Author(s): Erika Gayle C Ty*, Tanya Patricia T Allas, Kyla Janika M Nerva, Janella S Mercado Garcia, Athena Emmanuelle M Parro, Ma Criselda C Valerio, Vilma O Pelino and Ana Aurelia M Santos
Male pattern androgenetic alopecia is a chronic, progressive condition with significant social and psychological impact. Few preliminary researches have been done on the role of low-level laser therapy as a treatment modality for male pattern hair loss. This is a randomized, controlled, single-observer blinded clinical trial conducted from November 2019 to October 2021 at the East Avenue Medical Center Dermatology Out-Patient Department on the use of low-level laser therapy and topical minoxidil for the treatment of androgenetic alopecia. Twenty-four male adults with Norwood Hamilton Hair Loss Scale of IIa to V were randomly assigned into 2 groups: a control group (monotherapy with topical minoxidil 5%) and a treatment group (678 nm helmet-type low-level laser therapy and topical minoxidil 5%). A statistically significant higher increase in hair density was observed in the treatment group (14.58 and 15.08 for the right and left sides, respectively) compared to the control (5.83 on the right and 5.50 on the left, respectively, p=.000 <.05). In addition, the investigator’s global photographic assessment and patient satisfaction were also significantly higher. Both treatments were well tolerated. The results of this study show that 678 nm helmet-type low-level laser therapy is an effective adjunctive treatment modality to topical minoxidil 5% solution for the treatment of male androgenetic alopecia.
Male pattern androgenetic alopecia is the most common hair disorder in males affecting 60-70% of the population worldwide. It is a chronic, progressive condition with significant social and psychological impact and the treatment remains challenging. At present, there are only two scientifically proven therapeutic agents approved for this disorder: topical minoxidil and oral finasteride. These medical therapies require indefinite use and limitations include cost, potential side effects and patient adherence. Low-level laser therapy is a relatively new non-invasive therapeutic option for male androgenetic alopecia with long-term cost-effectiveness and has a potential to be used with ease in a home-setting. Preliminary research indicates that low-level laser therapy may be effective as an adjuvant therapy to minoxidil and finasteride and may also show promise as a primary treatment option. However, more research needs to be undertaken to evaluate low-level laser therapy against or in combination with current standard therapies for pattern hair loss. Guidelines for parameters such as optimal wavelength, fluence, pulse structure, power density, time, number of treatment sessions as well as its efficacy on different populations are yet to be established. By determining the efficacy of low-level laser therapy as an adjunct to topical minoxidil, this study can be used as evidence for using low level laser technology as a promising adjunct for patients who do not respond to either finasteride or minoxidil alone, and for those who do not want to undergo hair transplantation.
Androgenetic alopecia remains to be one of the most distressful and prevalent dermatological problems affecting men and women alike. It occurs in up to 73% of the Asian population with increasing age and familial history of baldness as strong risk factors. It is this hyperandrogenism that perhaps plays a central role in the development of alopecia. It is presumed that androgen dependent traits that predispose patients to developing alopecia are controlled by several genes, and several polymorphisms have already been published in the literature. Dihydrotestosterone is hypothesized to co-mediate three processes that play direct roles in the progression of alopecia - sheath thickening, perifollicular fibrosis, and calcification. The two drugs that have been used for treatment of alopecia are minoxidil and finasteride. Finasteride, a 5α-reductase inhibitor used in alopecia therapy, may lead to cessation of progression of the disease. Similarly, minoxidil, an FDA-approved hair growth stimulant, is purported to decrease androgen-related functions and increase blood flow in alopecic patches. However, not all patients respond to these drugs and its indefinite use renders these drugs susceptible to loss of compliance. In a large-scale study of 1495 minoxidil users, only around 38.4% of patients experienced some hair growth; almost two-thirds of them voluntarily discontinued therapy in a span of one year, citing “low effect”. Finasteride, despite efficacy in one- to five-years of indefinite use among patients, has been also associated with sexual dysfunction which limits its continued routine use [1-7]
The hair-growth stimulating effects of low-level laser therapy (LLLT) was first documented by Endre Mester in 1967 where shaved mice exposed to a low-power 694 nm ruby laser developed accelerated hair regrowth. In 1983, Rampen et al. also reported development of hypertrichosis of patients after treatment with PUVA. Similarly, the first reported case of paradoxical hypertrichosis after IPL treatment for hair removal was published in 2000 by Ferrando et al. The phenomenon of paradoxical hypertrichosis has been acknowledged to occur at an incidence of 0.6% to 10%. Hypertrichosis has since been recognized as a possible side effect of light treatments. These observations paved the way to investigate the potential benefit of low-level lasers for the treatment of hair loss [8-10].
While there is no set value for the best wavelength for LLLT, most treatment wavelengths fall somewhere between 500 and 1100 nm with a power density of 3-90 mW/cm2, and a fluency of 1-4 J/cm2. LLLT at 650-900 nm and 5mW is currently considered an effective treatment for androgenic alopecia from anecdotal evidence, but exact data supporting this setting is still lacking [11].
The basic biological mechanism of LLLT on the molecular level is considered to be the absorption of red and near-infrared light by chromophores contained in the protein of components of the respiratory chain of the mitochondria; in particular the cytochrome c oxidase, which results in photodissociation of inhibitory nitric oxide leading to greater enzyme activity, electron transport, and production of ATP. This allows possible hair regrowth and subsequent reversal of hair follicles from the dormant telogen stage of growth to the active growth or anagen stage. Increased circulation caused by release of nitrogen oxide, promoting vasodilation, also allows for a metabolic boost [12].
Weiss and co-workers were able to demonstrate through RT- PCR and microarray analysis that LLLT modulates 5-a reductase expression which converts testosterone into DHT. There is also an altered vascular endothelial growth factor gene expression as well as matrix metalloproteinase (MMP-2) which have significant roles in hair follicle growth. As result, there was reported stimulation of hair growth on human dermal papillae cells [13].
The usual LLLT wavelengths perform a therapeutic window close to the absorption spectrum of hemoglobin, water and some respiratory chain components. When applied on the hair follicles,laser phototherapy stimulates the epidermal stem cells from the follicle bulge, generating the shift from telogen to anagen. LLLT induces and prolongs the duration of anagen and prevents a premature catagen phase of the hair cycle. Clinical evidence showed reverse hair miniaturization and an increased number of hairs per follicular unit after LLLT therapy. LLLT induces not only an increase in the number of terminal hairs, but also in shaft diameter, together with a decrease of vellus hairs [ 4].
The first RCT on the role of LLLT in MPHL was conducted by Leavitt and colleagues in 2009 in 110 patients. This led to the FDA clearance of HairMax LaserComb, a handheld laser device with 9 beams and a wavelength of 655 nm (±5 %). It was observed in this study that those subjects in the treatment group had significant improvements in overall hair regrowth, slowing of hair loss, thicker feeling hair, better scalp health, and hair shine as documented in the patients’ subjective assessment at 26 weeks. In this study, the low-level light laser device was also well tolerated with no serious adverse events reported [15].
In another study, Lanzafame et al. evaluated the effects of LLLT on females with FPHL in a double-blind randomized controlled trial with results demonstrating a 37 % increase in hair growth in the active treatment group as compared to the placebo group. No adverse events or side effects were reported [16].
These studies show that US FDA-cleared LLLT devices are safe and effective for androgenic alopecia. Hair growth efficacy appears to be comparable to topical minoxidil and oral finasteride in studies of similar treatment duration. No significant side effects have been documented from LLLT, which differentiates it from the other AGA treatment options on the market.
Low-light laser therapy (LLLT) emerged as a new therapeutic approach for the treatment of androgenetic alopecia, gaining approval from the FDA in the last decade. Despite emerging use among dermatologists in the country, there has been no formal study conducted here that seeks to explore the feasibility of low- laser light therapy in treatment as compared to minoxidil therapy alone [17].
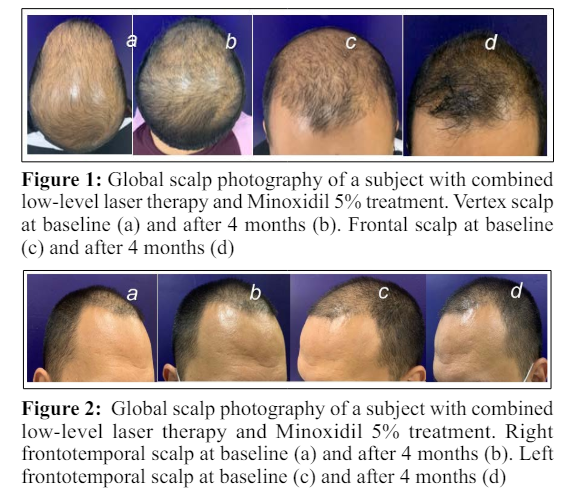
This study is a randomized, controlled, single-observer blinded clinical trial conducted at the East Avenue Medical Center Department of Dermatology Out-Patient Department in Quezon City, Philippines. Twenty-four male patients diagnosed with androgenetic alopecia, aged 18 and above were included and equally randomized into 2 groups. Digital microscopy and global scalp photography with standardized angle, lighting and position were done to determine hair density. Area to be evaluated by digital microscopy was measured 8.5 cm from each side (left and right) of the lateral eyebrow for reproducibility during final assessment. Patients in both groups were instructed to apply topical Minoxidil 5% solution 1ml or 20 drops 2 times a day for 16 weeks. Subjects in the experimental group underwent low-level laser therapy (two times a week for 16 weeks). Patient education on the potential side effects of the medication was done and they were given a daily monitoring sheet to monitor compliance and adverse effects. Assessment of safety and adverse effects (erythema, pruritus and increased hair shedding) by physical examination at every follow up and by the patient’s daily monitoring sheet. Primary outcome measures were 1) change in hair density (as measured by hair count per square cm) of the target area (8.5 cm from both lateral eyebrows) as determined by a digital microscope at 16 weeks from baseline and 2) Global photographic assessment performed by 3 blinded resident dermatologists and by the subjects using a 7- point global assessment scale. Secondary outcome was patient satisfaction determined using a 5-point visual analog satisfaction scale at the end of treatment. Data from 24 respondents was imported to SPSS Statistics 17.0 for analysis. Randomization of the patients were assessed using Fisher’s Exact test for independence. Mann-Whitney U test was used to analyze the primary outcome measures in comparing the efficacy of the combination of 678nm helmet-type low-level light therapy + topical minoxidil 5% and monotherapy topical minoxidil 5% between the control and treatment groups. Wilcoxon Signed-Rank Test was used to compare the variables for every subject at baseline and at the end of treatment. Fisher’s Exact test for independence was also done to see if there is an association between the treatment received and the presence or absence of side effects. All statistical significance testing was set at a p-value of less than .05.
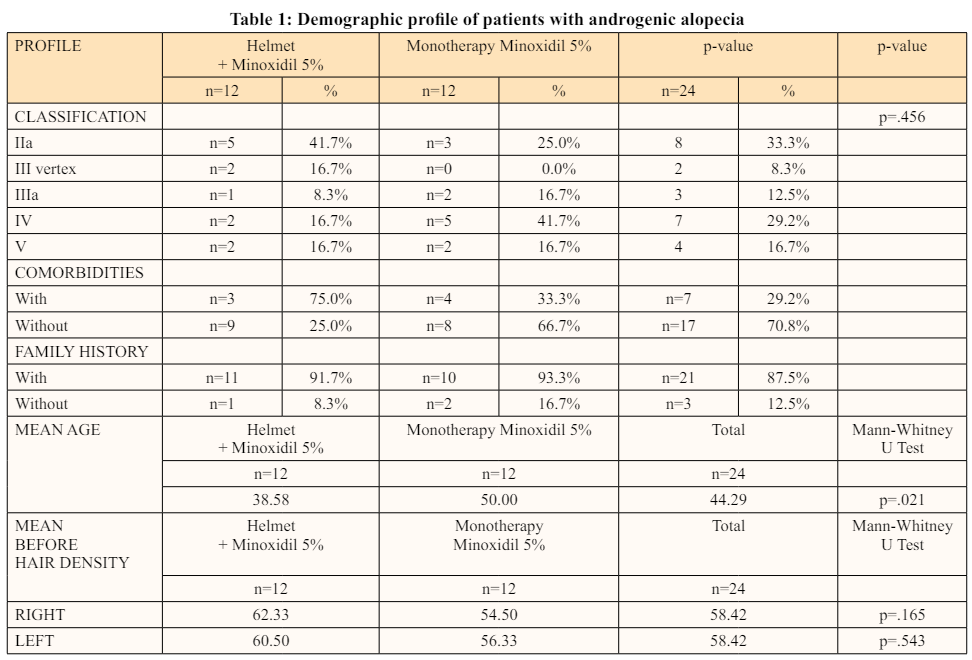
Overall, there is no significant difference found between the baseline demographics of the control and the treatment group-in terms the participants’ Norwood-Hamilton classification (p=0.456 >.05), comorbidities (p=1.000 >.05), and androgenic alopecia family history (p=1.000 >.05). Despite participants’ age being significantly different between the two treatment groups, the participants are still similar in terms of hair density prior to treatment (right p=.165 >.05, left p=.543 >.05). (Table 1)
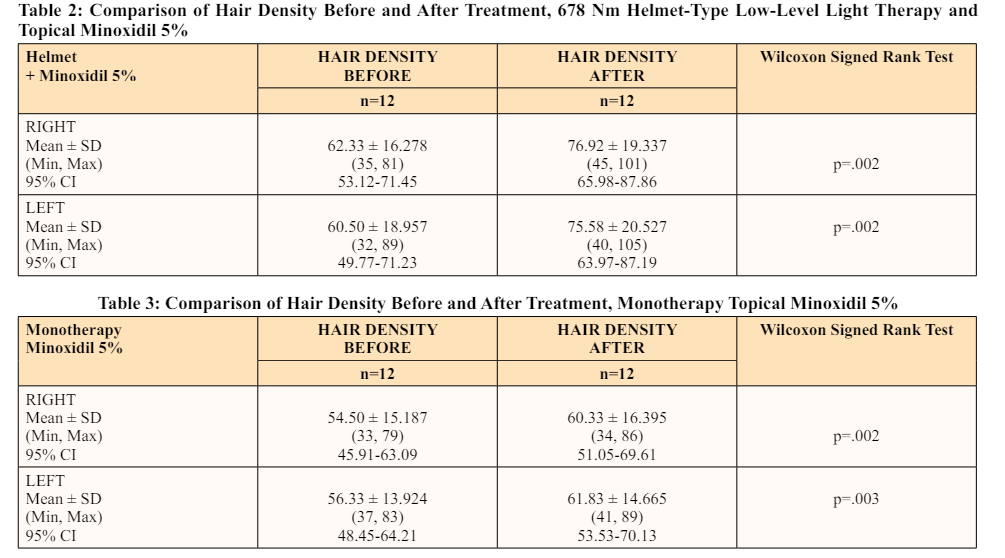
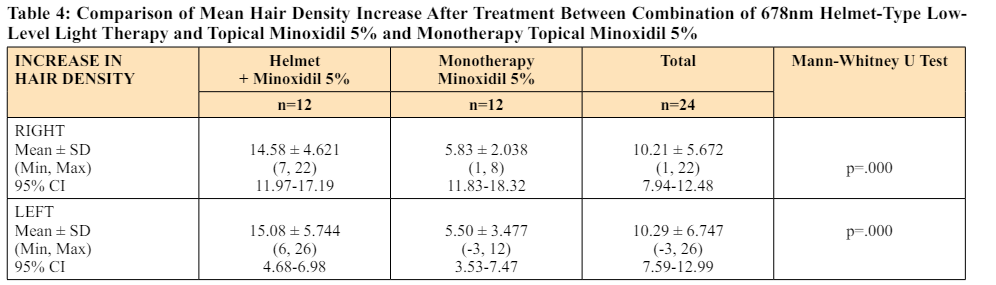
The mean increase in hair density for the combination group are 14.6 and 15.1 for the right and left side, respectively. Analysis showed that treatment with low-level laser therapy and minoxidil did elicit a statistically significant increase in hair densities and this applies for both sides, right (p=.002 <.05) and left (p=.002 <.05). (Table 2) As for the monotherapy group, the mean increase in hair density on the right side is 5.8 and 5.5 for the left side. Also true for both sides, hair densities are significantly higher after treatment with minoxidil; right side (p=.002 <.05) and left side (p=.003 <.05). (Table 3) Comparing the two treatment groups, there is a significant difference in the mean hair density increase between the combination and monotherapy groups (p=.000 <.05) in favor of the combination treatment group. (Table 4)
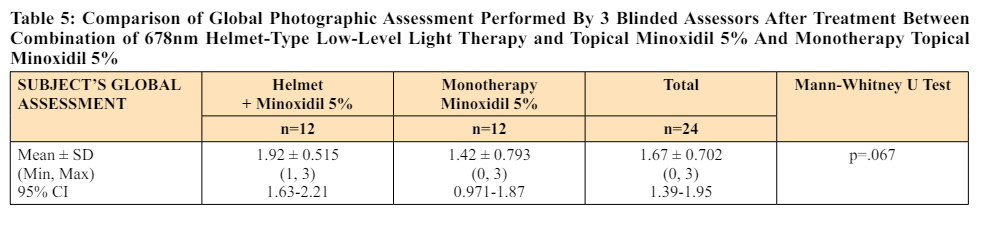
The mean investigator’s global assessment is 1.59 (slight to moderate change) for the combination group, and 1.11 (slight change) for the monotherapy group. The mean difference between the treatment groups in terms of this specific assessment is significant at p=.039. Whereas, the mean subject’s global assessment is at 2 (moderate change) for the combination group and 1.5 (slight to moderate change) for the monotherapy group. Unlike the investigators’, the subject’s mean global assessment did not turn out to be significantly different in the two treatment groups (p=.067 >.05). (Table 5)
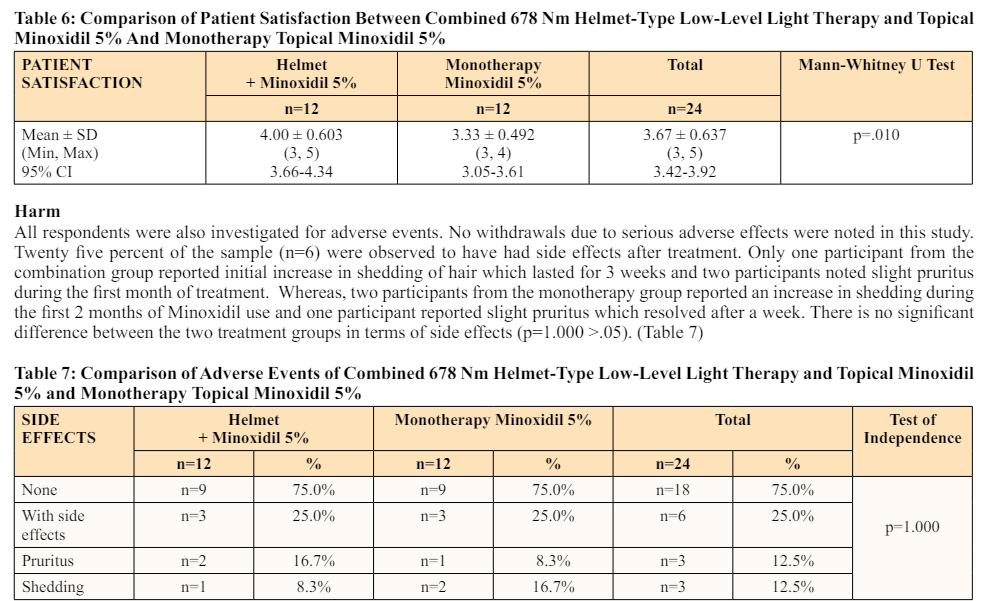
Mean patient satisfaction score is at 4 (satisfied) and 3.33 (no change to satisfied) for the combination and monotherapy group, respectively. Mean scores in satisfaction from patients in the combination treatment group turned out to be significantly higher than those from the monotherapy treatment group (p=.010). (Table 6)
The results of this study show that the combination of helmet- type 678 nm low-level laser therapy and Minoxidil 5% solution is an effective treatment with significantly higher increase in hair density compared to monotherapy of topical minoxidil 5% alone for male androgenetic alopecia with Norwood Hamilton Hair Loss Scale IIa, III vertex, IIIa, IV, and V.
These results are comparable with previous studies where there is noted improvement in both monotherapy and treatment groups. The earliest study utilizing low-level laser therapy as monotherapy or concomitant therapy with minoxidil or finasteride for male and female androgenetic alopecia showed that 63% of patients had moderate improvement and 25% of patients had significant improvement. However, the study utilized the low level laser therapy as monotherapy and returned no statistical difference between the concomitant treatment with either minoxidil or finasteride. This is in contrast with our study where there was significant increase in the outcome measures in favor of the combination treatment group. Our findings are similar to another clinical trial which noted a higher mean increase in hair count in the experimental group of low-level laser therapy with minoxidil compared to minoxidil and turned-off low-level laser therapy (78.3% vs 51.3%, p < 0.001). This study also showed no significant differences in side effects between the two groups. Another randomized controlled trial of 45 female patients observed a significantly higher increase in the number of hair follicles after two- and four months of use (18.6 ± 4.44, p = 0.025) [18-20].
The investigators’ global assessment was also congruent with the difference in increase in hair density and there were also significantly higher global assessment scores for the combination treatment group than the control group. Although the increase in subjects’ global assessment score was not significantly different in the two treatment groups, patient satisfaction was significantly different between the two groups, with the combination therapy group exhibiting higher satisfaction rates on subjective assessment (4 ± 0.603 vs 3.33 ± 0.492 on visual analog scale, p = 0.010). Similarly, the literature cited higher degrees of satisfaction for patients who underwent both low-level laser therapy and minoxidil therapy according to global subjective assessments. For both treatment groups, shedding (12.5%) and pruritus (12.5%) were reported adverse events, but there were no significant differences between the two groups (p = 1.000). Effects of low-level laser therapy may persist even up to 24 months beyond the initial treatment phase. It is expected that baseline satisfaction may even increase as the years progress [21].
Despite its years in the market already, mechanisms involving low-level laser therapy were not yet fully elucidated, and only snippets of mechanisms can be obtained from recent literature. It is assumed that nitric oxide, once released from the electron transport chain, allows oxygen to replace it in its stead and bind to cytochrome oxidase. This process pushes the cellular respiration process forward and increases ATP production leading to increased cellular proliferation. As nitric oxide levels are liberated from the cellular respiration, it can be then surmised that this molecule becomes available for uptake in the nearby tissues, effecting vasodilation and increasing oxygen supply across the microcirculation. Low-level laser therapy was also shown to increase proliferative potential of anagen hair follicles while simultaneously preventing the entry into catagen through a process called photo biomodulation. Minoxidil also stimulates an increase in cutaneous blood supply. The synergistic actions of low-level laser therapy liberating nitric oxide, minoxidil increasing vasodilation, and inherent photo biomodulation of the laser treatment may all be factors in the promotion of hair rejuvenation [22,23].

Although there have been several studies on the use of low- level laser therapy for male pattern hair loss, there is still no consensus for the most effective wavelength for this modality. This is the first clinical trial on the use these specific parameters of laser therapy: wavelength of 678 nm, power of 5 mW, power flux of 0.952 mW/cm2, radiance energy of 216J and fluence of 1.03 J/cm2 for male androgenetic alopecia. This landmark study provides the current body of knowledge on the effectiveness of the combination of low-light laser therapy and minoxidil in the treatment of androgenetic alopecia. With its relative ease of use, safety, cost-effectiveness and efficacy, this treatment modality allows persistent patient compliance that may provide patients with a better treatment option for their disease.
Due to the pandemic, follow-up and compliance of the participants beyond the 16-week minimum period were affected even though 6 from each arm were able to continue up to (the original time frame) 24 weeks. The small sample size and short treatment duration precluded us from generalizing our findings in the general population. Although the sample size seems low, an 80% power of analysis was achieved. And despite the short study duration, there was still a significant improvement observed in terms of hair density for both treatment groups. However, a longer study duration with more participants will further increase the power of this study.
In addition, a computer-assisted software would have provided a more objective measure of the hair density as well as the increase in hair diameter. Nonetheless, hair density as measured by hair count per centimeter square was manually done using a digital microscope increasing the objectivity of the findings. Another measurement tool, the Severity of Alopecia tool II (SALTII), could have also been a good additional outcome measure. Severity of Alopecia tool (SALT) was initially published for determining degree of hair loss based on percentage of SSA involved on the top, back, and each side of the scalp and this is mainly used for alopecia areata. However, they have updated this figure (SALT II) to include smaller increments of scalp coverage to facilitate the assessment of hair loss: (a) where small patches of hair loss predominate, such as in Alopecia Areata or cicatricial alopecia; and (b) where only certain areas of the scalp are involved, such as in male pattern hair loss (MPHL) and frontal fibrosing alopecia (FFA). This appears to be a more objective way of assessing hair loss and is a good tool to include in monitoring response to treatment of patients with hair loss [24,25].
No follow-ups were done after the treatment period, which could be helpful in assessing the temporariness or permanence of the treatment, and whether subtle adverse events might have occurred, such as excessive pruritus, erythema, or scaling of the treated areas.
Although there have been several studies on the use of low-level laser therapy for male pattern hair loss, there is still no consensus for the most effective wavelength for this modality. This is the first clinical trial on the use these specific parameters of laser therapy: wavelength of 678 nm, power of 5 mW, power flux of 0.952 mW/ cm2, radiance energy of 216J and fluence of 1.03 J/cm2 for male androgenetic alopecia. There are still no studies on the use of low-level laser therapy specifically on the Filipino population. This study may contribute knowledge in creating a guideline for optimal conditions for parameters, such as optimal wavelength, fluence, pulse structure, power density, time, number of treatment sessions as well as its efficacy on different populations.
More studies on the use of monotherapy low-level laser therapy are recommended to further assess its efficacy and potential as a stand-alone treatment in hair loss. In addition, its use in other hair loss conditions may also be evaluated in future trials.
