Author(s): Sultan Alanazi
Buccal exostosis is bony prominence located on buccal side of alveolar ridge of maxilla or mandible. It is commonly seen in maxilla than mandible, whereas the etiology remains unclear. This article presents a rare case of bilateral maxillary buccal exostosis, distomolars and polydactyly along with surgical management of exostosis. A 39-year-old male patient came to the dental OPD with a chief complain of swelling in the right and left back region of upper jaw from 12 years, which was a cosmetic concern to the patient. Patient was medically healthy with no familial history of gingival overgrowth. On examination, patient had polydactyly and bilateral mandibular distomolars. These isolated findings couldn’t be related to any syndrome after thorough examination and medical consultation. Finally, the treatment plan consisted of, oral hygiene instructions, mechanical debridement and periodontal resective osseous surgery, so as to reduce gingival inflammation and improve esthetic by removing the exostosis. Nonsurgical periodontal therapy alone did not reduce the gingival enlargement because of the bony nature of enlargement, thus necessitating surgical intervention. Post-operative evaluation at 1, 3 and 12 months reveled an uneventful healing and no sign of recurrence at surgical sites.
Tori and exostoses are nodular protuberances of calcified bone designated according to their anatomic location. Torus palatinus (TP) and torus mandibularis (TM) are the two most common types of intraoral osseous overgrowths [1]. Buccal exostosis is a bone prominence located on the buccal aspect of alveolar ridge of the maxilla or mandible and usually consists of dense cortical bone that are relatively avascular. It usually occurs bilaterally and seen in the premolar and molar region. It is more commonly seen in maxilla than mandible (5.1:1) and affects men more than women (1.66:1) [1-3]. The overgrowth is usually asymptomatic but may cause esthetic concern to the patient. The area serves as a good nidus for food lodgment, thus causing difficulty in oral hygiene practice by the patient. No consensus has been reached to determinate the etiology of buccal exostosis but it is believed that the reason is multifactorial, including environmental elements acting in unclear relationship with genetic factors [4-7]. The diagnosis of a buccal exostosis is based on the clinical examination along with radiographic interpretations. Radiograph of exostosis appears as well-defined round or oval calcified structure superimposing the roots of teeth [1,4].
Polydactyly is a condition of physical anomaly in humans resulting in the presence of extra fingers and/or toes. The extra finger is commonly seen in the ulnar (little finger) side of the hand [8]. Distomolar is a supernumerary tooth which is located in the distal aspect of third molars. It appears more frequently in men than in women. This case report presents a rare case of buccal exostosis associated with distomolars and polydactyly along with surgical management of exostosis [9,10].
A 39-year-old male patient was referred to the Department of Periodontology, College of Dentistry, King Khalid University with the complaint of swelling in the right and left posterior region of upper jaw from 12 years (Figure 1).

Figure 1: Preoperative view showing enlargement at maxillary left and right buccal region
The overgrowth was a major cosmetic concern to the patient. Whereas, the area serves as a good nidus for food lodgment, thus causing difficulty in oral hygiene practice by the patient. Detailed personal and family history of the patient revealed that the enlargement was not familial in nature. The patient didn’t reveal any history of medication and reported no known drug allergies. On extra-oral examination we found that patient had a high and broad smile line (1st molar to 1st molar). The general examination revealed the patient had a Polydactyly in both hand and feet (Figure 2) and the radiographic examination showed bilateral distomolars in lower arch (Figure 3).
Figure 2: : Polydactyle in both hands and feet
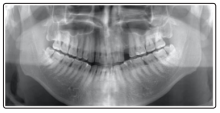
Figure 3: Panoramic radiograph showing Bilateral Distomolars in lower arch
These isolated findings couldn’t be related to any syndrome after thorough examination and consultation. The overgrowth was an esthetic problem to the patient due to the broad smile line. There was a generalized gingival inflammation in the upper and lower arch, and the probing depths were in the range of 3-4 mm with areas of 5 mm in the upper left first molars. There was Glickman grade I furcation involvement in both maxillary left and right first molars. After obtaining a medical clearance regarding the isolated findings, periodontal treatment was planned as patient education and motivation by oral hygiene instructions, scaling and root planing and periodontal resective osseous surgery. The patient was prescribed 0.2% chlorhexidine gluconate two times daily so as to reduce plaque and gingival inflammation. Re-evaluation after four week showed normal gingival characteristics, whereas the gingival enlargement failed to regress. After explaining the risks and benefits of surgery to the patient, an informed consent was obtained. After administration of local anesthesia, full thickness mucoperiosteal flap was reflected in order to gain complete access to the exostosis
Resective osseous surgery was performed in the following steps:
After removing the exostosis, surgical site was checked to determine any further recontouring. On obtaining the final result, the flap was sutured with 3-0 vicryl suture material. Postoperative medications and instructions were given to the patient. Patient was recalled after 10 days for suture removal. Post-operative evaluation at 1, 3, 6 and 12 months reveled an uneventful healing at all surgical sites without any reported complication and clinical sign of recurrence.
Right side Left side
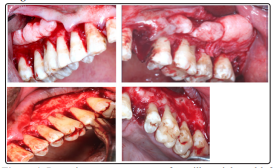
Figure 4: Resective osseous surgery of maxillary right and left buccal exostosis

Figure 5: 12 month’s postoperative view showing absence of enlargement in maxillary left and right buccal region
In this case report on examination, patient revealed polydactyly and bilateral mandibular distomolars and maxillary buccal exostosis. According to the patient’s medical and dental history, it was difficult to relate the exostosis to a direct cause. The patient was medically healthy and not under any medications. Exostosis was not in the family as the patient didn’t mention any that any family member had gingival overgrowth.
Buccal exostosis is a benign outgrowth, which is usually seen in the facial aspect of the upper jaw as compared to the lower jaw [1,2]. These outgrowths are usually asymptomatic, but sometimes may increase in size and cause cosmetic concern. They are commonly seen in male population compared to female population. They are commonly seen in premolar and molar region.
Polydactyly is defined as a condition in which a person has more than five fingers per hand or five toes per foot. It is considered to be the most common birth defect of the hand and foot. Surgery may be considered for poorly formed digits or very large extra digits. Surgical management depends on the complex level of the deformity [8].
Distomolar is a supernumerary tooth which is located distal to third molars. It usually appears in male more than female. The ?Dental lamina hyperactivity theory? to be the most accepted theory to explain this Condition. Distomolars are usually impacted. They can be asymptomatic or cause complications. Radiographs are important diagnostic tool for the detection of distomolars. Treatment involves the removal of the distomolar if there are associated complications otherwise to keep under observation [9,10].
A differential diagnosis of Fibrous dysplasia and Gardner syndrome was given. Gardner syndrome was excluded due to no appearance of multiple polyposis of the large intestine; osteomas of the bones; multiple epidermoid or sebaceous cyst of the skin. Clinical appearance of bilateral nodular growth on the buccal surface of the maxilla under the muccobuccal fold over which the mucosa appeared blanched ruled out fibrous dyslasia [11,12].
In this case report, phase I periodontal therapy alone did not reduce the gingival enlargement because it was bony enlargement, thus surgical intervention was needed. Vertical grooving was the first step of the resective osseous surgery to reduce the thickness of the alveolar housing and to provide relative prominence to the radicular aspects of the teeth. Cooling with sterile saline must be done so that the temperature of the bone is not raised beyond 47°C. Radicular blending was done next which is an extension of vertical grooving in an attempt to gradualize the bone over the entire radicular surface to provide the best results from vertical grooving. Gradualizing marginal bone was the minimal bone removal to provide a regular base for gingiva to follow [13-15]. Post-operative evaluation visits at 1, 3, 6 and 12 months revealed uneventful healing at all surgical sites without any reported complication and clinical sign of recurrence.
The case report presented above illustrates a unique and rare presentation of bilateral exostoses on the buccal side of the maxillary premolar - molar region. Resective osseous surgery was performed to correct the bony architecture. The procedure resulted in successful establishment of the normal bony contour without any unwanted complications.
