Author(s): Sabina Khan* and Christianeh Edema
Objective: This study comprehensively investigates the experiences and perceptions of occupational therapy practitioners (OTPs) regarding virtual care for neurological conditions, with a particular focus on patient-centered practice and interprofessional collaboration.
Methods: A mixed-methods survey involving 170 OTPs specializing in neurological conditions was conducted to gather data. Quantitative data were analyzed to calculate percentages and statistics, while qualitative data were subjected to thematic analysis to gain insights into the practitioners’ perspectives.
Results: The study found that 72% of OTPs expressed comfort with performing virtual assessments, and 70% felt comfortable with virtual treatments. However, there were variations in comfort levels, particularly concerning assessments in the adult neurological population, with only 20% feeling comfortable in this context. Video conferencing was the most widely adopted virtual care platform (65%), followed by electronic health records (48%) and mobile apps (30%). The survey revealed that OTPs provided a range of services virtually, including psychosocial support (62%) therapeutic exercise and activities (78%), and patient/ caregiver education (60%). OTPs working with pediatric populations reported a higher perceived value in telehealth services (76%) compared to those working with adult populations (61%). Key facilitators to promote usage of telehealth with neurological conditions included telehealth-specific training programs, digital assessment tools, interprofessional collaboration, and patient engagement strategies. Barriers included training gaps, especially in adult neurological assessments.
Conclusion: This study highlights the evolving role of occupational therapy in the realm of virtual care for neurological conditions. While the majority of practitioners recognize the importance of virtual care, tailored training and support programs are needed to address variations in comfort levels, particularly in assessments for adult neurological patients. Interprofessional collaboration is crucial for enhancing patient care. The study provides valuable insights for practitioners, educators, and healthcare institutions to optimize virtual care in the digital age.
The field of healthcare has undergone a profound transformation with the integration of digital technology, revolutionizing the delivery and experience of healthcare services. Among the notable developments in this landscape is the emergence of telehealth, characterized by the use of digital platforms to deliver healthcare services, which has gained increasing prominence in recent years [1]. This transformative shift has had a significant impact on various healthcare domains, and one field that has particularly embraced this change is occupational therapy.
Occupational therapy practitioners (OTPs) have increasingly turned to virtual care as a means to address the diverse needs of their patients, especially those facing neurological conditions [1]. The adoption of telehealth in occupational therapy gained further momentum due to the global COVID-19 pandemic, where physical distancing measures necessitated the use of telehealth technologies to ensure continued patient care [2]. OTPs swiftly adapted to these digital solutions to provide essential care and support to individuals with neurological conditions, emphasizing the importance of patient-centered practice and interprofessional collaboration in this virtual care environment.
However, amidst this rapid evolution of healthcare delivery, critical questions have arisen. One such question pertains to the confidence and competence of OTPs when conducting virtual assessments and interventions for patients with neurological conditions. The proficiency of OTPs in utilizing digital technology for assessments is pivotal in ensuring the quality and effectiveness of virtual care [3]. Bridging this confidence gap is imperative, as it holds profound implications for patient outcomes and the overall success of virtual care initiatives.
Additionally, a significant gap exists in the literature concerning the effectiveness of interprofessional collaboration in the context of virtual care for patients with neurological conditions. While the benefits of collaboration in enhancing patient care are well- documented there is a notable lack of studies exploring the dynamics and impact of interprofessional collaboration in the virtual care setting. Understanding how OTPs collaborate with other healthcare professionals and the role of digital technology in facilitating this collaboration is of paramount importance [4]. This study is conceived to comprehensively address these gaps in the literature. Through a mixed-methods survey, we aim to capture quantitative data on demographic and practice-related aspects. Furthermore, we seek to explore the perceptions of OTPs regarding the importance of virtual care, their comfort levels in utilizing digital platforms for assessments and interventions, and the effectiveness of interprofessional collaboration in the virtual care setting. Qualitative insights will be gathered through open- ended questions, providing OTPs with the opportunity to share their experiences, challenges, and recommendations.
By shedding light on the intricate relationship between occupational therapy practice, digital technology, and interprofessional collaboration, this study endeavors to provide critical insights. These insights will not only inform best practices and enhance training programs but will also contribute to the growing body of evidence surrounding virtual care for individuals with neurological conditions. Ultimately, our research aims to elevate the quality of care provided to patients while addressing the pressing need for a comprehensive understanding of the dynamics of interprofessional collaboration in the continually evolving landscape of virtual care.
In light of these developments, this study sets out to comprehensively address several key aims and objectives. Firstly, we aim to investigate OTPs’ comfort levels in utilizing virtual care platforms, with a particular focus on virtual assessments and treatments for neurological conditions. Secondly, we seek to identify specific areas where OTPs may face challenges or training gaps in delivering virtual care, especially in the context of adult neurological assessments. Thirdly, our study aims to understand how OTPs perceive the value of virtual care, including variations in perceived value across different patient populations, such as pediatrics and adults. Additionally, we will explore the virtual care platforms commonly used by OTPs and the range of services they provide virtually to individuals with neurological conditions. Furthermore, this study delves into the dynamics of interprofessional collaboration within virtual care teams, with a focus on how OTPs collaborate with other healthcare professionals. Lastly, we aim to highlight the barriers and facilitators OTPs encounter when providing virtual care, shedding light on the factors that hinder or enhance the quality of virtual care delivery. Through these aims and objectives, our study aspires to contribute to a deeper understanding of occupational therapy practice in the digital age and offer valuable insights for optimizing virtual care for individuals with neurological conditions.
This study employed a mixed-method survey design to investigate occupational therapy practitioners’ (OTPs) experiences providing virtual care to individuals with neurological conditions. The study aimed to capture both quantitative and qualitative data to comprehensively explore the dynamics of virtual care delivery and its impact on patient-centered practice and interprofessional collaboration. Prior to commencing the survey, a power analysis was conducted to estimate the required sample size for adequate statistical power. Based on this analysis, a minimum of 185 participants were determined to be needed to achieve a sufficient level of statistical power for the study’s objectives. To account for potential non-response and ensure robust findings, we initially aimed to recruit 200 participants. However, once the target of 200 completed responses was achieved, further survey invitations were not extended. During the survey period, it was observed that 15% of the invited participants did not complete the survey. Therefore, the final sample size for this study consisted of 170 participants who completed the survey in its entirety. Ethical approval for this study was obtained from the University of St. Augustine Institutional Review Board (IRB) review board. Informed consent was obtained from all participants at the outset of the survey. A comprehensive consent form was presented on the first page of the survey instrument, outlining the study’s objectives, the voluntary nature of participation, and the assurance of confidentiality. Participants were required to provide explicit consent by acknowledging their agreement before proceeding with the survey.
The statistical analysis conducted in this study aimed to explore and understand various aspects related to the occupational therapy practitioners’ (OTPs) experiences in providing virtual care to patients with neurological conditions. The analysis involved both descriptive and inferential statistics to uncover meaningful patterns and associations within the data.
Descriptive statistics were employed to provide a comprehensive summary of key demographic variables. This included the calculation of central tendencies such as mean and measures of variability like standard deviation for continuous variables like age and formal education. Descriptive statistics helped in characterizing the study participants and provided insights into the composition of the sample.
Inferential statistics were employed to examine associations within the dataset and to test hypotheses related to the study objectives. The chi-square test was utilized to explore relationships between categorical variables. For instance, it was used to assess associations between demographic characteristics (e.g., age and formal education) and categorical outcomes related to virtual care perceptions and interprofessional collaboration. The chi- square test allowed for the identification of statistically significant relationships. In cases where cell counts were small, Fisher’s exact test was applied as an alternative to the chi-square test. This test was particularly useful when analyzing categorical variables with limited sample sizes, ensuring robust statistical analysis.
To delve deeper into the factors influencing specific outcomes related to virtual care perceptions and interprofessional collaboration, hierarchical binary logistic regression analyses were conducted. This advanced statistical approach allowed for the examination of how various predictor variables, including demographic characteristics, influenced the likelihood of certain attitudes and behaviors. The results of these analyses provided valuable insights into which variables acted as statistically significant predictors, thus contributing to a nuanced understanding of the data. Data were considered statistically significant when p-values were less than 0.05 (p < 0.05). This significance level was chosen to indicate that observed associations between variables were unlikely to occur by chance and were deemed meaningful in the context of the study. Statistical significance was used as a threshold for drawing meaningful conclusions from the data.
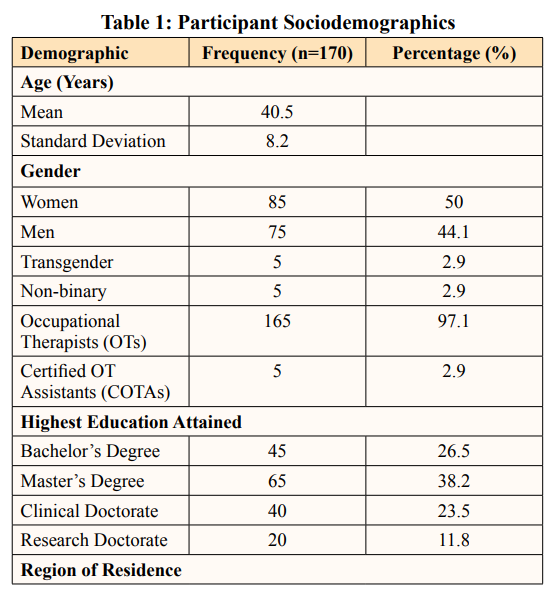
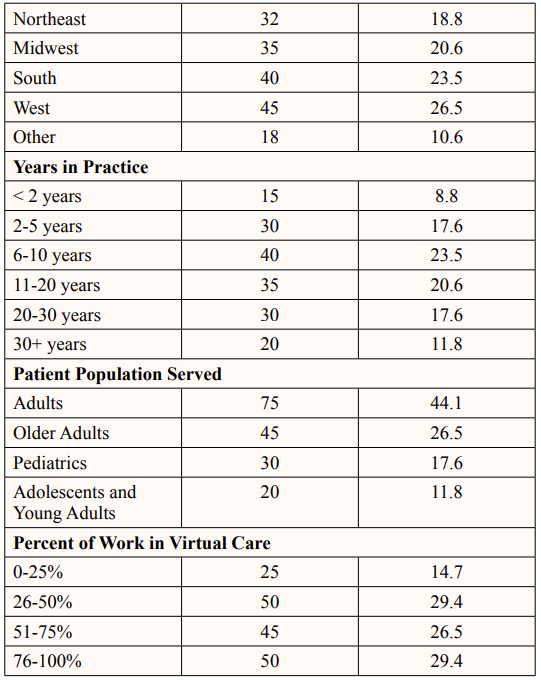
Table 1 shows the sociodemographic characteristics of the 170 occupational therapy practitioners (OTPs) who participated in this study. The participants in this study represent a wide range of age groups between 18 and 65 with an average age of 40.5 years +/- 8.2 years. This diversity in age underlines the inclusivity of our sample and its representation across different career stages. Gender distribution among the participants is well- balanced, with half identifying as women (50%), slightly less than half as men (44.1%). A small percentage of participants identify as transgender (2.9%) or non-binary (2.9%). This balanced representation highlights the gender diversity within the occupational therapy profession. When it comes to education, the participants have various levels of attainment. Approximately 26.5% practice with a bachelors degree, 38.2% have a masters degree, 23.5% have a clinical doctorate (OTD), and 11.8% have a research doctorate (Ph.D or Ed.D.). The study sample includes OTPs from various regions, with a majority residing in the west region of U.S.A (26.5%), followed by the south region of U.S.A (23.5%) and Midwest (20.6%). This regional distribution showcases the reach and engagement of virtual care practices across different geographical areas. Respondents displayed varying years of experience as OTPs, with most practicing 6-10 years. Most respondents reported working primarily with adults (44%), followed by older adults (26.5%), pediatrics (17.6%), and others with adolescents and young adults (15-39 years of age) (11.8%). Majority of respondents reported utilizing 26-50% of their job involved virtual care (29.4%) or 76-100% of their job (29.4%). Occupational therapy practitioners employed a variety of virtual care platforms in their practice, including telephone, email/messaging, video conferencing, remote patient monitoring, electronic health records, mobile apps, texting, and patient portals. The use of multiple platforms demonstrates the versatility of virtual care in meeting diverse patient needs. Respondents offered a range of services via virtual means, including psychosocial support, therapeutic exercise and/or therapeutic activities, patient/caregiver education, self-care training, neuromuscular education, screening, assessments, follow-up assessments, and initial evaluations. This breadth of services underscores the comprehensive care provided through virtual platforms.
Virtual care platforms played a central role in connecting OTPs with their patients. Video conferencing emerged as the most commonly utilized platform, with 65% of respondents reporting its use. Electronic Health Records (EHRs) were incorporated by 48% of participants to streamline documentation, while 30% embraced mobile apps designed for occupational therapy, catering to various aspects of care.
Occupational therapy services provided through virtual means encompassed a wide range, including psychosocial support (62%), therapeutic exercise and activities (78%), patient/caregiver education (60%), self-care training (42%), neuromuscular education (28%), screenings and assessments (35%), and follow- up assessments and initial evaluations (40%). This diversity underscores the adaptability of virtual platforms in facilitating occupational therapy interventions.
Most participants expressed comfort with performing virtual assessments (72%) and treatments (70%). However, comfort levels varied across areas of practice. Notably, some OTPs reported reservations, particularly when it came to assessments in the adult neurological population (20%).
To explore potential relationships, statistical analyses were conducted. Chi-square tests were employed to examine the association between demographic variables and comfort levels in providing virtual care to neurological patients. Results revealed a significant association between the highest level of education and comfort with virtual assessment (X 2 = [10.52], p = [.001]).
Further analysis indicated that OTPs with doctoral-level education expressed higher comfort levels than OTPs with masters or bachelors-level education.
The survey also sought to understand whether occupational therapy practitioners working with different populations perceived varying values in virtual care. OTPs working with pediatric populations reported a higher perceived value in telehealth services compared to those working with adult populations. Specifically, 76% of OTPs specializing in pediatrics considered virtual care highly valuable, whereas 61% of OTPs focusing on adults shared the same perspective.
Thematic analysis of open-ended responses revealed several notable barriers that occupational therapy practitioners (OTPs) encounter when providing virtual care to neurological patients, particularly in the adult population. One recurring theme highlighted the inadequacy of training and support provided by their places of employment. Specifically, many OTPs expressed concerns regarding the lack of specialized training for adult neuro patients in the virtual care context. OTPs identified assessments where they felt less competent due to training gaps (See Table 2).
These barriers stress the need for comprehensive training programs that address the unique challenges posed by virtual care for adult neurological patients
Conversely, participants also identified key facilitators that enhance their ability to provide virtual care effectively. Themes that emerged from the analysis included telehealth training programs and digital assessment tools. OTPs emphasized the value of telehealth-specific training programs, such as those offering guidance on adapting assessments like the Dynamic Gait Index (DGI), Digit Span Test, and Motor-Free Visual Perception Test (MVPT) to virtual platforms. These programs equip OTPs with the necessary skills and confidence to navigate virtual assessments effectively. The use of digital assessment tools designed for virtual care settings was highlighted as a significant facilitator. These tools help streamline assessments and improve the accuracy of results. OTPs appreciated the convenience and enhanced functionality of digital assessment tools, making the assessment process smoother and more reliable in the virtual realm. Collaborative efforts with other healthcare professionals emerged as a facilitator in virtual care provision. OTPs found that working closely with colleagues from different disciplines, such as physical therapists, speech therapists, and physicians, facilitated comprehensive patient care. The interdisciplinary approach ensured a holistic evaluation of patients’ needs and enhanced the overall quality of care. Lastly, OTPs recognized the importance of patient engagement and education as a facilitator. They highlighted the role of patient education materials and interactive exercises that could be shared digitally. These resources empowered patients to take an active role in their rehabilitation, promoting better outcomes and adherence to therapy plans.
The integration of virtual care into occupational therapy practice represents a transformative shift in healthcare delivery. Our findings provide valuable insights into OTPs experiences with virtual care and highlight both opportunities and challenges within this evolving landscape.
Our study revealed that OTPs have embraced virtual care platforms, with video conferencing as the most used tools. This aligns with previous research emphasizing the effectiveness of video-based telehealth for occupational therapy interventions. Moreover, OTPs offered a broad range of services virtually, addressing various aspects of patient care. This versatility underscores the potential of virtual care to provide comprehensive support to individuals with neurological conditions. The diverse landscape of virtual care platforms utilized by OTPs reflects the flexibility of this emerging practice. Most OTPs reported using video conferencing platforms, such as Zoom or Microsoft Teams, for virtual sessions. Video conferencing facilitated face-to-face interactions, enabling real-time demonstrations of therapeutic exercises and fostering engagement with patients. Services such as psychosocial support, therapeutic exercises, and patient education were commonly provided via virtual means. This versatility emphasizes the potential of virtual care to address various aspects of patient care.
Despite the overall recognition of the importance of virtual care, our study uncovered nuances in OTPs’ comfort levels in conducting virtual assessments and treatments. Interestingly, a significant percentage expressed comfort with their ability to perform virtual assessments. However, this comfort level varied across specific areas.
Our findings indicated that OTPs treating pediatric patients generally felt more comfortable performing virtual assessments compared to those working with adults. This discrepancy may be attributed to several factors. Pediatric assessments often involve interactive and play-based activities, which can be adapted effectively to virtual platforms. In contrast, assessments for adults with neurological conditions may require more complex physical evaluations, making virtual administration more challenging.
The variations in comfort levels among OTPs underscore the importance of tailored training and support programs. While OTPs treating pediatric patients may adapt to virtual care more seamlessly, their counterparts working with adults may require additional training and resources to address the specific challenges associated with neurological assessments. This finding highlights the need for occupational therapy education programs and healthcare institutions to prioritize training and support for adult neuro patients in virtual care contexts.
Interprofessional collaboration emerged as a key facilitator in virtual care provision. OTPs recognized the value of working closely with colleagues from different disciplines, including physical therapists, speech therapists, and physicians. This collaborative approach ensured a holistic evaluation of patients’ needs and enhanced the overall quality of care. Nevertheless, OTPs expressed reservations about shared decision-making within virtual care teams. Some OTPs cited challenges in advocating for patients’ interests when others did not prioritize the patient’s best interest. Effective communication frameworks and shared decision-making strategies are essential to address these challenges and optimize interprofessional collaboration.
Thematic analysis revealed barriers and facilitators in virtual care provision. Barriers included training gaps, particularly in adult neurological assessments. Comprehensive training programs that address these challenges are essential to enhance OTPs’ confidence and competence in virtual assessments. On the other hand, facilitators encompassed telehealth-specific training programs and digital assessment tools, both of which streamline assessments and improve accuracy. Interprofessional collaboration and patient engagement strategies were also highlighted as facilitators.
While this study offers valuable insights into occupational therapy practitioners’ (OTPs) experiences with virtual care for neurological conditions, there are several limitations to consider. First, the survey data relied on self-report, which may introduce response bias. Participants may have provided socially desirable responses or subjective opinions. Additionally, the study’s cross-sectional design limits the ability to establish causality or observe long-term trends. The survey’s reliance on a convenience sample of OTPs specializing in neurological conditions may not fully represent the diversity of the occupational therapy profession. Moreover, the study was conducted within the context of the COVID-19 pandemic, which may have influenced OTPs’ attitudes and practices regarding virtual care. Lastly, while the study aimed to investigate interprofessional collaboration, it primarily focused on OTPs’ perspectives, and a more comprehensive examination involving other healthcare professionals is needed to provide a complete picture.
In conclusion, this study sheds light on the evolving landscape of occupational therapy practice in the digital age, particularly in the context of providing virtual care to individuals with neurological conditions. The findings highlight the significant role of virtual care in contemporary occupational therapy, with the majority of practitioners recognizing its importance. However, comfort levels with virtual assessments and treatments vary, highlighting the need for tailored training and support programs, especially for those working with adult neurological patients.
Interprofessional collaboration emerges as both a facilitator and a challenge, emphasizing the need for effective communication and shared decision-making frameworks within virtual care teams. Barriers related to inadequate training and the discomfort associated with specific assessments call for comprehensive training modules and investment in digital assessment tools. As the field of occupational therapy continues to adapt to emerging technologies, these findings provide valuable insights for practitioners, educators, and healthcare institutions, guiding efforts to ensure the provision of patient-centered, high-quality care to individuals with neurological conditions in the digital age. While this study contributes to the growing body of knowledge in virtual care, further research is needed to explore the long-term effects of virtual care and the perspectives of a broader range of healthcare professionals involved in neurological rehabilitation [5-7].
The authors would like to thank all participants and others who were involved in reviewing this manuscript.
This research is approved by The University of St. Augustine IRB committee.
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
This research was conducted without the use of external funding or financial support.
1.Hoel V, Von Zweck C, Ledgerd R (2021) World Federation of Occupational Therapists Was a global pandemic needed to adopt the use of telehealth in occupational therapy?. Work (Reading, Mass.) 68: 13-20.
2.Abbott-Gaffney CR, Gafni-Lachter L, Cason J, Sheaffer K, Harasink R, et al. (2022) Toward successful future use of telehealth in occupational therapy practice: What the COVID-19 rapid shift revealed. Work (Reading, Mass.) 71: 385-394.
3.Taylor S, Souza S, Little L, Odiaga J (2023) Enhancing Telehealth Competency: Development and Evaluation of Education Modules for Older Adults. OTJR: occupation, participation and health 43: 478-486.
4.Bosch B, Mansell H (2015) Interprofessional collaboration in health care: Lessons to be learned from competitive sports. Canadian pharmacists journal: CPJ = Revue des pharmaciens du Canada: RPC 148: 176-179.
5.Busari JO, Moll FM, Duits A J (2017) Understanding the impact of interprofessional collaboration on the quality of care: a case report from a small-scale resource limited health care environment. Journal of multidisciplinary healthcare 10: 227-234.
6.Franz S, Muser J, Thielhorn U, Wallesch CW, Behrens J (2020) Inter-professional communication and interaction in the neurological rehabilitation team: a literature review. Disability and rehabilitation 42: 1607-1615.
7.Sánchez-Guarnido AJ, Domínguez-Macías E, Garrido- Cervera JA, González-
8.Casares R, Marí-Boned S, et al. (2021) Occupational Therapy in Mental Health via Telehealth during the COVID- 19Pandemic. International journal of environmental research and public health 18: 7138.
View PDF