Application of Prone Position Ventilation in Clinical Treatment of Patients with COVID-19
Author(s): CAO Ying, TIAN Kun, WEN Meng *
Based on the PIPOST tool to establish evidence-based issues, relevant domestic and foreign databases and websites were searched for clinical decisions, guidelines, evidence summaries, systematic reviews, recommended practices, and expert consensuses on the management of prone ventilation with acute respiratory distress syndrome. The retrieval time was from the establishment of the database to December 10, 2022, and the quality evaluation and evidence extraction of the literature that met the inclusion criteria were carried out. A total of 13 articles were included, including 1 clinical decision, 7 guidelines, 2 expert consensuses and 3 systematic evaluations [1-13]. 34 pieces of best evidence were summarized from 5 dimensions, namely pre-operation evaluation, operation implementation, end of prone ventilation, complication prevention and personnel organization management. The best evidence summarized in this study can provide a reference for clinical medical staff to implement prone position ventilation, but in clinical practice, it is necessary to select and apply evidence in a targeted manner in combination with specific circumstances, so as to improve the safety and therapeutic effect of prone position ventilation.
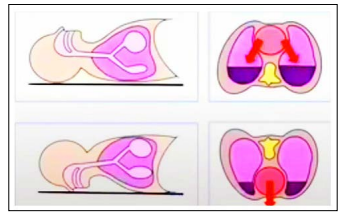
Prone position ventilation was used for acute respiratory distress syndrome before, and now it is widely used for the clinical treatment of novel coronavirus. It can effectively improve the patient’s blood oxygen saturation and the lung ventilation/blood flow ratio by turning over the bed, turning machine or artificial bare hand to make the patient breathe or mechanical ventilation in the prone position.
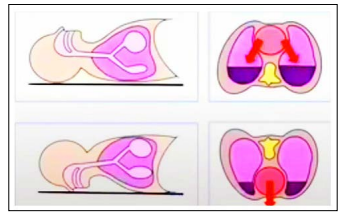
Figure 1: Principle of Prone Position Ventilation
What are the “Prone Position Ventilation”?
1. Mechanical ventilation in prone position under sedation and analgesia: in order to avoid some complications and reduce the discomfort of patients when receiving treatment, the whole process of sedation and analgesia will be closely monitored at the same time.
2. Ventilating in conscious prone position: It is applicable to all types of COVID-19 patients who are in a conscious state. They can turn over on their own or cooperate with turning over, and can call for help when breathing is difficult.
3. Modified prone position ventilation (large lateral position): It is applicable to some special patients, such as pregnant women, obesity, abdominal hypertension, tracheotomy, head and face injury, etc., which is not convenient for patients in conventional prone position.
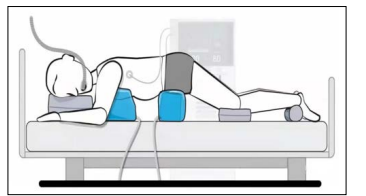
How to do “Prone Position Ventilation”? Prepare at least three pillows, one in front of the chest, one in the head, one in the ankle, and another under the belly of the patient with large stomach. Relax your shoulders and turn over once in 2 hours.
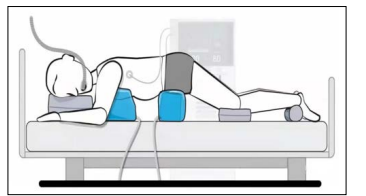
Figure 2: Prone position ventilation
Precautions for “Prone Position Ventilation”?
- The medical staff and your family will help you turn your face to the opposite side every 2 hours, and change the pillows to the opposite side, while modifying the complications such as injury. The daily target time of prone position is 12 hours.
- The prone position ventilation is simple and easy to operate. The treatment time varies according to the needs of the patient. We often use the step-by-step method to gradually extend the treatment time.
- The catheter shall be properly fixed to avoid pressure, distortion and excessive pulling of the tube in prone position.
- Please pay attention to observation with your family and report to the medical staff in case of any abnormality.
- For anxiety patients, anti-anxiety drugs can be used to improve tolerance according to the doctor’s instructions.
- The target time of treatment for pregnant women is 2 hours per day, and the treatment time of prone position can be shortened or extended according to the actual situation of patients.
Contraindications of “Prone Position Ventilation”.
- Risk of airway obstruction
- Respiratory failure caused by cardiogenic edema
- Dyspnea, respiratory rate ≥ 40 times/min
- SpO 2 cannot achieve accurate and continuous monitoring
- Difficulty or limitation in autonomous movement, unable to tolerate prone position
- The skin is damaged or injured and cannot tolerate prone position
- There are unstable fractures of cervical spine and spine that need to be fixed
- Glaucoma or other extremely elevated intraocular pressure
- There is intracranial hypertension caused by craniocerebral injury
- There is a high risk of pulmonary embolism
References
- Fan E, del Sorbo L, Goligher EC, Hodgson CL, Munshi L Walkey AJ, et al. (2017) An Official American Thoracic Society/European Society of Intensive Care Medicine/ Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome [J] Am J Respir Crit Care Med 195: 1253- 1263.
- Cho YJ, Moon JY, Shin ES, Kim JH, Jung H, et al. (2016) Clinical practice guideline of acute respiratory distress syndrome [J] Tuberc Respir Dis (Seoul) 79: 214-233.
- Respiratory Critical Care Medical Group (2016) Respiratory Society, Chinese Medical Association. Mechanical ventilation guideline for patients with acute respiratory distress syndrome (trial) [J] Natl Med J China 96: 404-424.
- Malhotra A (2022) Prone ventilation for adult patients with acute respiratory distress syndrome https://www.uptodate.com/contents/prone-ventilation-for-adult-patients-with-acute-respiratory-distress-syndrome.
- Papazian L, Aubron C, Brochard L, Chiche JD, Combes A, et al. (2019) Formal guidelines: management of acute respiratory distress syndrome [J] Ann Intensive Care 9: 69.
- Dalmedico MM, Salas D, Oliveira AM, Baran FDP, Meardi JT, et al. (2017) Efficacy of prone position in acute respiratory distress syndrome, overview of systematic reviews [J] Rev Esc Enferm USP 51: e03251.
- Ball C, Adams J, Boyce S, Robinson P (2001) Clinical guidelines for the use of the prone position in acute respiratory distress syndrome. Intensive Crit Care Nurs 17: 94-104.
- Hashimoto S, Sanui M, Egi M, Ohsimo S, Shiotsuka J, et al. (2017) The clinical practice guideline for the management of ARDS in Japan. J Intensive Care 5: 50.
- Griffiths MJD, McAuley DF, Perkins GD, Barrett N, Blackwood B, et al. (2019) Guidelines on the management of acute respiratory distress syndrome .BMJ Open Respir Res 6: e000420.
- Subgroup of Critical Respiratory Diseases (2020) Chinese Society of Critical Care Medicine, Chinese Medical Association. Standardized protocol of prone position ventilation in patients with acute respiratory distress syndrome. Chin J Intern Med 59: 781-787.
- Mitchell DA, Seckel MA (2018) Acute respiratory distress syndrome and prone positioning. AACN Adv Crit Care 29: 415-425.
- Bloomfield R, Noble DW, Sudlow A (2015) Prone position for acute respiratory failure in adults . Cochrane Database Syst Rev 2015: CD008095.
- Munshi L, del Sorbo L, Adhikari NKJ, Hodgson CL, Wunsch H, et al. (2017) Prone position for acute respiratory distress syndrome. A systematic review and meta-analysis . Ann Am Thorac Soc 14: S280-S288
View PDF