Author(s): Nurfareha Mohd Hatta*, Noor Kaslina Mohd Kornain and Norhafizah Saifudin
Giant cell tumour of soft tissue (GCT-ST) are rare soft tissue tumours, with the first case reported in the 1970s. Involvement of the head and neck region, particularly in the nasal cavity is extremely uncommon. GCT-ST are considered the bone counterpart given the striking histological and immunohistochemical resemblance. Despite that, GCT-ST and GCT of bones are genetically distinct. Microscopically, GCT-ST exhibit numerous osteoclast-type multinucleated giant cells within a background of mononuclear stromal cells. They are locally aggressive and can potentially recur. It is important to distinguish GCT-ST from giant cell reparative granuloma (GCRG) as they both share similar clinical and morphological characteristics, however, they have different treatment modalities. We report a case of GCT-ST occurring in the nasal cavity, an unusual site of presentation.
Giant cell tumour of soft tissue (GCT-ST) are exceptionally uncommon tumours, with the first case reported in 1972. 70% of these tumours are usually found in the superficial soft tissues of the extremities. A small percentage of the tumours, about 7%, arise in the head and neck region. To date, they are only 13 GCTST of the head and neck reported in the literature reviews, with 2 cases involving the nasal cavity and nasopharynx. GCT-ST predominantly affect patients in the fifth decade of life and they can be seen in broad age groups, with no sex predilection. It is thought that GCT-ST is the counterpart of GCT of bones as they bear similarities morphologically and immunohistochemically [1,3]. However, they are genetically different despite their resemblance [3,4]. Studies have shown that H3F3A gene mutations are demonstrated in most GCT of bones. Based on Sanger sequencing done by Lee et al, no somatic mutation was detected in all 15 cases of GCT-ST, suggesting that GCT-ST and GCT of bones have different pathogenesis [4].
GCT-ST usually present with a painless well-circumscribed nodular mass with either a fleshy, reddish-brown or grey surface [1,2]. Microscopically, there are polygonal to spindled mononuclear stromal cells admixed with abundant osteoclasttype multinucleated giant cells, the latter showing diffuse CD68 immunoreactivity [1]. GCT-ST are locally aggressive with rare metastatic potential [1,3]. Few cases have been described to have locally recurred and metastasized to distant sites [1]. Complete surgical excision with free resection margin is considered the standard treatment approach, followed by a strict follow-up to monitor for tumour recurrence [1,3].
Giant cell reparative granuloma (GCRG), a benign non-neoplastic lesion initially described in 1953, is the most likely differential diagnosis. It is a reactive entity which occurs following a history of trauma or inflammation [5-7]. It is more prevalent among children and young adults, with a female preponderance. Mandible and maxilla are the most common sites with rare occurrences in the nasal cavity [6,7]. Its pathogenesis remains unknown [5]. GCRG is demonstrated histologically by the presence of osteoclastlike multinucleated giant cells concentrated around areas of haemorrhage, accompanied by mononuclear stromal cells and fibroblasts [5-7]. GCRG can be locally aggressive although they have no malignant potential. GCRG and GCT-ST have different treatment approaches; the former can be treated non-surgically [6,7].
We here report a case of GCT-ST of the left nasal cavity in a 45-year-old male in our facility
A 45-year-old Chinese gentleman, a chronic smoker and ex-drug abuser, presented to ORL clinic with a 6-month history of facial pain and heaviness, worsening for 3 months. He also complained of headache, left eye blindness, nasal congestion and stuffiness, reduced appetite and weight loss. He denied facial numbness, vertigo or tinnitus. He had his CT brain initially done at a private health care centre, which revealed a base of the skull lesion suspicious of sphenoid sinus carcinoma. On examination, his left pupil deviated toward the centre. His neurological examinations are all intact with no abnormality detected. His rigid endoscopy findings showed presence of necrotic tissue at the left nasal floor with copious foul-smelling mucopurulent pus. The left Fossa of Rosenmullar was unable to be visualized. The tissue biopsy was sampled at the necrotic tissue
He was subsequently admitted due to hyponatremia secondary to Syndrome of Inappropriate Anti-diuretic Hormone (SIADH). His CT Brain upon admission showed cerebral oedema. CT Neck, Thorax, Abdomen and Pelvis was also performed during his admission, confirming presence of a large sinonasal mass with marked regional infiltration into the adjacent structures and extensive bony erosion, especially at the base of skull. There is no evidence of distant metastasis seen.
Biopsy of his left nasal cavity showed uniformly distributed osteoclast-like giant cells within sheets of mononuclear stromal cells. The mononuclear cells have epithelioid to spindled appearance and exhibit bland round to oval nuclei, even chromatin distribution and small nucleoli. There is no significant nuclear atypia. Scattered mitotic figures are also seen, but no atypical forms are noted. The background stroma is vascularized with focal areas of necrosis observed. There is no identifiable bone or cartilage formation. Immunohistochemical stains revealed positivity for CD68 and Vimentin. CKAE is negative. The overall morphological features are consistent with giant cell tumour of soft tissue. The patient was then referred to the Oncology team for further treatment.

Figure 1: CT Scan shows a soft tissue attenuation in the left nasal cavity
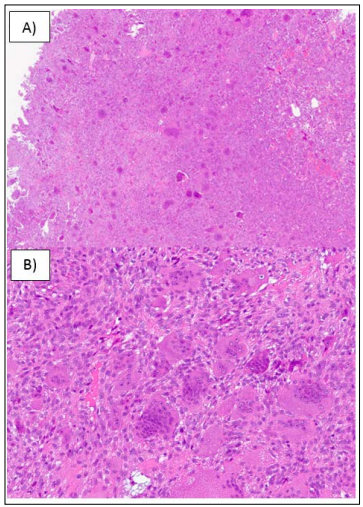
Figure 2: Histomorphological features of the giant cell tumour of soft tissue of the nasal cavity. A) Low power view of the tumour showing a cellular lesion with giant cells seen. B) High power view of the tumour demonstrating osteoclast-like multinucleated giant cells with surrounding mononuclear stromal cells infiltration
GCT-ST are considered the bone counterpart as they are morphologically and immunohistochemically similar [1,3]. They are commonly seen in the soft tissue of the extremities with rare incidence in the head and neck region, especially in the nasal cavity, paranasal sinuses or nasal septum [1,2,5]. GCT-ST originating from the nasal cavity has been reported in only one case, involving a female patient presented with frequent sinus infection and nasal obstruction [1]. Our case is a second case of GCT-ST involving the nasal cavity.
In our case report, our patient presented with facial pain, headache, left eye blindness, and nasal congestion. He was found to have a sinonasal mass with extensive regional infiltration and bone destruction. Biopsy from his left nasal cavity revealed numerous CD68-positive osteoclast-like multinucleated giant cells in uniform distribution with background sheets of epithelioid to spindled mononuclear stromal cells and increased vascular proliferation. He was diagnosed with giant cell tumour of soft tissue in the left nasal cavity
Regardless of the location, morphology remains a gold standard in the diagnosis of giant cell tumours of soft tissue. Immunohistochemical studies may serve as useful ancillary studies and they should not supersede the morphology features. CD68 immunoreactivity is not specific and its negativity does not preclude the diagnosis of giant cell tumours [3].
Giant cell reparative granuloma (GCRG), a benign entity is one of the important differential diagnosis and like GCT-ST, its involvement in the nasal cavity is very rare [5-7]. This lesion is believed to be a reactive process typically preceded by a history of trauma or inflammation. Frequently found in the maxilla and mandible, GCRG is classified according to the site of the lesion. Central GCRG affects bone, and peripheral GCRG affects only the soft tissues [6,7]. Both present with similar morphological features [6]. They are described as randomly distributed osteoclast-like giant cells near the haemorrhagic areas within a fibrous stroma. Associated reactive bone formation is usually seen. Despite its benign behaviour, GCRG is locally aggressive. However, GCT-ST poses a higher rate of recurrence [5-7].
GCT-ST also needs to be distinguished from giant cell variant of malignant fibrous histiocytoma, a high-grade soft tissue sarcoma. The latter shows randomly distributed bizarre multinucleated giant cells with marked nuclear atypia and atypical mitoses [3]. This tumour is now termed undifferentiated sarcoma as there is no identifiable lineage, therefore it is a diagnosis of exclusion [2].
There is no clear protocol regarding the specific management of GCT-ST. In most reported cases, complete surgical resection is the mainstay of treatment. A strict follow-up is recommended to look for any recurrence. Unresectable tumours have been treated with osteoclast-acting agents such as bisphosphonates and radiation therapy [3,5]. In our case, the patient’s lesion was not excised in view of its destructive nature and he was referred to the Oncology team for further management
We presented a case of a giant cell tumour of soft tissue arising in the nasal cavity, a second case reported in the literature, to the best of our knowledge. Further studies are encouraged to gain more insights and understanding of these rare giant cell tumours.
