minor papilla 96% (24/25) without severe complications. After endoscopic treatment, the prognosis was good in 32, fair in 3 and one had an operation. In calcified IPD cases, endoscopic treatments were performed many times by stone and pain relapse, and EPS is still placed in 24 cases.
In the literature, papers about the treatment of incomplete pancreatic divisum (IPD) are few, so we would like to report about the treatment methods of IPD in our hospital, especially 2 new procedures; rendezvous pre-cut method and reverse balloon method.
In these 7 years, we have experienced 47 cases of IPD. They consisted of 33 male and 14 female, aged 13-90 y/o (mean 63). It was 3.0% of naïve ERP cases in this period. The states of disease were 4 ARP (acute relapsing pancreatitis), 36 CH (chronic pancreatitis), and 7 asymptomatic without duct deformity. We classified them with the modified “Hirooka’s classification” (Figure1) into stenotic fusion type I / II, ansa pancreatica type, branch fusion type I / II / III ( Table 1), and each case number was 3,1,0,15,0, and 27 respectively [1]. One case was unclassified.
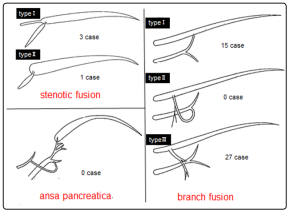
Figure 1: Modified Hirooka’s classification of Incomplete pancreas divisum
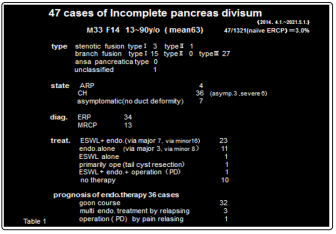
34 cases were diagnosed by ERP and 13 by MRCP. The 37 symptomatic cases consisted of 29 male, 8 female (calcified 31,alcoholic 30) and the 10 asymptomatic cases consisted of 3 male, 7 female (calcified 2,alcoholic 3) (Table 2). Severe pancreatitis cases with pseudocysts were all calcified alcoholic male cases.
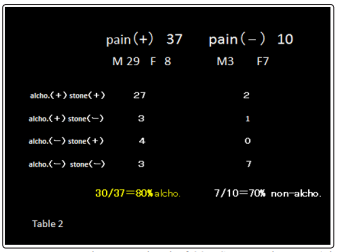
Treatment procedures consisted of 23 ESWL+endoscopy (via major papilla 7, via minor papilla 16), 11 endoscopy alone (via major 3, via minor 8), 1 ESWL alone, 1 primarily operation (tail pseudocyst resection) without medical treatment, 1 pancreatoduodenectomy after medical treatment and 10 no therapy. 80% of symptomatic patients had a history of alchohol intake, while 70% of asymptomatic patients had no such history.
There were no early complications such as bleeding, perforation and severe pancreatitis and no late complications ie. stent migration and re-stenosis of papilla.
At the first endoscopic treatment, a pancreatic stent (5 or 7Fr. Pig tail type) was placed (Figure 2 ), then 4 months and 10 months later it was removed and re-placed as necessary. 32 symptomatic cases became pain free, however another 3 calcified cases required treatments many times due to stone and pain relapsing. 1 case had an operation (PD) after medical treatment. There were no cases of cancer occurrence or death after treatment
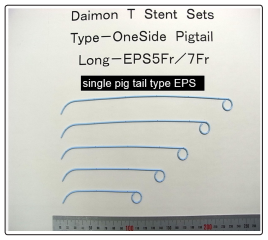
Figure 2: (5Fr.,7Fr.) 180mm,210mm,240mm,270mm,300mm
A Rendezvous pre-cut method: 12 cases (Figure 3)
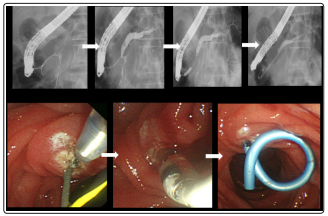
Figure 3: 56y/o m stenotic fusion I, pancreas stone- rendezvous precut method-EPS
Case 1 56-year old male. The guidewire, inserted through the major papilla, came out into the duodenum via the minor papilla. Along this guidewire, the minor papilla was cut by a needle type papillotome (KD-200Q-0721 Olympus) and the catheter was inserted into the minor papilla, then EPS was placed. This is our original procedure, a variant of the rendezvous method B Reverse Balloon Dilation Method: 3 cases (Figure 4,5)
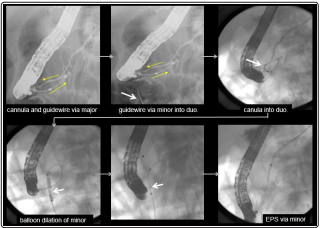
Figure 4: 13y/o f branch fusion III - rendezvous precut method+reverse balloon method
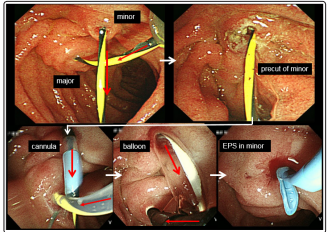
Figure 5: 13y/o f branch fusion III - rendezvous precut method+reverse balloon method
Case2 13-year old female: She entered into our hospital complaining of recurrent epigastralgia. The guidewire, inserted into the major papilla, came out via Wirsung’s duct, connecting branch, Santorini’s duct and minor papilla into the duodenum. The minor papilla was cut by needle type papillotome (rendezvous pre-cut method), then a balloon catheter was inserted along the guidewire and the minor papilla was dilated from the reverse direction by a 4mm dilation balloon, then EPS could be placed into the dorsal duct.
We had 3 cases combined with IPMN- in one case (dorsal main duct type IPMN), minor papilla-drainage orifice of mucin- located in the duodenal diverticulum. (Figure 6) Two young females were treated - one was case presentation 2 (below), and the other was a 13 y/o (branch fusion type III) combined with duodenal membranous occlusion.
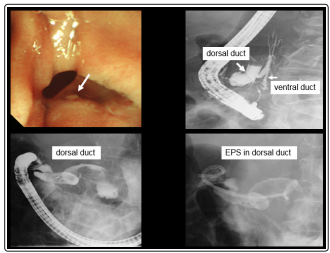
Figure 6: 78y/o f branch fusion III IPMN,minor in duodenal dive-EPS
In this paper, we classified 47 IPD cases by “modified Hirooka’s classification.” Within them, no branch fusion type II was seen , so we imagine some deviations in our diagnosis.
Like other authors, we suppose that congenital dysfunction of the minor papilla and acquired factors (alcohol intake,obesity) cause pancreatitis [2,3].
In early stage of CPD complete pancreatic divisum) and IPD medical conservative therapies are recommended [4-7]. Formally in the symptomatic stage, surgical therapy was performed. In these days, endoscopic therapy is preferable. In some reports, the therapeutic effects of surgery and endoscopy are almost equal, but in other reports the effect of the former is superior to that of the latter [8]. In many reports, patients of ARP stage had better results than in CH stage [9].
Recently, endoscopic procedures are the preferred choice for CPD and IPD therapies, with good results in our hospital. Cotton reported minor papilla sphincterotomy in CPD [10], and Jacob reported minor papilla sphincterotomy in CPD [11]. Since then many new techniques (wire-guided minor papilla sphincterotomy, pre cut method, needle knife cut method balloon dilation) were developed and good results were reported by many authors [12- 22]. New therapeutic procedures have also been recently reported by Chavan-; reverse sphincterotomy of the minor papilla, and by Everson ; reverse minor papilla balloon dilation without EPS [23,24].
From 2017, we have introduced and reported about new therapeutic procedures for the PD, IPD therapy: pre-cut method, balloon dilation method free-hand method, rendezvous method rendezvous pre-cut method and reverse balloon dilation method. The success rate of CPD and IPD via minor papilla was 97% (131/135) and 94% (33/36) respectively without severe complications [25-27]. However we had to exchange EPS many times and still now EPS is placed in 24 cases.
In this paper, we reported the safety and usefulness of our new treatment methods-rendezvous precut method and reverse balloon method. Guidewire assisted cut method precut method free hand method balloon dilation method and rendezvous method are also safe and useful endoscopic treatment for CPD and IPD.
