Author(s): Sanpreet Singh Sachdev, Tabita Joy Chettiankandy, Ashish Sunilkumar Sarda, Om Dnyanadev Kharat and Suleka Ranganath
Odontogenic keratocyst (OKC) has always been a subject of interest for researchers and clinicians, owing to its unique pathogenesis, aggressive clinical behavior and association with syndromes. Majority of OKCs occur in the mandibular posterior region, and sporadic type of cysts have a predilection to occur in males and in patients of older age groups. The present article reports a case of sporadic OKC presenting in a relatively unusual manner, occurring in the maxillary anterior region of a young female patient. Unlike other reported cases that found OKC prior to commencement of orthodontic treatment, herein it had possibly occurred as a complication of the orthodontic treatment. The article also depicts characteristic microscopic features of OKC such as uniform parakeratinized lining with multiple infoldings, basal palisading, areas of interface separation between the lining and capsule. Disrupted lining with severe inflammatory cell infiltrate in the capsule was indicative of secondary infection.
Odontogenic keratocyst (OKC) is a developmental odontogenic cyst that exhibits parakeratinized epithelium lining the cystic lumen. Epidemiologically, OKC is quite rare accounting for about 10% of odontogenic cysts in Indian population [1]. The cyst has always been a subject of interest for researchers and clinicians, owing to its unique pathogenesis, aggressive clinical behavior and association with Nevoid basal cell carcinoma syndrome. There are two peaks of occurrence with syndromic OKCs being more common in the second or third decade, and sporadic OKCs being more common in patients of age 50 years and above [2].
Radiologically, OKCs present as a well-defined uni- or multi-locular radiolucency and may occur as any of the four types- replacemental, envelopmental, extraneous, or collateral [3]. Histologically, the cyst displays a regular parakeratinized epithelial lining of 6-12 layers of cells, without rete ridges. A characteristic microscopic feature of OKCs is the presence of palisaded basal layer of tall columnar cells exhibiting hyperchromatic nuclei with reversed polarity [2].
OKC displays a male predilection (M: F = 1.6:1) and in about 80% cases, occurs in the mandibular posterior region [2, 4]. The cyst tends to proliferate in between the bony trabeculae without causing much expansion of the bone until advanced stages. Consequently, it is rather commonly identified incidentally during routine radiographic examination for other reasons such as dental extractions, endodontic or orthodontic treatment [5].
In this context, the present case of a sporadic OKC presented in a relatively unusual manner occurring in the maxillary anterior region of a young female patient. Unlike other reported cases that found OKC prior to commencement of orthodontic treatment, herein it had possibly occurred as a complication of the orthodontic treatment.
A 19-year-old female was referred to our institute for investigation of pain in the maxillary right canine region.
A history of impacted canine was elicited, which was extruded over the past three years by surgically exposing the canine and taking anchorage of maxillary right first molar. The orthodontic treatment was performed in a private dental clinic and before its commencement, a cone beam computed tomography scan was performed for the patient, in which no evidence of disease was detected. However, since the past eighteen months, patient noticed intermittent pain in the maxillary right canine region. The maxillary right premolars and molars were endodontically treated by the private practitioner. A swelling developed in theregion, about a month ago, for which the patient was referred to our institute.
At present, extraoral examination of the patient was unremarkable. Only a slight distal rotation and palatal tipping of the maxillary right canine with erythema of marginal gingiva could be observed upon intra-oral examination. A broken molar band was noted around the maxillary right first molar. Clinically, the pain was thought to be originating as a result of maxillary sinusitis and radiographic investigation of the maxilla was planned.
Orthopantomogram revealed an ill-defined unilocular radiolucent lesion between the maxillary right canine and lateral incisor. A slight radiopaque haziness was also noted in the right maxillary sinus. CBCT revealed a cystic lesion having corticated borders between the two teeth along with elevation of the floor of the maxillary sinus (Figure 1). The dimensions of lesion were 25 x 36 x 9 mm. The differential diagnosis after radiographic examination included radicular cyst, odontogenic keratocyst, fissural cyst, unicystic ameloblastoma, and adenomatoid odontogenic tumor.
A complex mucoperiosteal flap was reflected from the maxillary right central incisor to the third molar region. The cyst was exposed by removing the bone overlying the maxillary sinus. The contents of the cyst were aspirated which exhibited a bloodtinged yellowish white cheesy material (Figure 2A). A window was created and complete enucleation in toto was carried out by means of curette and mosquito forceps (Figure 1). Antral cavity was irrigated with a 5% povidone iodine solution and 3-0 vicryl sutures were placed.
Macroscopically, the lesion had overall dimensions of 34 x 26 x 7 mm. On cutting transversely, a cystic lumen lined by a cystic wall of 3 mm thickness was noted, which displayed occasional thickening in some areas (Figure 2B). The inner side of the cystic capsule was smooth, devoid of any ingrowths into the lumen.
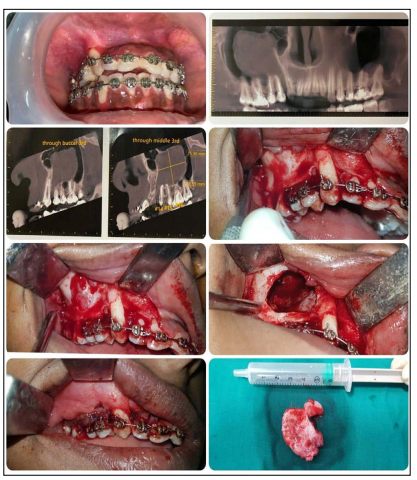
Figure 1: Comprehensive Depiction of the Surgical Removal of Cyst in Toto
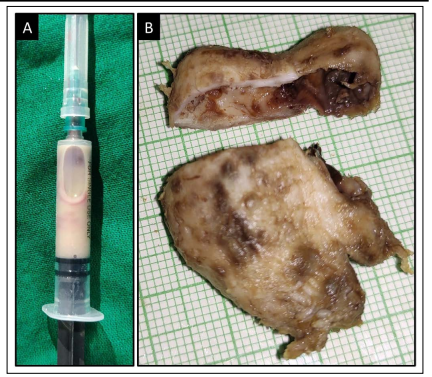
Figure 2: A) Blood-Tinged Yellowish White Cheesy Aspirate;
B) Transversely Cut Gross Specimen Exhibiting Uniform Cystic
Wall with Focal Thickening
Histopathological examination showed that the cystic lumen was lined by a cystic lining and capsule thrown into multiple folds towards the lumen (Figure 3A). The interface between the cystic lining and the cystic capsule was flat and showed separation in some areas (Figure 3B). The lining comprised of parakeratinized stratified squamous epithelium of 6 to 10-layer thickness, correspondingly measuring about 60-100 μm (Figure 4A). The tall columnar cells of the basal layer consisted of hyperchromatic nuclei, which were polarized away from the basement membrane, exhibiting palisaded or tombstone appearance.
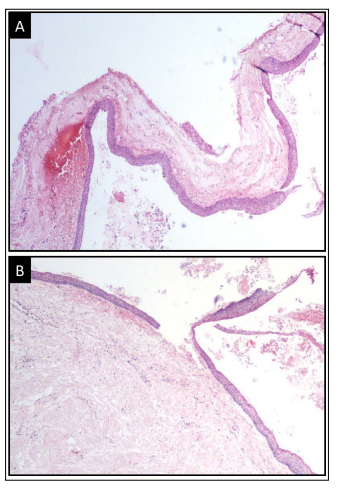
Figure 3: A) Uniform Stratified Squamous Lining Exhibiting
Multiple Infoldings;
B) Separation of the Lining from Underlying
Capsule in Some Areas. (H and E, Original Magnification X40)
Just below the lining epithelium, the cystic capsule demonstrated a band of loose bundles of collagen fibers with presence of apparent vacuolations between the fibers, indicative of glycosaminoglycanrich zone (Figure 4B). Remainder of the cystic capsule comprised of parallelly arranged, dense fibrous bundles interspersed with mature fibroblasts. In some areas, the cystic lining was disrupted. In these areas, the capsule exhibited severe chronic inflammatory cell infiltrate, chiefly comprising of lymphocytes and plasma cells, in a background of loose, oedematous collagen fiber bundles and engorged blood vessels (Figure 5).
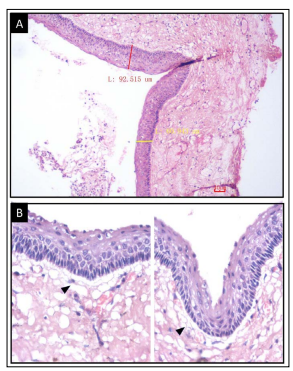
Figure 4: A) Uniform Parakeratinized Epithelial Lining of 6-10 layers (H and E, Original Magnification X100); B) High Power View Exhibiting Palisaded Appearance in the Basal Layer and Juxtaepithelial GAG-Rich Zone (Arrowhead). (H and E, Original Magnification X400).
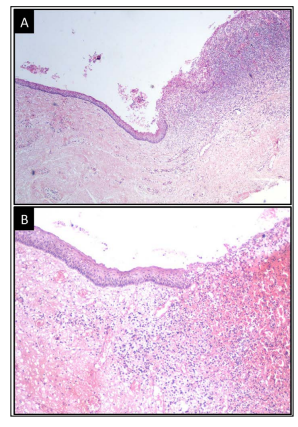
Figure 5: Disrupted lining Epithelium in Areas with Severe Inflammatory Cell Infiltrate in the Cystic Capsule in A) H and E, original magnification X40; B) H and E, original magnification X40.
The histopathological features were undoubtedly characteristic of an odontogenic keratocyst, with secondary infection, which was imparted as the final diagnosis. The orthodontic brackets were removed and uneventful healing of bone was noted four months after the surgery. Uprighting of the maxillary canine and lateral incisor was suggested to the patient. No evidence of disease or recurrence was noted after a follow-up of 18 months (Figure 6).
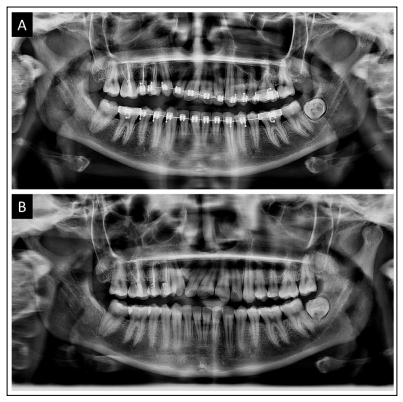
Figure 6: A) Orthopantomogram after a 12-month follow-up
exhibiting adequate bone healing;
B) No evidence of disease
after removal of orthodontic brackets at 18-month follow-up visit.
Various types of cells such as cell rests of Serres, reduced enamel epithelial and basal layer of surface epithelium overlying the jaws have been demonstrated to serve as origin for OKCs [2]. However, the exact mechanism triggering the formation of lesion from these cells is not clearly known. Various etiological factors such as genetic mutations, trauma, radiation, or infection have been suggested for stimulation of the cells of origin [2, 6]. In the present case, absence of disease prior to the commencement of orthodontic treatment suggests that the cyst occurred amidst the duration of the treatment.
The forces generated due to orthodontic movement of tooth most likely resulted in stimulation of the dormant cell rests lying in the jaws. It is also quite possible that the trauma during the surgical exposure of canine could also have triggered the event. The theory is further supported by the evidence that although the canine was brought to its functional position in the oral cavity, it displayed a distal rotation. If the cyst was present beforehand, the tooth movement would have been hampered and the canine would not have been able to erupt. The epicenter of cyst between the canine and lateral incisor suggests that the cyst has occurred towards the end or after the completion of orthodontic extrusion of canine and has caused displacement of the adjacent teeth.
In the present case, the cyst occurred as an extraneous variant between the roots of canine and lateral incisor. Although the cyst has originated between the two teeth, the major portion of the cyst lies above the premolars. Furthermore, the anteroposterior dimensions of the cyst are much larger compared to its buccolingual width. There was also absence of cortical plate perforation. This indicates that the cyst had expanded in an anteroposterior direction without causing much expansion of the cortical plates, which is characteristic of OKCs [2, 3].
Intermittent pain began only after eighteen months postcommencement of the orthodontic treatment. In odontogenic cysts, pain is usually associated with infection of the cystic wall or occurs due to impingement of large cysts on the nerves [7]. The secondary infection of cyst was confirmed by microscopic presence of areas of cystic wall showing intense inflammatory infiltrate with disrupted cystic lining.
The lining of OKC is relatively more fragile as compared to other odontogenic cysts, and is therefore, often removed in fragments [8]. Additional factor contributing to the fragility of lining is presence of glycosaminoglycan-rich zone in the capsule just beneath the epithelial lining, as demonstrated in the histopathological picture of our case. This zone is responsible for separation of areas of lining from the underlying capsule. Spread of the cyst between the trabeculae due to active proliferation of lining cells in the medullary spaces and secondary infection further make in toto removal of the cyst difficult [2]. As a result, remnants of the cyst may remain after its surgical excision, which account for the relatively higher recurrence rate of OKC [9].
However, in the present case, the cyst could be enucleated entirely, possibly because of thickening of cystic wall, which occurred over the long-standing course of the lesion. Even so, because of multiple factors contributing to the recurrence of OKC such as incomplete removal of cystic lining, high proliferative index, recurrence from offshoots from the basal layer of the surface epithelium, and indigenous potential for recurrence, long-term follow-up is crucial for management of such cases [9,10]. No evidence of disease was found in the periapical radiographs and OPG of the patient taken at six-monthly intervals for the present case, after a follow-up for 18 months.
Although accidental discovery of OKC during pre-orthodontic evaluation has been commonly reported, OKC arising as a result of complication of orthodontic treatment is quite rare. The present case comprised of an unusual mode of presentation of a sporadic, extraneous, infected OKC in the maxillary anterior region of a young female. The possibility of OKC occurring due to stimulation of cell rests of dental lamina during the orthodontic treatment needs consideration and reporting of similar cases would shed more insight into its etiological potential.
Sources of Support: None
Conflict of interest: The authors have no conflicts of interest to declare.
