Author(s): Soni Patel, Shreya Rani and Nilotpol Kashyap*
Papillon-Lefever syndrome (PLS) or palmoplantar keratoderma with periodontitis (Rapini, Ronald P; 2007) is an autosomal recessive genetic disorder caused by deficiency in cathepsin C [1,2].
Two French physician Papillon & LeFevre were the first one to characterize this disease in a brother & sister suffering from palmoplantar hyperkeratosis associated with early onset of periodontitis & premature loss of primary & permanent dentition (P-L 1924) [1,3]. The third component that is Dural calcification in this disease was added by Gorlin et al 1964 (Gorlin 1964) [1]. Other symptoms include hyperhidrosis, arachnodactyly, increased susceptibility infection & mental retardation (Hattab FN 1995, sollecito TP 2005) [1-6].
It has a prevalence rate of 1-4 cases per million. PLS is inherited as an autosomal recessive disorder [1-3]. There is a 25% risk for children to be affected if both parents are carrier of the defective gene. (Hart TC 1994).The rate of prevalence is more in consanguineous offsprings. (Khan FY 2012) [1-6].
Alteration in ectodermal & mesodermal components leads to the skin lesion in this syndrome, but there is no such explaination regarding rapid loss of deciduous as well as permanent teeth. (Kothiwale SV 2008).
PLS may cause cellular immune defect with decrease chemotaxis & phagocytic function of neutrophils & granulocytes. Causation of periodontal problems in PLS may be associated with the presence of pathogens such as Actinobacillus Actinomycetemcomitans, Capnocytophaga Gingivalis, Porphyromonas Gingivalis, Peptostreptococcus Micros, Fusobacterium Nucleatum & Spirochetes [1,2].
Palmoplantar keratosis appears as well defined demarcated keratotic plaques over the palmar & plantar surfaces [1-6]. Hyperhidrosis present may be seen with the keratosis giving a foul odor [1-3].
There is early onset of periodontitis which starts at the age of 3-4 years. Gingiva then appears inflammed & bleeds on provocation [5,6]. The periodontitis progresses rapidly & doesn’t respond to the conventional periodontal treatment.
There is early shedding of deciduous teeth mostly by 3-4 years of age. Even though the development & eruption of it occurs at a normal chronological age [5]. Gingiva reverts back to normal after deciduous teeth gets shed but the gingiva again gets inflammed as soon as permanent teeth erupts [5,6].
At the age of 13-16 years there is complete shedding of permanent teeth except third molar which gets shed later [5].
A 13 year old male child reported to the Department of Pedodontics & Preventive Dentistry, at Vananchal Dental College and Hospital Garhwa, with the chief complaint of loss of multiple teeth. While taking the past dental history it was revealed that his deciduous teeth had erupted normally but were eventually lost at the age of 5 years approximately
After eruption of the permanent teeth there was bleeding from the gingiva while brushing & eating. As per patient he began losing all his upper & lower incisors by the age of 10 years & all the remaining tooth were Grade-III mobile when checked clinically.
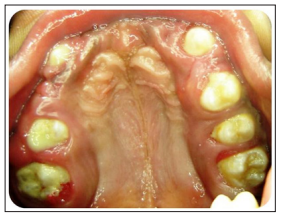
Figure 1
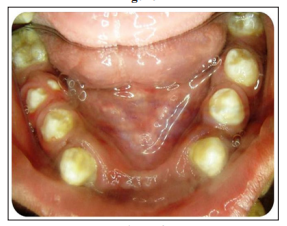
Figure 2

Figure 3
There was no relevant medical history and parents were not of consanguineous marriage, there was no significant prenatal history given by the mother.
The patient was mesomorphic. His physical and mental development was normal. The patient showed hyperkeratosis papules on his hands Figure 4, feet Figure 5 and knees Figure 6

Figure 4:Keratosis of Palm

Figure 5: Keratosis of fee
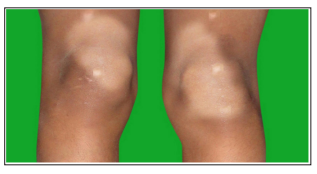
Figure 6: Hyperkeratosis Papule on Knees
Orthopantamogram Figure 7. shows excessive bone loss in respect to both maxilla and mandible & presence of teeth namely 13, 14, 15, 16, 23, 25, 26, 33, 34, 35, 36, 43, 44, 45, 46, in addition to it unerupted 17, 27, 37, 47 can be seen. Loss of bone support around all the erupted teeth.
Lateral cephalogram shows dural calcification Figure 8.

Figure 7: Orthopantamogram Showing Overall Bone Loss

Figure 8: Lateral Cephalogram Showing Dural Calcification
PLS is an autosomal recessive inherited disorder [1-4]. It is thought to be because of mutation in cathepsin-C [1-6]. The Cathepsin-C gene is located on chromosome 11q14.1- 11q14.3 (Wani A 2006) [1-3]. Cathepsin-C is a lysosomal exo-cysteine protease encoded by CTSC gene, central co-ordinator for activation of many serine protease in immune cells. Activation of serine protease results in degradation of extracellular matrix component which further leads to tissue damage & chronic inflammation in the patient. Mutation in the Cathepsin- C gene causes prepubertal periodontitis in patients with PLS.
Differentiation should be made with certain diseases like Haim Munk syndrome, Olmsted syndrome, Huriez syndrome, Epidermolysis bullosa herpetiformis, Cole disease which shows palmar-plantar keratosis like PLS but doesn’t show juvenile periodontitis [1-6]. On the other hand certain diseases like hypophosphatasia, acrodynia, histiocytosis X, leukemia, cyclic neutropenia associated with periodontitis & premature loss of teeth doesn’t show palmar-plantar keratosis [1-3].
Periodontal Therapy - Scaling followed by root planning was done in the patient, counseling was done for maintaining his oral hygiene. Chlorhexidine mouthwash was prescribed for oral prophylaxis.
Prosthetic Rehabilitation - After completion of periodontal therapy patients was given removable partial dentures to replace his lost upper & lower anteriors. Fixed partial denture was not given as the abutment teeth were mobile due to excessive bone loss. Dental implants were not given because the growth of maxilla & mandible has not been completed & due to the fear of rejection and because of the socioeconomic status of the patient.
Maintenance Phase - patient was asked to report to the Department of Pedodontics & preventive dentistry after every 3 months for evaluating his oral hygiene status & to check the fitting of removable partial denture.
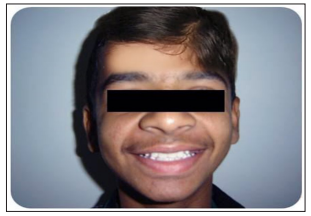
Figure 6: Removable Partial Denture
Patients with PLS are most likely to consult a dentist for there periodontal problems. As such a dentist should have sufficient knowledge about the signs & symptoms of PLS. Thus dentist should also learn to differentiate between diseases having similar signs & symptoms. An early diagnosis by the dentist can prevent the loss of permanent teeth by instituting oral retinoids during the eruption of permanent teeth. The dentist can also help those patients who comes at a later stage by administering prompt periodontal therapy to preserve those tooth which are still present.
