Author(s): Maria del Mar Espinosa, Roberto Pradanos del Pico and Manuel Dominguez*
In this work we are going to review the different alternatives and technologies currently existing in the field of 3D printing in the field of medical engineering. To do this, we will begin by commenting on the projects already developed and completed in our research group in Graphic and Design Engineering, related to medical topics. We will continue exposing the currently existing alternatives, that is, the state of the art; to then move on to propose alternatives for the future in our field.
3D printing takes place thanks to two fundamental factors: the development of plastic materials (specifically photopolymerizable resins) and the development of manufacturing systems with a high degree of automation.
In 1957, in the midst of the development of plastic materials, the French sociologist and philosopher Roland Barthes (1915-1980) commented:
“The hierarchy of materials has been abolished: one simple material replaces them all. The entire world can be made of plastic, and even life itself, since the manufacture of plastic aortas is already a reality.”
Indeed, the appearance of plastics has been very important both industrially and in medicine; and something similar is currently happening with 3D printing. But from there to whether plastics or 3D printing can “create life” is an abyss.
Without a doubt, the starting point of additive manufacturing must be placed on March 9, 1983, when, in the United States, the founder of the company 3D Systems, Charles W. Hull, managed to print a cup of tea in the first 3D printing system: the SLA-1 stereolithography apparatus, built by himself.
At UNED, we got on this train almost from the beginning, among other things because the technology took a few years to reach Spain, but in the nineties we already had our doctorate courses in rapid prototyping (that's what it was called then), and our publications [1].
It should be noted that from the first moment solid pieces began to be printed, among which were bones, but it is not until very recently that flexible materials have been printed on a regular basis,
undoubtedly due to the reduction in costs and the appearance of the RepRap phenomenon [2].
Indeed, a very important milestone in the spread of 3D printing is the RepRap movement, started by Adrian Bowyer in 2004 [3]. It is interesting to comment here that, although it is already known that the RepRap phenomenon has played, and is playing, a very important role in the development of additive manufacturing, at first it was not accepted by the academic community, considering it a minor issue. Only a few years later the movement was accepted, but not as a phenomenon in itself but rather under the approach of a machine that could manufacture itself, something that every manufacturing professional knows has been feasible since the 19th century, with milling machines.
At UNED we already did our bit in this chain with the design and manufacture of the Azara 3D printer (Figure 1) in 2011 [4].
Figure 1: Azara 3D Printer, Designed in UNED
In our research group, apart from other minor initiatives, two important projects have been developed.
Project Title: Obtaining prototypes through 3D printing for use in the design and manufacture of dental prostheses
Participating Entities: National University of Distance Education, Aragoneses Dental Group, University-Business Foundation, Madrid.
Duration, from: October 2011 to: December 2013
As a result of this project, apart from the interesting contributions achieved for the Aragoneses Dental Group and its patients, the following publication has been achieved:
Authors: Jiménez M., Romero L., Domínguez M., Espinosa M.M.
Title: Rapid prototyping model for the manufacturing by thermoforming of occlusal splints [5]
Place of publication: Rapid Prototyping Journal.
Volume: 21 (1) Pages, initial: 56 final: 69 Date: 2015
This paper has been selected by the journal’s editorial team as the Outstanding Paper in the 2016 Emerald Literati Network Awards for Excellence.
This project aims to obtain dental splints with highly automated procedures (Figure 2).
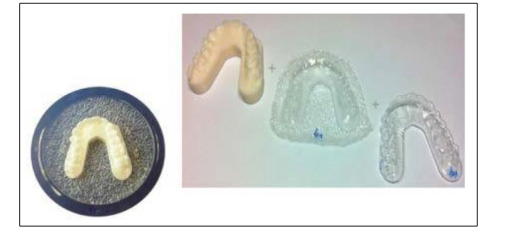
Figure 2: Dental Splints
In the development of the project we encountered many difficulties, among which we can highlight the step caused by the layer height in the printed piece (Figure 3).
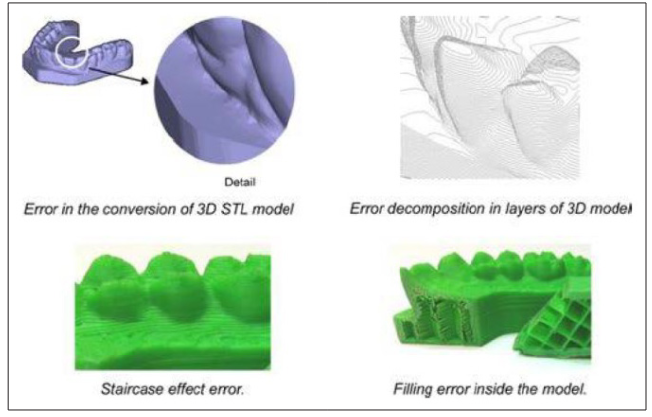
Figure 3: Problems in Obtaining Splints through 3D Printing
The final result, despite the difficulties, was highly satisfactory (Figure 4).

Figure 4: Tests on Patients of the Obtained Splints
Project Title: Obtaining prototypes through 3D printing for use in the design and manufacturing of master models with geometries similar to those of dental implants and reusable nuts that can be used in prostheses in dental implantology
Participating Entities: National University of Distance Education, Dentalmill s.l., University-Business Foundation. Madrid
Duration, from: October 2012 to: December 2014
As a result of this project, apart from the interesting contributions achieved for the Dentalmill Group and its patients, the following publication has been achieved:
Authors: Romero L., Jiménez M., Espinosa M.M., Domínguez M.
Title: New Design for Rapid Prototyping of Digital Master Casts for Multiple Dental Implant Restorations [6]
Volume: 10(12) Pages: 0145253-13 Date: 2015
Place of Publication: PLOS ONE.
This project took a step forward in automating the process by incorporating a scanner that captured the geometry of the patient, which in this case was an edentulous or almost edentulous patient (Figure 5).

As a result of this process, geometry of the mouth of the patient and the precise position of the implants is obtained (Figure 6).
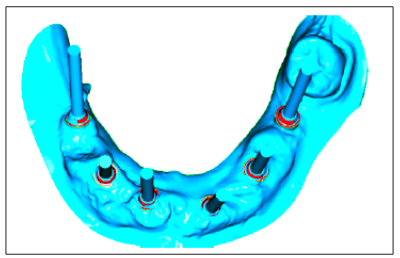
Figure 6: Image Obtained after Scanning
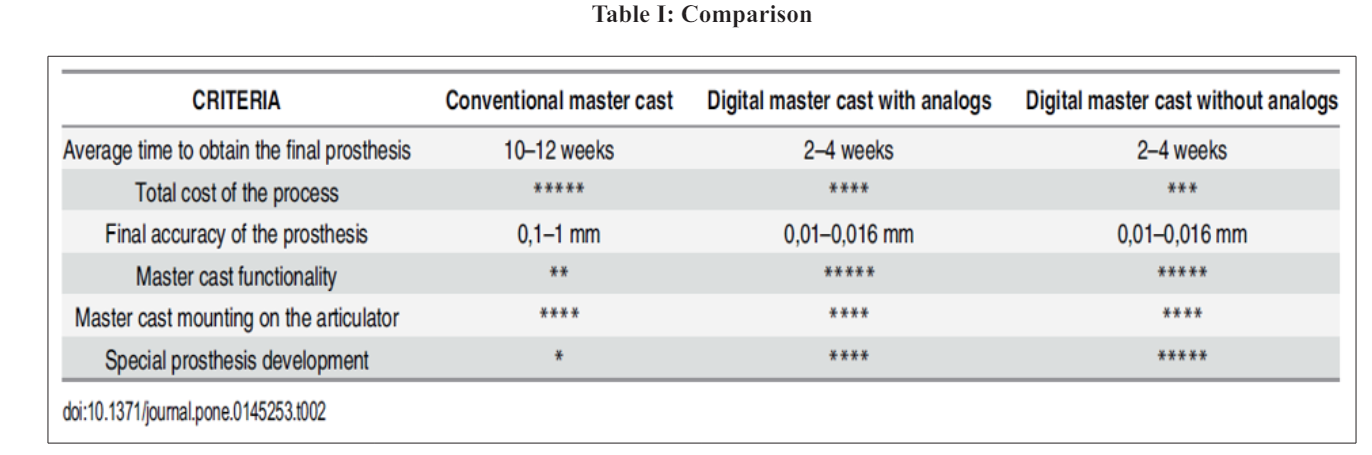
One of the advances in the design of the master model was the adoption of standard removable elements, which significantly reduced the cost and delivery times of the prosthesis (Figure 7).
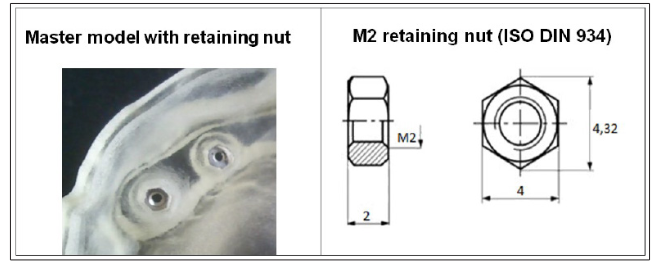
Figure 7: Use of Standard Pieces
Figure 8 shows images of the obtained results, and table I shows the comparative study with traditional methods that provided, as indicated, significant reductions in both cost and delivery times.

Figure 8: Obtained Results
A normal 3D printing process starts with the geometric modelling of what you want to build, and then cuts it into layers. These logical layers are sent to the machine that physically builds these layers to obtain a tangible reality that is a replica of the logical reality initially created.
In the field of medicine, it is normal not to start from geometric modelling but from a scan of the external geometry (by photogrammetry or laser) or the internal geometry.
One of the advantages of the current situation regarding 3D printing in medicine is how advanced the scanning system is. Basically, there are two alternatives to obtain internal geometries: magnetic resonance and computed tomography, which allow layer by layer to obtain the structure of the soft materials, in one case, or the hard materials, in the second (Figure 9).
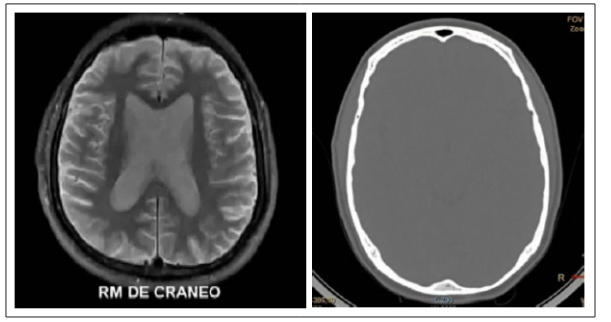
Figure 9: Magnetic Resonance and Computed Tomography
One of the advantages that provide this method is that it is feasible to work without having to generating the stl file, being able to directly generate the G code that 3D printing machines normally require.
Obtaining the digital geometry of anatomical parts requires, therefore, an image capture system and appropriate software to transform the information into something printable. There are basically two capture systems, as indicated: computed tomography (CT) and magnetic resonance (RM). Their operation is different, and therefore one or the other may be more appropriate depending on what you want to build. CT is a snapshot of conventional x-rays, which leaves the bone structure very well defined and is ideal if we want to print bone. RM works by creating a magnetic field, without exposure to radiation, and allows different soft tissues to be distinguished very well. That is why it is used when you want to observe the brain mass, for example.
With the right software all these independent images are converted to 3D, and once that has been achieved, printing with materials without special biocompatibility requirements is relatively easy. Simply with the above we already have the possibility of printing a three-dimensional model of a part of a specific human and “learning with it”.
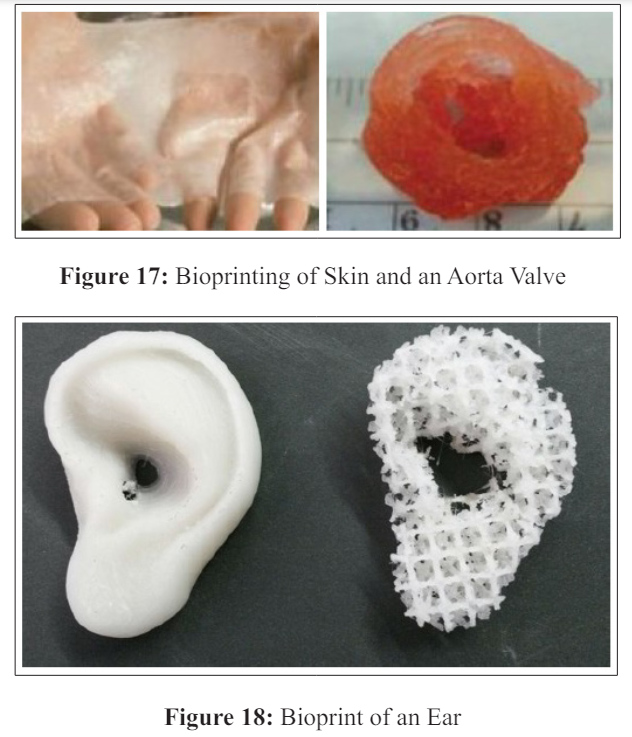
3D printing has two approaches: printing non-living, biocompatible and sometimes biodegradable materials; and the printing of living elements (cells). The first case has already been widely studied and the advances are important. As for the second, 3D printing of living cells, bioprinting, it is probably the object of most research projects today.
Bioprinting normally requires the deposition of cells at the same time as the support element, or matrix, is deposited. This matrix, the place where the cells will grow up and from which they will extract food, may be liquid, normally called biological ink, pasty, rigid solid or elastic solid (Figure 10). All of them, and especially solid materials, may or may not be biodegradable.
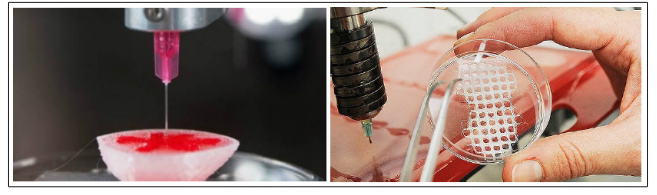
Figure 10: Printing of Biological Ink and Solid Structures
The biodegradation is an added factor in this technology. Since this biodegradation occurs too quickly, the expected results will not be obtained; but if it is done too slowly, there is a possibility that the structure will prevent the development of the cells, which in the end will not obtain the desired results either.
This area covers the generation of physical organs and bones for study (Figure 11), which can be very useful in preparing for surgeries, for example.
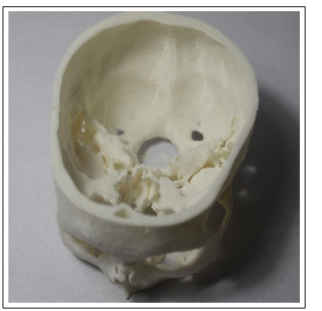
Figure 11: Skull Reproduction in ABS
Something very interesting in this sense is that it has been possible to reduce surgery time when they are complicated since the surgeon and his entire team can study the intervention to find the best possible approach and foresee the complications that will be found and how can be resolved. In short, it allows the operation to be better planned, reducing time in the operating room and, therefore, reducing the risks of prolonged anaesthesia or contaminations.
There are many examples of the use of 3D printing in this sense, such as capturing the geometry of a tumour or the scanning and subsequent reconstruction of two conjoined twins joined by the skull, which had a large part of their vessels in common. The creation of the model, with different colours for the skull (transparent) and the vessels (in red) allowed the surgery to be rehearsed in advance and finally completed successfully.
The next point to advance is the use of appropriate materials to the use that is going to be given to it. The first thing has been to create biocompatible printable materials, that is, that do not pose toxicity to the body, nor do they make the immune system react more than admitted (which would lead to rejection) and that resist physiological conditions (pH, temperature or stress).

Figure 12: Use of 3D Printing in Complex Surgeries
In this sense, the most notable are the prostheses that replace a bone or a joint. Jaw, hip or shoulder prostheses have been made successfully. The possibilities are multiple and allow millimetric adjustment to reality. For example, fragments of skull bones that were fractured have also been made (Figure 13).
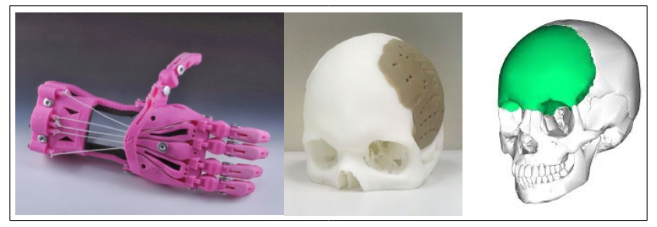
Figure 13: Prosthesis
Biodegradable structures have also been created. A common example is a trachea and bronchus implant in a baby with a congenital problem. The objective of the implant was to allow air to pass while the baby were small, but once the baby grow up the implant would no longer be necessary, hence the interest in it being biodegradable, avoiding a second surgery.
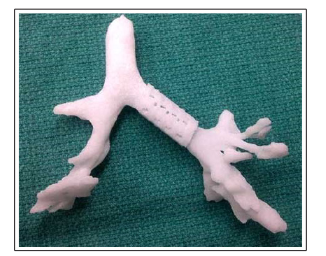
Figure 14: Biodegradable Prostheses
The development of 3D printing does not stop here. The next step is that is now called “bio-printing”, which is the living cells and tissues printing [7,8]. Its interest is due, mainly, to the scarcity of organs available for transplant and the possibility of avoiding rejection, if the necessary organ can be printed with the own cells of the patient. Its use in research into new drugs is also very important, to reduce the use of laboratory animals. In this sense, the example of 3D printing of a pulmonary bronchus can be used to investigate the antihistamine capacity of drugs. You can see the contraction of the bronchus muscles due to the addition of histamine, which reproduces a real-life asthma attack. By maintaining this contractile capacity of the bronchial muscles we can test whether a certain medication that is going to be put on the market is effective or not, without the need to test it on animals, and thus avoiding failures due to differences between species.
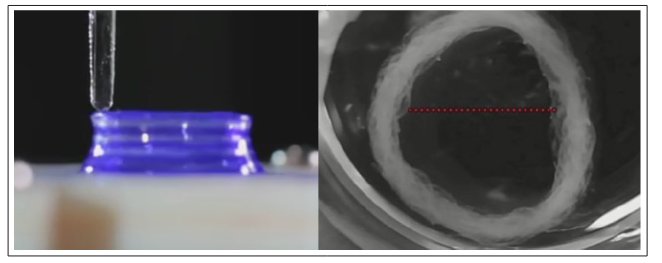
Figure 15: 3D Printing of a “Live” Pulmonary Bronchus
Bio-printing faces a series of challenges that other printing formats do not have:
The complexity of human tissue. Reproducing a tissue, no matter how simple it may be, means knowing each of its components, the function of each of them and their relationships. Skin is an example, because it is often talked about as if it were something easy to reproduce. In the image (Figure 16) we see, from top to bottom, the keratin, in bright pink, secreted by the superficial cells of the epidermis; the epidermis, in purple, with superimposed layers of cells and hair follicles (which project inward); and the dermis, in light pink.
Building this entire structure, with the different cell types and support molecules, is ideal for making a perfect 3D print, but it is not done due to its technical difficulty.
The procedure currently used consists of printing stem cells in layers of matrix. The matrix has a structural, connective and nutritional function. Polymeric materials, natural or synthetic, are usually used, such as alginate or collagen.
Stem cells are those capable of self-replication and becoming a differentiated type of cell. Embryonic stem cells have the ability to differentiate into any cell in the body and are therefore called pluripotent, but they have the drawback, in addition to the ethical issue, that the factors that cause them to become one cell or another are difficult to control. In adults there are “adult” stem cells, which are responsible for the regeneration of damaged tissues and replacement due to aging. Adult stem cells have a limited ability to differentiate, depending on where they are located. Blood stem cells, generated primarily in the bone marrow, can give rise to all blood cell types, but they cannot become an epithelial cell.
Stem cells are extracted from the patient, grown up in the laboratory, and included in the matrix where an adequate cell density is achieved. The mixture is then printed with the desired shape, and it is left for a while at the appropriate temperature for the cells to differentiate and create connections between them.
Another problem that bioprinting faces is the formation of vessels in tissues, which should allow nutrition and waste removal. In small skin implantations, for example, there would not be a big problem because the vessels of the surrounding healthy skin would infiltrate the implanted tissue until they completely irrigate it. The problem is in the creation of organs. It is not yet possible to create a liver, but it is possible to decellularize an existing liver and print in it the cells multiplied in the laboratory. The structure of a liver is used and there are no rejection problems.
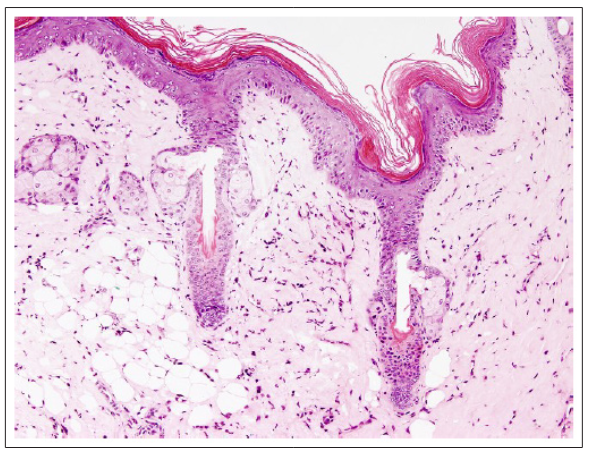
Figure 16: Skin Section
Bioprinting is in laboratories for more than ten years, and some more or less complex structures have been printed, such as ears, heart valves and even bladders. Although research has been going on for years, the impression of functional kidneys or other complex organs has not yet been achieved.
Finally, mention the in vivo printing, which is made on the own patient body. The machine scans the depth of the wound and then fills it with a material that allows the surrounding skin to regenerate, as if creating bridges for the regenerating skin cells to pass through (Figure 19).

Figure 19: In vivo Printing
3D printing in the medical sector faces two important barriers:
On the one hand, the dimensions of the cells (ranging from 0.2 to 10 μm) are at the limit of the positioning precision of the machines (around 15 μm).
On the other hand, we must delve deeper into the system of functioning and reproduction of cells, since they are living materials, and the conditions of the environment and the structures themselves make the work very delicate.
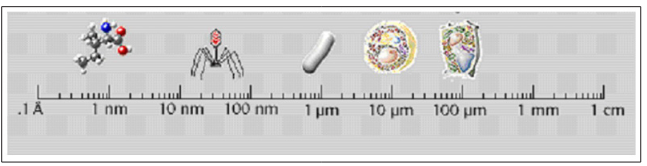
Figure 20: Cell Size
But not all efforts should be focused on therapeutic procedures. Many times it is better to work on prevention, which in the end gives better results. Therefore, the food factor must be taken into account, and 3D printing should not be left out [9].
What does not make sense is to develop cutting-edge technology to obtain pizzas and hamburgers. Work must be done on this technology in the food fields that have yet to be developed. In this sense, a 3D food printing system can dose quantities very well, it can produce foods that include drugs, and it can obtain attractive geometries for children and the elderly, and many more alternatives that are yet to be discovered.
Without a doubt, 3D printing in the field of medicine will give rise to many projects and publications in the coming years. To do this, it is necessary to form multidisciplinary teams where there are doctors, biologists or veterinarians working in collaboration with chemists, engineers and technicians in general.
On the other hand, it is important to improve techniques to cure sick patients or patients suffering from a problem. But it is no less important to work on prevention, which is why nutrition is essential and, in this sense, it is probable and desirable that the coming years will bring advances in 3D printing in food that are along those lines.
1.Canedo-Arguelles EL, Domínguez M (1999) Estado actual del prototipado rápido y futuro de este. in Actas del XI Congreso Internacional de Ingeniería Grafica 3: 1242-1255.
2.Rodríguez L, Romero L, Domínguez M (2016) Analysis and Validation Model of Design Proposals Through Flexible Prototypes Modelo de análisis y validación de propuestas de diseno mediante prototipos flexibles. Dyna 91: 502-506.
3.Sells E, Smith Z, Bailard S, Bowyer A, Olliver V (2007) RepRap: The Replicating Rapid Prototyper. Maximizing Customizability by Breeding the Means of Production. in Proceedings of the 2007 World Conference on Mass Customization & Personalization (MCP).
4.Guerrero de Mier, M del M Espinosa (2014) Progress in RepRap: Open Source 3D Printing Avances en RepRap: Impresión 3D de código abierto. Dyna 89: 34-38.
5.Jiménez M, Romero L, Domínguez M, M del M Espinosa (2015) Rapid prototyping model for the manufacturing by thermoforming of occlusal splints. Rapid Prototyp. J 21: 56-69.
6.Romero L, Jiménez M, M del M Espinosa, Domínguez M (2015) New Design for Rapid Prototyping of Digital Master Casts for Multiple Dental Implant Restorations. PLoS One 10: e0145253.
7.Zhu W, Ma X, Gou M, Mei D, Zhang K, et al. (2016) 3D printing of functional biomaterials for tissue Engineering. Curr. Opin. Biotechnol 40: 103-112.
8.Murphy SV, Atala A (2014) 3D bioprinting of tissues and organs. Nat. Biotechnol 32: 773-785.
9.Sun J, Zhou W, Huang D, Fuh JYH, Hong GS (2015) An Overview of 3D Printing Technologies for Food Fabrication. Food Bioprocess Technol 8: 1605-1615.
View PDF