Author(s): Muhammed Anas Ayoob
Castleman’s disease (CD) is an uncommon, lymphoproliferative disease that shares common lymph node histological features. Its aetiology and incidence are unknown. It can affect lymph nodes of any body area, imitating both benign and malignant malformations. Clinically it manifests as the unicentric (localized or unifocal) Castleman disease (UCD) and the less common multicentric (generalized or multifocal) Castleman disease (MCD). In this paper we report a case of a 24 years old gentleman who presented with an incidental radiological finding of a right hilar mass lesion led to a histological diagnosis of this rare condition by Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS TBNA)
Castleman’s disease is a benign disorder first described by Dr. Benjamin Castleman in 1956 [1]. It is also referred to as angiofollicular hyperplasia, and is a non-clonal disease of the lymphnodes. It can affect any lymph nodes, imitating both benign and malignant malformations [2]. We herein report a rare case of hilar unicentric Castleman’s disease.
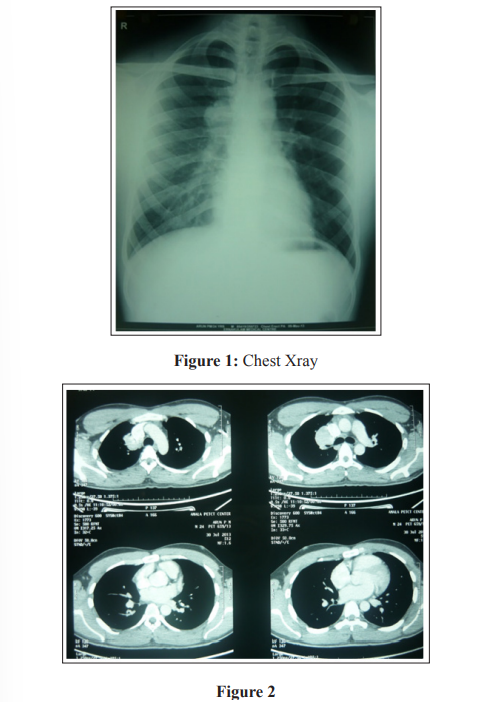
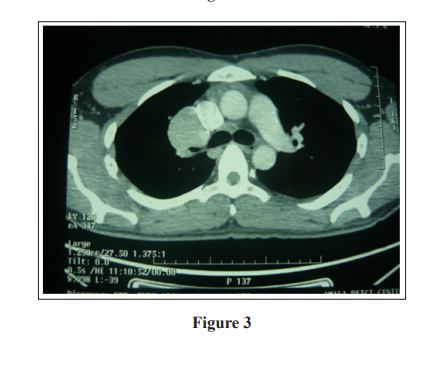
A 24 years old gentleman, working as an Engineer, presented with an incidental finding on a routine chest X-ray during his medical check-up. He was asymptomatic and had no past medical illness. He had no significant family history and was a nonsmoker. Clinical examination showed a moderately built and nourished individual with normal vitals and no crucial findings in the systemic examination. Laboratory data showed almost all normal results. Chest X-ray showed right hilar opacity (figure 1), which was further evaluated by computed tomography (CT) chest, which showed a 39 x 37mm size right hilar soft tissue density mass lesion, compressing right main bronchus & right upper lobe bronchus. This lesion wedged between the right upper lobe, superior vena cava and right middle lobe (figure 2,3).
Differential Diagnosis [3]
• Tuberculosis
• Lymphoma (Hodgkin’s )
• Benign neoplasm: Adenoma, Hamartoma, Thymoma
• Metastatic lymph node enlargement:
• Bronchogenic carcinoma
• Sarcoidosis
• Collagen vascular disease
• Wegners granulomatosis
• Carcinoid
• Castleman’s disease
• Fungal infections such as histoplasmosis and coccidioidomycosis
• Viral (Infectious mononucleosis)
• Berylliosis
• Atypical mycobacteria
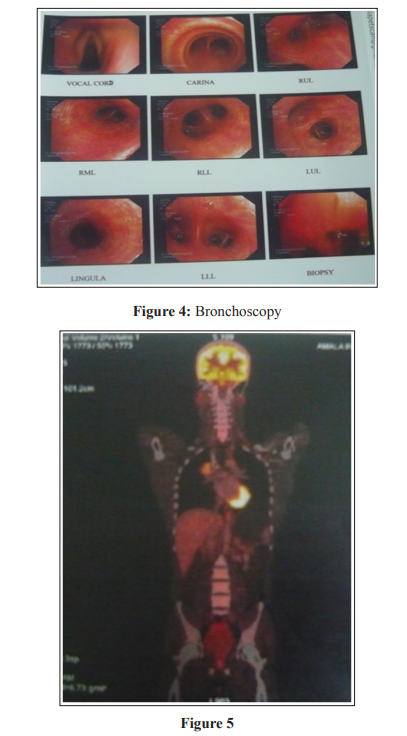
Fiberoptic bronchoscopy was done, which showed narrowed right upper lobe posterior orifice and mucosal bulge noted at the junction of the right upper lobe apico-posterior segment (figure 4). Bronchial wash and conventional transbronchial needle aspiration (TBNA) was done. Cytopathological examination was negative for dysplastic cells and no evidence of granuloma. Positron emission tomography (PET)-CT revealed elevated metabolic activity in a smooth-bordered, oval-enhancing soft tissue nodular mass in the right hilum and a few metabolically active tiny mediastinal nodes (precarinal) (figure 5,6). Also noted Metabolic activity in the thymus and no other focus of elevated metabolic activity. So further evaluated by EBUS- TBNA and cytopathological examination suggestive of Castleman’s disease - Hyaline vascular type. Immunohistochemistry revealed CD20 positive B cells showed a reactive pattern for Ki67 & bcl2. CD 3 positive T cells and a few CD 68 positive cells were seen, and Cyclin D1 was negative. The diagnosis of unicentric Castleman’s disease- hyaline vascular type was made based on final histological findings. He was referred to a thoracic surgeon for surgical excision.

Castleman disease is a rare lymphoproliferative disorder with a nondefinite etiology and can be classified into subtypes based on clinical and histological manifestations [4]. Castleman’s disease is classified as a ) unicentric versus multicentric, based on clinical and radiological findings, and b) as HIV negative versus HIV positive, based on the HIV status of the patient [5]. All these factors need to be taken into account in the assessment of patients. Histologically the main types are [6]: (figure 7,8)
The hyaline vascular type characterised by lymphoid follicular proliferation at different levels of maturity, often forming a layered or ‘onionskin’ pattern surrounding a hyalinised vessel at the centre of the follicle. These vessels are often prominent and reactive. This is more commonly seen in the localised form of the disease.
The plasma cell variant has sheets of mature plasma cells within the interfollicular tissues surrounding larger germinal centres and has significantly less vascularity. The multicentric form of the disease is nearly always associated with this variant.
A third histological variant showing a mixed picture can also be seen in MCD.

Unicentric Castleman’s Disease is usually a slow-growing solitary mass typically located in the mediastinum or mesenteries.
Typically, there are no constitutional symptoms and no elevation of acute phase reactants (Interleukin 6, ESR and CRP). Symptoms may be due to a mass effect of bulky lymphadenopathy. In a few cases, abnormal clonal, cytogenetic findings have been described arising from a dysplastic follicular dendritic cell network, but it remains uncertain how these findings are related to Unicentric Castleman’s Disease. In 90-95% of cases, surgical resection is curative, and normally there is no progression to lymphoma or association with other tumours. The prognosis is exceptional, with a five year survival of close to 100%.
In multicentric Castleman’s disease, there is usually widespread lymphadenopathy with occassionaly hepatosplenomegaly. “B” symptoms, including fever, severe fatigue, night sweats, weight loss, and anorexia, are typically present. These symptoms are typically driven by the overproduction of interleukin 6. It results in an acute phase reaction with elevated ESR, CRP, fibrinogen, thrombocytosis, and hypergammaglobulinemia, while haemoglobin and albumin levels are decreased [8].
Patients typically have peripheral oedema that is poorly responsive to loop diuretics and suffer from anaemia and hypoalbuminemia. Approximately 20% of patients have peripheral neuropathy. Other conditions associated with multicentric Castleman’s Disease include autoimmune hemolytic anaemia, multiple myeloma, amyloidosis, and Pemphigus. Multicentric Castleman’s Disease runs a more aggressive course and can progress to non-Hodgkin’s lymphoma. Multicentric Castleman’s Disease often requires systemic therapy
In this case, we initially used conventional TBNA for tissue sampling, but it was inconclusive. So further evaluated by EBUS- TBNA and diagnosed Castleman’s disease by proper sampling and pathological examination. Despite its main role in the diagnosis and staging of cancer, the literature demonstrates that EBUS-TBNA is a safe and reliable procedure for diagnosing non-neoplastic diseases involving mediastinal lymph nodes.
This case report is presented for its rarity. Hilar lesions are involved in Castleman’s disease and may be confused with other common causes of mediastinal lymphadenopathy like tuberculosis, sarcoidosis and nodal secondaries. EBUS-TBNA is a reliable procedure for diagnosing non-neoplastic diseases involving mediastinal lymph nodes. Surgical removal of the tumours in the unicentric type of Castleman’s disease is the treatment of choice.
