Author(s): Nader Francis*, Ahmad Al Kamali and Sinan Yavuz
Hemoptysis is a rare, life-threatening condition in childhood defined as bleeding into the lungs due to underlying disorders or respiratory tract abnormalities. The bleeding from an arterial malformation to normal lung segments without underlying cardiovascular or pulmonary disorders is widely reported in adults but extremely rare in the pediatric age group. Bronchial artery aneurysm (BAA) is a rare vascular malformation complicated with a bronchial artery to pulmonary artery (BA PA) fistula. BAAs are life-threatening conditions because of the substantial risk of rupture that can cause massive hemoptysis. In such a case, BAA embolization (BAAE) has become essential management. We report here previously healthy child presented with massive hemoptysis due to systemic-pulmonary fistula, which was bleeding controlled by BAAE.
BA-PA fistulas are extremely rare vascular anomalies due to the connection between systemic and pulmonary arteries. It can be congenital or acquired [1]. Most patients usually asymptomatic once the diagnosis is confirmed need urgent management because it can be fatal due to massive hemoptysis if rupture occurs. While exact etiology is unknown, most bronchial artery aneurysms (BAA) are linked to chronic inflammatory, infectious, and vascular lung diseases [2]. BA-PA fistulas are very few numbers in reported studies [3, 4]. In literature, 4% of pulmonary AVMs have been reported to have systemic arterial supply, and rarely bronchial artery can be the artery feeding the AVM [4].
In this case report, we describe a patient who presented with massive hemoptysis and dyspnea, found to have a BAA with associated BA-PA fistula. The case was successfully managed with BAA embolization. On the follow-up visit, she is noted to be totally fine with no more symptoms.
A 9-year-old girl previously healthy admitted to another facility with a chief complaint of racing heart and sudden onset productive cough with blood-tinged sputum after exercise. The mother reported that the cough had been present intermittently for a few days but became more frequent and was productive of bloodtinged sputum on the day of presentation. The patient was slightly short of breath with fever but denied sick contacts. The mother denied any other bleeding, including melena or hematuria. Past medical history was unremarkable. Blood work at that time was normal. On physical examination, the patient was well-nourished, slightly pale, and in acute distress. She was febrile, with a slightly increased respiratory rate, normal blood pressure, and oxygen saturation on room air but was tachycardic. Her Extremities, abdomen, neurological, and neck examination were normal. Cardiac examination revealed tachycardia but no murmurs, rubs, or gallops. The patient placed on oxygen also an intravenous fluid bolus gave. An electrocardiogram showed sinus tachycardia. Chest X-ray (posterior-anterior and lateral views) showed large patchy alveolar infiltrates and consolidation in the lower right lob. Complete blood count revealed significant low hemoglobin but no leukocytosis or thrombocytopenia. Electrolytes and renal function, and coagulation profile were normal. The ESR and CRP were normal.
The decision to do an endoscopy was made to rule out hematemesis. During the procedure, the patient developed massive hemoptysis, which was needed intubation and ventilation. An urgent bronchoscopy was performed. It revealed active bleeding, and the installation of adrenaline controlled bleeding. The patient received a blood transfusion and started to the broad-spectrum antibiotic. She transferred to our hospital for proper management and further evaluation. She was ventilated on receiving her in PICU, on PRVC mode with no acute bleeding from the endotracheal tube. Initial blood workup including (CBC, CRP, ESR, coagulationprofile, electrolyte, renal and liver function test C-ANCA, ANA, Anti- DNA, AGBM, H1N1 PCR, APL IGM, urine, blood and sputum culture, Ultrasound abdomen) were normal. Chest X-ray bilateral basal consolidation, more on the right side. (Image 1) Repeated bronchoscopy showed clots in the trachea and the right main bronchus lower and middle lobe without active bleeding. The left lung is normal (Image 2).

Bilateral basal consolidations, more on the right side.
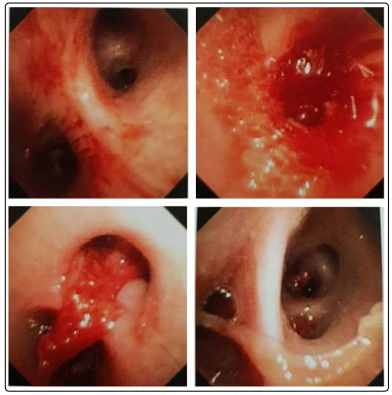
Right lung: no active bleeding with multiple clots in the main right bronchus, lower and middle lobe
The next day, the patient developed massive hemoptysis. It was controlled by tranexamic acid nebulization. An urgent computed tomography (CT) chest with contrast revealed right lower lobe sub-segmental consolidation suggesting a localized pulmonary infarction in the lower right lob (Image 3). A vascular cause of the bleeding was suspected based on the localized massive bleeding, with a chest Ct scan with contrast suggesting a localized pulmonary infarction in the lower right lob. A pulmonary arteriovenous malformation (PAVM) was suspected. The patient underwent cardiac catheterization to localize the bleeding site, which confirmed the right bronchial artery, which gave an abnormal connection to the pulmonary artery (Aneurysmal fistula). Another superior right bronchial artery was supplying to the same aneurysmal (Image 4). She promptly underwent bronchial artery embolization. A lipiodol ultra-fluid solution was injected in both bronchial arteries with the microcatheter with the arteries’ total occlusion. No other arteries were found supplying abnormal fistula. Which successfully stopped the bleeding. Following the BA embolization, the patient’s hemoptysis ceased, and she recovered uneventfully.
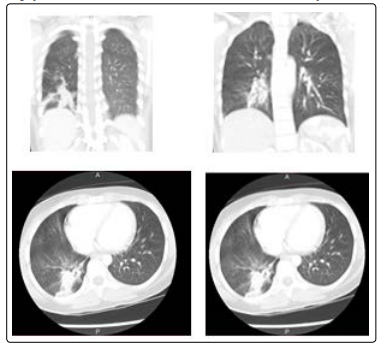
Image 3: CT chest with contrast: revealed right lower lobe sub-segmental consolidation suggesting a localized pulmonary infarction in the lower right lob.
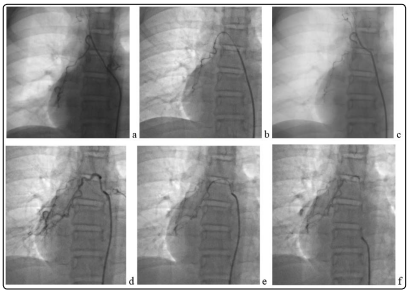
Image 4: Interventional angiogram:
(a)first bronchial artery,
(b)embolization of its distal part,
(c)
preservation of its proximal part to avoid possible spinal ischemia.
(d) Second bronchial artery,
(e) embolization,
(f) final result
Follow up the child in the clinic; she is doing well, healthy, asymptomatic. The followed Chest radiograph after three and six months were normal (Image 5,6) [5].

Chest Xray (after embolization) on follow up after 3 months: Coils of previous embolism noted in the right paracardiac border.

XR Chest (after embolization) follow up for six months: Linear serpiginous lines of previous intervention.
In a healthy state, pulmonary tissues are fed from pulmonary and bronchial arteries. Deoxygenated blood came through the pulmonary arteries to the lung, while oxygenated blood returns to the heart by pulmonary veins. Bronchial arteries arise from systemic circulation. Right lung supply from the right branch of bronchial arteries which originates from the right intercostal artery. Descending thoracic aorta gives two left bronchial arteries to supply the left lung. The drain of both side bronchial arteries via pulmonary veins into the left atrium [6]. There is no direct connection between these arteries. A systemic pulmonary arteries fistula is formed in the presence of communication between this vascular system.
BAA is a rare condition, and accompanying with BA PA is extremely unusual. It should be treated after the diagnosis because of the risk of rupture due to a lack of stability [7]. Despite complications that can occur, BAE remain is the treatment of choice [2]. In the literature, there are few cases of developed hemoptysis due to systemic-pulmonary artery malformation in the absence of lung or systemic disease [8].
Massive hemoptysis is a life-threatening event that needs urgent assessment and treatment. Bronchoscopy, CT, and X-ray chest are helpful to localized of bleed [7]. While CT angiography is useful to localized, detect the cause and mechanism of the bleed [9]. Despite these investigations, 25% of cases remain undiagnosed and are called cryptogenic hemoptysis [10]. In such suspected pathology, a selective bronchial angiography followed by embolization is recommended [11].
The rupture BAA rate with BA to pulmonary circulation compared with BAA alone unknown because data for this event limited to case reports [2]. Bronchial artery malformation can be congenital or acquired [8]. In the case of acquired mostly associated with underlying such as bronchiectasis, tuberculosis, or other inflammatory diseases [12]. Congenital BA-PA fistula vascular supply to normal lung tissue has been rarely described [1]. BA embolization can have complications as unintentional migration approximately 3%, and air emboli 2% of cases [11, 13]. The risk of spinal artery embolization around 6.5%. BAE techniques are continuously developing [14]. Each case is evaluated individually to choose an embolization agent and consider the durability of occlusion, size of occluded vessel, and ease of delivery. The relapse rate in a patient who developed hemoptysis managed with BAE 10 to 55% after around 2 years [15].
Our case had the right bronchial artery-pulmonary artery fistula and superior right bronchial artery-pulmonary artery fistula (aneurysmal). To our knowledge, she presented with massive hemoptysis due to aneurysmal fistula rupture, which was treated successfully with BA embolization. She never complains from any systemic or lung disease, and her malformation is seldom.
We report a rare case of a child with BA-PA fistula, accompanied by a BA aneurysm. BA-PA malformation is extremely rare in the pediatric age group can be presented with massive life-threatening hemoptysis for which needed urgent management. It is important to do detailed investigations in such cases. In the literature, few cases reported in children; most of the patients were reported in adults. Imaging studies can be normal, and CT angiogram may not show fistula formation; the bronchial artery angiogram is recommended for the diagnosis.
