Author(s): Molina Leon
Acute motor axonal neuropathy (AMAN), is a pure motor axonal form of Guillain-Barré syndrome (GBS) characterized by the absence of sensory and cranial nerve involvement. Its prevalence in western countries, together with the sensorimotor variant, ranges in 3-5% of GBS cases. Acute motor axonal neuropathy (AMAN), or motor axonal form of Guillain-Barré syndrome, is a rare entity in the West, but it can be underestimated by confusing it with demyelinating forms of the syndrome if serial neurophysiological studies are not performed.
To present a case seen in our hospital of a patient with acute tetraparesis of two weeks of evolution.
A 73-year-old man with acute tetraparesis of proximal predominance of 2 weeks of evolution, suspected AIDP VS AMAN. Referred by Suspected GUILLAIN BARRE SYNDROME (suspected AMAN). On examination, a decreased muscle balance is detected. Decreased tactile sensitivity. Symmetrical and diminished ROTs. BILATERAL ROTULIAN ARREFLEXIA. Began with acute, predominantly proximal tetraparesis one- two weeks. No RAF. HTN in treatment. No diabetes or dyslipidemia. 2-4 cigarette smoker daily. He does not drink alcohol regularly. No heart disease. No bronchopathy. He refers that since he was 20 years old he has presented several episodes of weakness in MMSS and MMII with subacute onset and slow recovery, not studied. Operated for cataracts in both eyes. Bilateral inguinal herniorrhaphy. Treatment: tamsulosin, diovan, iron, rivotril, zanidip. COVID NEGATIVE.
2-3 weeks ago diarrhea of 1 week of evolution without fever. A few days then paresthesias in the hands which subsided in 1-2 days and progressive upper and lower limb weakness. 3 days ago and today falls due to weakness in MMII, plus EID. No pain or sensitive alterations. No alterations sphincter.
Preserved Vertebral alignment with left convex lumbar scoliosis. Morphological changes are seen in vertebral bodies with marginal osteophytes due to spondylosis. Moderate degenerative disc changes from C3 to C7 and diffuse lumbar discs are observed characterized by dehydration, slight loss of height, more pronounced in L5-S1 and diffuse cervical disc bulges, together with uncoarthrosis and lumbar from L2. The previously described findings produce obliteration of the anterior subarcnoid / epidural space, without significant canal stenosis, moderate stenosis of the right foramina from C4 to C7 and mild stenosis of the lumbar, which contributes to facet hypertrophy. Marrow with normal signal intensity and Morphology. Medullary Cone and roots of the horsetail without alterations. No evidence of soft tissue mass. Slight distal asymmetry in the thickness of the psoas muscle, the left being slightly greater than the right. More pronounced facet osteoarthritis from C5 to C7 and from L3. In the included cuts of the thorax, fat infiltration of the gluteus maximus is seen.
There is no cord compression or foci of compressive myelopathy that justify the symptoms .Intervertebral chondrosis due to moderate degenerative disc disease, together with diffuse cervical disc-osseophytic bulges from C3 to C7 and diffuse lumbar bulges from L2 to S1, without significant stenosis.
Conscious, alert, normal speech, preserved language. Centered pairs. Strength MMSS 4- / 5, distal 3/5. MMII force: bilateral 3-4- / 5 hip flexion, right knee extension 4- / 5, left 4 + / 5; knee flexion 4- / 5, dorsal flexion and plantar 3-4- / 5 bilateral. ROT bicipitals right ++, left ++. Tricipital ++. patellar right +, left ++, achillean +. Plantar flexors. No sensitive alteration. No ataxia.
Clear and Transparent Cerebrospinal Liquid Appearance. Leukocytes 10,polymorphonuclear 30%, L. mononuclear 70%, Red blood cells 0, Glucose 59, Proteins 79.9, Lactate 2.10. ADA pending to come.
There are no intra- or extra-axial hemorrhages or signs that suggest established extensive acute ischemic injury. No mass effects or deviation of middle line. Good gray matter-white matter differentiation. Mild cortico-subcortical retraction according to age. Cavum vergae as a variant of normality. As a window with a bone window it is not observed alterations in bone or occupation of the paranasal sinuses or the mastoid cells included in study. Conclusion: Study without evidence of acute intracranial pathology
Findings suggestive of small ischemic infarcts. Findings suggestive of small bilateral parietal corticosubcortical chronic ischemic infarcts. Mild leukoatia (Fazekas grade 1) of probable vascular origin of small glass. Findings suggestive of abnormal Fe deposition in basal ganglia, red nuclei, and black substance. Mildmoderate global cortical atrophy predominantly frontotemporal. Temporal atrophy moderate medial.
There is no spinal cord compression or compressive myelopathy foci that justify the clinic. Intervertebral chondrosis due to moderate degenerative disc disease, along with bulging diffuse cervical disc-osseophytic from C3 to C7 and diffuse lumbar from L2 to S1, without significant strictures.
During his stay in the ward, the patient remains hemodynamically stable. He has featured episodes of predominantly nocturnal agitation controlled with 25 mg of quetiapine. At the motor level, some improvement: upper extremities with proximal force 4 + / 5 deltoids, 4 biceps and bilateral tricpes, flexion-extension of hands 4-, extensor, interossei 3 with greater subjective involvement on the left; MMII strength 3/5 psoas 4+, quadriceps 4+, flexoexentension foot 5- bilateral. At the sensitive level, it denies alterations. Osteotendinous reflexes ++ bi- y bilateral tricipital, ++ bilateral styloradial, left patellar ++, right patellar +, achilles + bilaterally, plantar cutaneous flexor bilateral. He is able to stand up independently and walk with support. It has recommended walker and in principle it has not been considered a candidate for specific treatment by rehabilitation. Given the clinical stability, a decision was made to discharge home with follow-up in consultations.
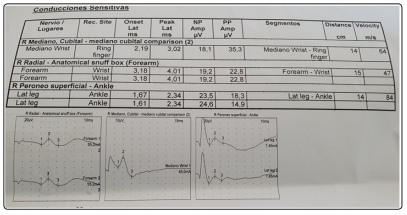
- Sensitive ENG of N. Peroneus sensitivo right and left (PES) N. sural dcgho and izq. N. Radial right, ulnar right and median right.
- ENG motor of N. Peroneal right and left (CPE). N. Right motor tibial (CPI). medium right motor. F waves reflection H.
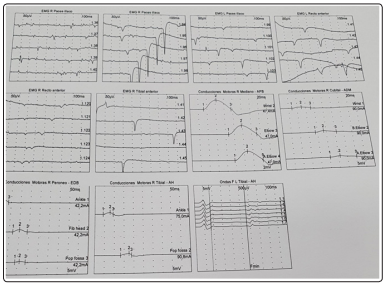
- Conventional EMG of the rectus femoris, vastus lateralis, tibialis anterior, peroneus longus, pedium, right medial calf muscles and left.
- Sensitive ENG and MMSS motor
- Radial sensitive right. : Normal, no drop in amplitude with preservation of latencies and VC.
N. ulnar sensitive right: Normal, no drop in amplitude with preservation of latencies and VC.
- Medium sensitive right. : Normal, no drop in amplitude with preservation of latencies and VC. N median right. Potential is obtained with moderate latency delay on the right side and no loss of sensory amplitude. A comparison of interpeak latencies between 4th median-ulnar finger, greater than 0.35 msec, is obtained. Specifically the current difference is 1.2 msec. on the right Median amplitudes decreased. Signs of severe focal segmental demyelinating and axonal lesion, compatible with DCHO CTS.
Severe with data of neuropraxia without associated axonotmesis.
• Mixed ENG: wrist-elbow of right median nerve. normal .no drop in the amplitude of the PRMixto and delay in its conduction speed.
• Middle right motor: proximal and distal amplitude drop, latencies preserved, no conduction block. VCM .: preserved.
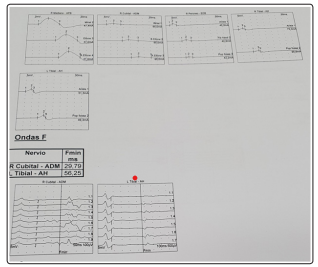
• WAVE F of the medium right motor. - With less than 50% persistence and latency lag.
• Right motor ulnar: proximal and distal amplitude drop, latencies preserved, no conduction block. VCM .: preserved.
• CUBITAL F WAVE RIGHT. : Right motor with less than 50% persistence and latency lag.
Sensitive ENG and MMII motor SNAP abd CMAP:
- SNAP -Peroneo sensitive right. : Normal, no drop in amplitude with preservation of latencies and VC.
- SNAP - Peroneo sensitive left. : Normal, no drop in amplitude with preservation of latencies and VC.
- SNAP -N. SURAL SENSITIVE RIGHT AND LEFT. : NORMAL.-
• Right motor CPE.CMAP : At the foot muscle level. Proximal and distal amplitude drop, latencies preserved, no conduction block. VCM .: preserved. Current absence of motor conduction block, no temporary potential dispersion, no increase in distal latency more than 125% of ULN. F WAVE of the right motor peroneal bone. : with more than 50% persistence and no latency delay.
CPE motor left. CMAP: At the foot muscle level. Proximal and distal amplitude drop, latencies preserved, no conduction block. VCM.: preserved. Current absence of motor conduction block, no temporary potential dispersion, no increase in distal latency more than 125% of ULN. F WAVE of the right motor peroneal bone. :with more than 50% persistence and no latency delay.
Right and left motor CPI CMAP:. Proximal and distal amplitude drop, latencies preserved, no conduction block. VCM .: preserved.F
WAVE of the right motor peroneal bone. : with less than 50% persistence and no latency delay. WAVE F of the right TP. - With less than 50% persistence and latency lag.
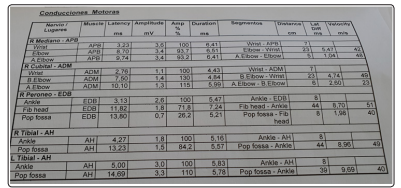
IN THIS PATIENT, LOW AMPLITUDE OF CMAP IS OBSERVED, (THERE IS A DROP IN AMPLITUDE GREATER THAN 80% IN MORE THAN 2 MOTOR NERVES), INEXCITABILITY OF SOME OF THE MOTOR NERVES, NO CONDUCTION BLOCKS ARE OBSERVED, WHICH COULD BE REVERSIBLE (REVERSIBLE MOTOR DRIVING BLOCK MAY BE PRESENT IN AMAN AND AMSAN) SENSITIVE POTENTIALS (SNAP) COME OUT NORMAL IN THE SAME SEGMENTS OF THE MOTOR NERVE, SIGNS OF ACUTE DENERVATION ARE OBSERVED, proximal and distal 1-3 months). , predominantly proximal to LEVEL OF MUSCLES INTERVATED BY THE FEMORAL NERVES, tibial nerve and right and left peroneal nerves. that speak in favor of acute-subacute axonal degeneration. IT HAS ALSO BEEN OBSERVED, slight alterations in late responses, non-distal temporal dispersion, absence of conduction block, and a pattern of preservation of the sural and superficial peroneal nerves. Data compatible with the pure axonal motor form of GBS. AMAN in subacute stage (1 month) without reversible conduction blocks. AMAN has a spectrum that ranges from reversible conduction failure, with a more favorable course, to axonal degeneration, with a worse prognosis. In this case, a sign of proximal and distal subacute axonal degeneration is observed in both MMII.
SUB-ACUTE NEUROGENIC PATTERN WITH DENERVATION (+ / ++++) (1-3 MONTHS) in muscles dependent on proximal and distal roots (from l2 to s3).
- AMAN has a spectrum that ranges from reversible conduction failure, with a more favorable course, to axonal degeneration, with a worse prognosis.
• ANPA or NAPA. Acute motor axonal neuropathy
• Moderate EPOC
The ENMG examination made it possible to establish the certainty diagnosis of acute motor axonal neuropathy in the face of the initial suspicion of an AIDP. Being able to discern and objectify through the ENG-.EMG, the motor neurographic differences between the AIDP (Acute inflammatory demyelinating neuropathy)and the NAPA (Acute motor axonal neuropathy).
View PDF