Author(s): Sabitha Challa
The association between Subclinical hypothyroidism and Depression is recognised. It is found that patients with Thyroid disorders are more prone to develop depressive symptoms and depression may be accompanied by various subtle thyroid abnormalities. The most commonly documented abnormalities are elevated T4 levels, Low T3, elevated rT3, a blunted TSH response to TSH, Positive anti thyroid autoantibodies and elevated CSF TRH concentrations. It is also found that thyroid hormone supplements appear to accelerate and enhance the clinical response to antidepressants. It is found out that Depression is associated with changes in Hypothalamic-pituitary axis as thyroid hormones act on the central nervous system. Mild thyroid dysfunction causes depression in younger patients (<60 years old) diagnosed by depressive scale. It was found that differences in age group may cause depressive episodes. Depressive episodes such as anxiety and the risk of committing suicide are considerable factors that differ according to the age of the individuals.SCH was found to be associated with depression in the younger adults (<60 years old). The only difference between SCH and normal thyroid function is TSH.In depressive disorder and subclinical hypothyroidism sex differences have also been recognised. Association between subclinical hypothyroidism and Depression is assessed by various depressive scores such as Beck Depression Inventory and Hamilton depression rating scale. As Subclinical hypothyroidism is associated with low mood, Serum levels of TSH, FT3, FT4 and Hamilton depression, treatment with Levothyroxine showed significant decrease is TSH levels and Hamilton scores were decreased. Since the prevalence of depressive symptoms in hypothyroidism is high TSH cut-off levels is used,TSH cut off value for hypothyroidism is based on associated symptoms,TSH cut-off value is 2.5 MIU/L is optimal.
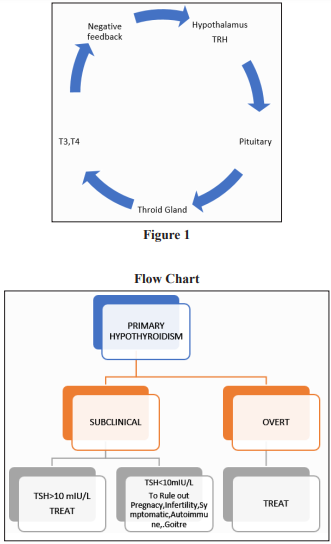
Subclinical hypothyroidism is defined as an increase in serum thyroid-stimulating hormone (TSH) level and Free Thyroxine (T4) being within normal limits It occurs due to two main reasons a) Primary gland failure b) Insufficient thyroid gland stimulation by the hypothalamus or pituitary gland [1]. Symptoms include dry skin, poor memory, fatigue, cold intolerance, constipation, and hoarseness [2]. It is diagnosed by Serum TSH levels and serum thyroid-stimulating hormone (TSH) levels range from 5.0-19.96 m IU/L and normal T4 Levels [3].Treatment is considered based on following factors a) Symptoms are present b) If there is goitre c) Risk of progression to Overt Hypothyroidism and risks of CHD d) TSH levels >10 m IU/L [4]. Individuals are at risk of developing Cardiovascular manifestations, Hypercholesterolemia, Cognitive decline and dementia and decreased GFR.
In Individuals with subclinical hypothyroidism the goal of therapy is to bring Serum Thyrotrophic to normal levels. Levothyroxine is the treatment of choice. Since the degree of thyroid dysfunction is mild, small (25-75 μg) doses of levothyroxine are sufficient to restore normal serum thyrotrophic levels in the majority of individuals. Serum thyrotrophic levels should be checked every 6 weeks after initiating the medication. Once the levels become normal, annual thyroid screening should be done [5].
Depression is most common psychiatric disorder and an important factor that affects all age groups all over the world [6]. The prevalence of depression is in the range of 10% to 15% worldwide both in developed and developing countries. Depression impairs both cognitive and social functioning. The Path physiology of depression may result from deficiency of neurotransmitter in brain regions such as abnormalities in serotonin, nor epinephrine, dopamine, GABA, Peptide neurotransmitters or tropic factors such as brain derived neutrophic factor, somatostatin, Thyroid related hormones and neurotransmitter such as acetylcholine and Corticotropin releasing factor and substance P are thought to cause depression.
Depression is associated with increased rates of suicidal behaviour and mortality. The symptoms of include depressed mood, loss of interest or pleasure, decreased energy and fatigue, reduced concentration and attention, reduced self-esteem and selfconfidence, ideas of guilt and unworthiness, bleak and pessimistic views of the future, ideas or acts of self-harm or suicide, disturbed sleep and diminished appetite [7].
The management of depression can be broadly be classified into antidepressants, electroconvulsive therapy (ECT) and psychosocial interventions. The selection of antidepressant medications is based on patient specific and drug specific factors such as Patient preference, previous side effects with medications, Drug tolerability and drug interactions. Because of the side effect and safety profile, selective serotonin reuptake inhibitors (SSRIs) are considered to be the first line antidepressants. Other preferred options include tricyclic antidepressants, mirtazapine, bupropion, and venlafaxine. The medications must be started in the lower doses and the doses must be titrated, depending on the response and the side effects experienced. Psychotherapeutic approaches is an important factor that may be considered in the decision to use psychotherapy as the initial treatment modality. Cognitive behavioural therapy (CBT) and interpersonal therapy are the psychotherapeutic approaches that have the best efficacy in the management of depression [8].
There is association between Subclinical hypothyroidism and depression-Since brain is the main target for thyroid hormone overt hypothyroidism can cause symptoms related to relate to depression. It was found out that patients with depression are found to have slightly elevated TSH levels and thus have depressed symptoms due to abnormalities in thyroid hormone levels. Patients treated with L4 are found to have reduced depressive symptoms after there is decrease in thyroid stimulating hormone, depressive symptoms reduce [9].
It is found that mild thyroid dysfunction is related causes depression in younger patients (<60 years old) diagnosed by depressive scale. It was found that differences in age group may cause depressive episodes. Depressive episodes such as anxiety and the risk of committing suicide are considerable factors that differ according to the age of the individuals.SCH was found to be associated with depression in the younger adults (<60 years old). The only difference between SCH and normal thyroid function is TSH [10].
Studies showed that there is increased prevalence of depression in adults associated with SCH, compared with euthyroid individuals. So proper clinical practice can improve the clinical practice and improve the quality of life in patients. The association between mood disorder and changes in HPT axis has been recognised. In the CNS, alternations in hormone levels causes neuropsychiatric disturbances and thus affecting HPT axis and thus explain the association between SCH and Depression. Studies have reported that reduction in somatostatin Levels in cerebrospinal fluid, leading to increased TSH levels among individuals with depression. In individuals with depression serotonin deficiency is also seen, which causes changes in HPT axis. All these together SCH and Depression share common mechanisms. Depression is reported among age group of 35-45 years .It has become increasingly common among elderly as normal aging itself associated with changes with HPT axis. Since the secretion of thyroid hormones is reduced with increasing in age, with a lower FT3 levels but a relatively unchanged FT4 concentration. When compared with younger population higher TSH level is seen in the elderly due to reduced FT4 degradation and its peripheral conversion to FT3, with subsequent positive feedback to the HPT axis.
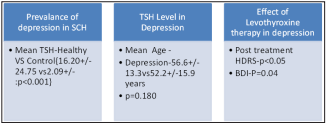
In this analysis, old patients with SCH compared with healthy individuals (p=0.020).TSH was found out to be significantly higher compared to healthy controls (p<001).It was found out in studies that there is higher prevalence of depression in individuals with SCH compared to healthy controls. In Five studies depression scores were found to be higher in SCH individuals than healthy controls. In a pooled analysis, individuals with SCH has higher risk of depression compared with euthyroid state.
Analysis showed that relation of SCH association is more common in younger individuals with odds ratio of 1.75(p=0.020).In another analysis, it showed that there is prevalence of subclinical hypothyroidism is higher in depressed individuals (p<0.001). In another analysis, study done in a sub sample of patients with depression, it showed that there is prevalence of subclinical hypothyroidism was likewise higher in depressed adolescents (p<0.001).
In a study in hospitalised patients with DD, depression scale used is (Hamilton depression rating scale), the prevalence of SCH was 11.8%.The prevalence of SCH in female depressed patients is approximately two times than that of male patients (p<0.05).In an correlation analysis it showed that thyroid stimulating hormone levels were associated with BMI, Total cholesterol levels, low density lipoprotein cholesterol levels.
In a study population of 174 hypothyroid patients, composed of individuals under the treatment with Levothyroxine (age: 19-68 years).The individuals were evaluated in terms of depression by BDI. Based on questionnaire, scores below 10 were considered normal, while scores above 10 is indicative of depression. The findings revealed, 116 subjects were depressed, 58 were healthy. The mean for T4 and T3 8.3 pg/dl and 1.2 ng/ml and TSH cut off is 2.5mU/L. It showed 89.66 sensitivity and 87.93 specificity. Then among patients with severe depression (BDI>19) different cut off were determined and compared based on severe depression and finalised the optimal TSH cut off is 4 m U/L with respect to depressive individuals.
TSH serum levels were measured in 43 individuals range (reference values: 0.25-5.00 lIU/ml) FT4 serum concentrations were measured in 42 patient’s .One individual had elevated FT4 level of 20.25 pmol/l with normal TSH and FT3. Seven individuals were under the lower limit of FT4 reference values. 35 patients were within the normal limits. FT3 was assessed in 43 patients.13 patients were below the norm; 30 patients were in norm. It was noticed that among 30 patients having theirs FT3 within the norm.
Depression was assessed by using CGIs and HDRS.FT3 levels done during admission were positively correlated with clinical improvement assessed with CGI.There was no association with HDRS.FT4 levels were positively correlated with clinical improvement with HDRS.
In a retrospective cohort study done showed individuals with high TSH levels has increased risk of depression (<0.001). In another analysis done individuals having below normal TSH levels, can also be indicative of subclinical hypothyroidism.
In studies done, association between mood disorders and changes in HPT axis has been observed. In the brain due to alterations in hormone levels changes in hormone levels such somatostatin and serotonin can result in neuropsychiatric disturbances. Thus these disturbances affect HPT axis and thus explain the association between SCH and depression. Several studies reported a reduction in the Somatostatin level in cerebrospinal fluid, leading to increased TSH level among individuals with depression. Serotonin deficiency, which is also commonly seen in those with depression, has been observed to cause alterations in the HPT axis. So taken together, SCH and depression may share common bio- logical mechanisms, which is in support of our findings.
Analysis showed 266 individuals treated with L-Thyroxine therapy showed improvement in depressive symptoms (p<0.001). If TSH>10 treatment should be given with L-Thyroxine showed improvement in depressive symptoms. The duration of treatment is 2-12 months. In one individual depressive symptoms improved.3 studies showed decrease in depression scores. In a randomised double -blind placebo controlled study, study is done in individuals with Subclinical hypothyroidism. Beck depression scale was used for all these individuals and assessed .Both intervention and control groups received Levothyroxine and placebo for 12 weeks. At the end of the 12 weeks it showed decrease in sub scale in individuals in the intervention group assessed by Beck depression scale.
In a study done in individuals, serum TSH, FT3 and FT4 levels were measured and HAM-D rating scale was used. Individuals underwent treatment with Levothyroxine for 2 months. Treatment with Levothyroxine resulted in a decrease in Serum TSH levels and Hamilton scores (p=0.00).
| Author | Year | Study design | Location | Sample size | Outcome | |
| 1) | T.Zhao [11] | 2020 | N/A | China | 1787 | Prevalence of SCH was 11.8%.It was more prevalent in female patients compared to male patients |
| 2) | Huai Heng Loh [12] | 2018 | SystematicReview | Malaysia | 12,315 | It was found out that elderly patients with SCH had 1.7 higher folder of depression compared to healthy individuals |
| 3) | Raphael Hirtz[13] | 2019 | Cross sectional study | German | 360 | It was found out that the prevalence of subclinical hypothyroidism is higher in depressed adolescents |
| 4) | A Talaei [14] | 2016 | Cross Sectional study | Iran | 174 | It is found out that patients with TSH of 4 MU/L has increased prevalence of depression |
| 5) | Dominika Berent [15] | 2013 | N/A | Poland | 43 | Lower FT3 levels was seen in patient with depression. It was observed that High FT4 was associated with severe depression |
| 6) | Eun Young kim [16] | 2014 | Retrospectivecohort study | Korea | 13,017 | Depressive symptoms were in increased individuals with higher TSH levels in females more than males. |
| 7) | Andrei Costache [17] | 2020 | Cohort study | Romania | 96 | In patients with depression out 96 patients 7 patients were found to have subclinical hypothyroidism with Low TSH levels with normal T4 levels. |
| 8) | Marco Medici[18] | 2013 | Cross sectional study | Netherlands | 1503 | This study showed that elderly patients with Low normal TSH levels are at increased risk of developing depression |
| 9) | Mirella P.Hage[19] | 2011 | N/A | Lebanon | - | It is observed that patients with thyroid abnormalities are more prone to develop depression and vice versa. |
| 10 | Lazily Najafi[20] | 2013 | Randomisedcontrolled clinical trial | - | 60 | In patients with subclinical hypothyroidism treatment with Levothyroxine showed improvement in depressive symptoms. |
| 11 | Gaurav Vishnoi [21] | 2013 | N/A | India | 300 | It was observed that treatment with Levothyroxine showed decrease in TSH levels and Hamilton scores. |
| 12 | Lea Wildisen [22] | 2020 | Randomisedcontrolled clinical trial | Switzerland | 427 | The mean (SD)GDS-15 score was 1.39 for Levothyroxine group and placebo group with an adjusted between group difference of 0.15. |
The above Table-1 shows Characteristics of included studies
This analysis has some limitations, such as 1) most of the studies dome were observational studies such as cross sectional studies 2) There were moderate studies done showing association between subclinical hypothyroidism and depression and probable bias were present in selection of articles heterogeneity, confounding factors and publication bias. 3)There may have been probable bias existed in terms of Diagnosis of SCH based on TSH and depression and depressive symptoms based on depression scales.4)All these studies done doesn’t have proper criteria based on age ,gender criteria and its diagnosis is dependent only on TSH levels which misleads to diagnosis.
Despite of these limitations, the current analysis showed that the prevalence of SCH with depression is seen in women more than men. Proper diagnosis and treatment with L-Thyroxine has improved the outcome. Other than TSH measurements some studies showed Low FT3 is also useful in diagnosis of SCH with depression. The prevalence of SCH with depression is more common in young age.
Overall the studies indicates that all individuals with SCH doesn’t develop depression. Diagnosis should have differences ranges of TSH levels according to age to diagnose SCH and can help for better evaluation of depression.
From studies conducted, it is better to do routine screening among individuals with SCH especially among elderly to prevent morbidity and mortality. The use of Levothyroxine therapy among people with depression need to be considered carefully on individual basis, weighing risks and benefits of the treatment .More studies should be done to gain more insights of the pathogenesis and natural history of depression in SCH.The efficacy and safety of levothyroxine to improve mood disorders among high risk individuals. Studies show that prevalence of SCH is more common among female hospitalised patients with depression is approximately two times more common than male patients. Risk factors include recurrent hospitalisation and high BMI in female depressed patients. So proper screening of TFT should be done in female patients with Depressive disorder in future in female inpatients.
SCH increases the risk of developing depression, so L-Thyroxine replacement therapy helps to resolve depressive disorder if TSH is >10mIU/L in SCH patients.
Severe SCH causes severe depressive symptoms in older age, so proper evaluation and treatment should be given.
Subclinical hypothyroidism is associated with depression as thyroid hormones act on central nervous system and these changes causes neuropsychiatric disturbances thus affecting HPT axis. So proper screening should be done to prevent morbidity and mortality.
Proper screening of TFT should be done in female inpatients who are at risk in future studies. Elderly persons with Low normal TSH levels are at risk of developing depressive syndrome.so elderly patients with Low TSH should be screened properly for depressive syndrome.