Author(s): Atiqul Islam KM, Richmond Ronald Gomes*, FM Monjur Hasan, Shoriful Islam and Mamun Newaz
Background: Pituitary macro adenomas are benign in origin, mass effects of which, may lead to serious clinical symptoms such as visual impairments, chronic headache, and pituitary insufficiency. The visual disturbance in pituitary macro adenomas range from dimness of vision to bilateral total loss of vision. Visual field defect is one of the common presentations of pituitary macro adenomas. They usually results in bitemporal hemianopia by causing compression on optic chiasm. Our main objective of this study was to evaluate the changes of visual field in relation with cranio-caudal diameter of pituitary macro adenoma.
Methods and Materials: This cross-sectional, observational study was carried out at Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka from April, 2019 to September, 2020. Thirty six patients with pituitary macro adenomas underwent visual field analysis using Humphrey Field Analyzer30-2 program at Bangabandhu Sheikh Mujib Medical University. Correlation betweenmean deviation of visual field with craniocaudal diameter of pituitary macroadenomas, volume of tumor, duration of sypmtoms were observed.
Results: This study was conducted on 67 eyes of 36 patients including 22 male and 14 female subjects with mean age of 39.00 years and histologically proven pituitary adenoma. Mean cranio-caudal diameter was 31.72 mm. Highest number of patients had cranio-caudal diameter of 32-41 mm with mean deviation of -12.95 dB and -12.24dB in right and left eye respectively. Regarding correlation of mean deviation of visual field with cranio-caudal diameter of pituitary macro adenoma, Pearson correlation showed that r value was -0.358(p-value0.044) in right eye and -0.527(p-value 0.012) in left eye.
Conclusion: When pituitary macro adenomas grow in vertical direction it results in deterioration of visual field by compressing optic chiasma. The present study ascertains that there is significant correlation between the cranio-caudal diameter of pituitary macro adenoma and deviation visual field.
Pituitary adenomas account for approximately 12% of clinically symptomatic intracranial tumors. They are classified into two categories based on their size, micro adenoma (less than 1 cm) and macro adenoma (greater than 1 cm). Pituitary macro adenoma can cause visual field (VF) defects by compressing the optic chiasm or the optic nerve. Because of its anatomical relationship with the optic chiasm, pituitary adenoma typically results in bitemporal hemianopia [1].
Pituitary tumors are common lesions believed to account for 10% to 15% of all primary brain tumors. Data from academic medical centers suggest that pituitary tumors represent as many as 20% of surgically resected primary brain tumors [2].
The pituitary gland is crucial for the maintenance of several homeostatic functions, including metabolism, growth and reproduction. Most pituitary tumors develop in the adenohypophysis- the epithelial component that consists of the anterior and intermediate lobes of this gland, which is composed of six adenohypophysial cell types. These epithelial cells secrete peptide hormones that produce trophic hormones [3].
Pituitary adenomas are non-metastasizing neoplasms. They usually arise in the sellaturcica. In rare instances, they develop along the developmental pathway of the pituitary from the roof of the mouth to the base of the brain. These tumors show a wide range of hormonal and proliferative behavior. They might be small lesions with a slow rate of growth. When hormonally inactive, such tumors are typically detected as radiographic ‘incidentalomas’ or at postmortem examination. When they produce hormones in excess, they can give rise to severe clinical syndromes, such as acromegaly or Cushing’s disease, which affect many organ systems and can be lethal. Some pituitary adenomas grow rapidly and give rise to symptoms of an intracranial mass. These include headache, loss of normal anterior pituitary hormone production (by compressing the normal portion of the gland) and visual field disturbances (due to compression of the optic chiasm). They can also invade downwards into the paranasal sinuses, laterally into the cavernous sinuses (thereby disrupting coordinated eye movement) and upwards into the parenchyma of the brain [3].
Non-functioning pituitary macroadenomas (NFMAs) are the most prevalent pituitary macroadenomas. Although NFMAs are benign in origin, mass effects may lead to serious clinical symptoms such as visual impairments, chronic headache, and pituitary insufficiency. At the time of initial diagnosis, visual field defects are detected in 60-80% of NFMA patients [4].
The pituitary fossa is delineated in front by the tuberculumsella and chiasmatic sulcus. The dorsum sella and the posterior clinoid processes form the posterior relationship. The sellar floor, which separates the sellar contents from the underlying sphenoid sinus, extends from the tuberculumsella in front to the base of the dorsum sella posteriorly. The thickness of the sellar floor to be equal to or less than 1 mm in 82% of specimens and more than 1 mm thick in 18%. Occasionally, the floor was very thin, only a few microns thick [5]. The depth of the sella is the greatest distance between the floor and a perpendicular line connecting the tuberculum and dorsum sellae. The depth ranged from 5 to 12 mm, mean 9 mm. Sellar length, defined as the greatest anteroposterior diameter of the pituitary fossa, may occur at the level of the tuberculumsellae or below, depending on the shape.The length ranged from 7 to 14 mm, mean 10 mm. Sellawidth, defined as the width of the horizontal plateau of the sella floor. The range was 10 to 16 mm, the meanwas 14 mm [5].
The diaphragmasellae forms the roof of the pituitary fossa. It is a fold of dura mater, more often rectangular than circular and has a central opening, which transmits the infundibulum [5]. The position of the optic chiasma varies. It lies in the sulcus chiasmaticus in 5% and over the diaphragmasellae in 12%. These two positions are termed prefixed. The chiasma lies over the dorsum sellae, which is its normal position in 79%. In the postfixed position the chiasma lies over and behind the dorsum sellae and is found in 4%.The optic chiasm is situated 8-13 mm above the diaphragmasellae and therefore, there should be considerable growth of the tumor before vision is affected [6].
The normal chiasm overlies the diaphragmasellae and pituitary, the prefixed chiasm overlies the tuberculumsellae and the postfixed chiasm overlies the dorsum sellae. Of the sellaestudied, 10% were prefixed, 15% postfixed, and 75% normal [5]. Potential mechanisms of injury include direct disruption of conduction along the axon, impaired axoplasmic flow, demyelination and ischaemia from compression of chiasm vessels. Cited about observation, that the blood supply of the optic chiasm arises from a superior and inferior group of vessels, and the crossing fibres in the chiasm receive only the inferior group of vessels. Consequently, an infrachiasmal compression due to a pituitary tumor can produce a bitemporalhemianopsia [7-9].
Various patterns of visual field defects (VFD) have been described in patients with pituitary adenomas with the precise type of defect depending on the anatomy of the optic chiasm and its relation to the tumor. The typical VFD associated with pituitary tumors is bitemporal hemianopia, occurring when the body of the chiasm (which is comprised of the crossing nasal fibres of each optic nerve) is compressed by the enlarged gland. The defect may be complete, involving the whole hemi-field or partial, usually beginning superiorly and progressing inferiorly, depending on the degree of nerve compression. Anterior placed lesions can cause central scotomas and nerve fiber layer pattern VFD while posterior lesions may involve the optic tracts producing a homonymous hemianopia [10].
Incomplete bitemporal VF defects are much more common than true hemianopsia and are considered by neuro-ophthalmologists as a sign characteristic of chiasmal syndrome, which is usually caused by lesions that affect the optic chiasm from below. Pituitary adenomas are the most common of all chiasmal syndrome tumors. The visual deficits associated with pituitary adenoma depend on the size, location, and hormonal activity of the tumor as well as the position of the chiasm as it relates to the sellaturcica. According to a recent study, the tumor volume also affects the severity of the VF defect [11].
Pituitary tumors, by compressing the optic apparatus, may produce: (1) reduction or loss of visual acuity due to compression of fibers subserving central vision; (2) various types of field defects. The visual field defects that commonly occur due to pituitary tumors are: (1) Bitemporal hemianopia either incomplete or complete; (2) Temporal field defect in one eye with loss of vision in the other eye; (3) Central scotoma; (4) Junctional scotoma; (5) Homonymous hemianopia [10].
The pathway for afferent visual information begins in the retina. An important retinotopic organization is preserved throughout the course of the afferent visual pathways. The nasal retina receives information from the temporal field and the temporal retina information from the nasal field. The superior retina receives information from the inferior field and the inferior retina from the superior field. This upside-down and backward information is conveyed via the remainder of the afferent pathway [12].
Bilateral temporal VF defects, either pure or associated with additional defects, are the most common defects noted in patients with pituitary macro adenoma. Most patients had compression of the pre chiasmal optic nerves, the post chiasmal tracts, or both, in addition to compression of the chiasm, which may account for these impure VF findings that include areas outside the bitemporal zones. Such defects are typically present in patients with greater than 3 mm of displacement of the optic apparatus. In addition, patients with asymmetric compression of the optic pathway seen on MR images are likely to have asymmetric VF defects [11].
The cranio-caudal diameter of tumor superior to 30 mm was associated with a higher MD absolute value and a higher frequency of optic disc pallor. In patients with bigger tumor, the visual acuity was lower. It is supposed that the most frequent impaired visual function in patients with pituitary macro adenomas is visual field. A longer chiasmal compression and a bigger tumor involve a worse visual field defect [9].
MD is the mean of all deviations between the sensitivity threshold of each retinal point and the normal expected value found in healthy people. Therefore, MD indicates how much the visual field strays from the normal one. In patients with normal vision MD is approximately 0, whereas a negative number indicates a visual field defect [9].
This cross sectional, observational study was carried out in Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka, Bangladesh. From April, 2019 to September, 2020. Total thirty six consecutive admitted patients with visual field defect due to pituitary macro adenoma underwent visual field analysis using Humphrey Field Analyzer30-2 program. Changes in visual fields were analyzed separately for the right and left eyes in all patients. Correlation between cranio-caudal diameter of pituitary macro adenoma and mean deviation (in dB) of overall visual field changes were assessed by using Pearson correlation coefficient test. For statistical analysis, softwareStatistical package for social Sciences (SPSS) for Windows version 22.0was used. Statistical significance was set at p-value <0.05.
| Frequency (n) | Percentage (%) | |
|---|---|---|
| 19-30 | 11 | 30.6 |
| 31-42 | 15 | 41.7 |
| 43-54 | 8 | 22.2 |
| >55 | 2 | 5.6 |
Most patients were within 31 - 42 years age group (41.7%). Second large were within 19 - 30 years age group(30.6%) & third was within 43 -54 years age group (22.2%). Only 2 patients (5.6 %) were in the age group of >55.
Table 2: Distribution of study subjects according to gender (n=36)| Frequency(n) | Percentage (%) | |
|---|---|---|
| Male | 22 | 1.6 |
| Female | 14 | 38.9 |
About 61.6% patients were males and 38.9% patients were females. Male:female ratio is 1.57:1.
Table 3: Distribution of study subjects according to presenting complain (n=36)| Presenting complain | Frequency (n) | Percentage (%) |
|---|---|---|
| Headache | 32 | 88.9 |
| Dimness of vision | 24 | 66.7 |
| Vomiting | 8 | 22.2 |
| Abnormal body growth of body configuration | 12 | 33.3 |
| Increased thirst, urination or hunger | 4 | 11.1 |
| Infertility/amenorrhea/ galactorrhea | 8 | 22.2 |
| Unusual sensitivity to hot or cold | 2 | 5.6 |
Table 3 shows 33 (88.9%) patients presented with headache, 24(66.7%) patients presented with visual complains and 20 (55.5%) patients presented with hormonal abnormality.
Table 4: Distribution of patients according to fundal photograph (n=36)| Fundal photograph | Right eye n (%) | Left eye n (%) |
|---|---|---|
| Pallor | 15 (41.7) | 16 (44.4) |
| Atrophy | 4 (11.1) | 3 (8.3) |
| Normal | 17 (47.2) | 17 (47.2) |
Table 4 shows fundus was pallor in 15(41.7%) and 16(44.4%), atrophy in 4(11.1%) and 3(8.3%), normal in 17(47.2%) and 17(47.2%) in right and left eye respectively.
Table 5: X-ray skull finding (n=36)| X-ray findings | Frequency (n) | Percentage (%) |
|---|---|---|
| Anterior clinoid process (Eroded) | 3 | 8.3 |
| Posterior clinioid process (Eroded) | 5 | 13.9 |
| Seller size | ||
| AP (mm) | 14.94 ± 5.70 | 8.00 - 31.00 |
| Depth (mm) | 12.66 ± 5.64 | 6.00 - 33.00 |
Table 5 shows anterior clinoid process was eroded in 3(8.3%) and posterior clinoid process was eroded in 5 (13.9%) in X-ray skull. Mean AP diameter of sella was 14.94 ±5.70 mm (8.00-31.00) and depth was 12.66±5.64 mm (6.00-33.00).
Table 6: MRI finding (n=36)| MRI findings | Frequency (n) | Range |
|---|---|---|
| Volume of the tumor (cm3 ) | 16.01 ± 32.31 | 0.49 - 197.26 |
| Cranio-caudal diameter (mm) | 31.72 ± 10.31 | 12.16 - 54.37 |
| Antero-posterior diameter (mm) | 24.30 ± 12.53 | 7.51 - 79.85 |
| Depth (mm) | 25.57 ± 15.52 | 4.97 - 104.20 |
Table 6 shows different MRI findings of tumor. Volume of tumor was 16.01±32.31 cm3 (0.49-197.26), cranio-caudal diameter was 31.72±10.31 mm(12.16-54.37),antero-posterior diameter was 24.30±12.53mm(7.51-79.85) and depth was 25.57±15.52 mm (4.97-104.20).
Table 7: Visual field defect (n=36)| Visual field | Right eye n (%) | Left eye n (%) |
|---|---|---|
| Temporal field defect | 13 (36.1) | 12 (33.3) |
| Upper quadrant field defect | 4 (11.1) | 4 (11.1) |
| Three quadrant field defect | 2 (5.6) | 2 (5.6) |
| Atypical field defect | 0 (0.0) | 2 (5.6) |
Table 7 shows distribution of patients according to visual field defects. Temporal field defect was 13(36.1%) and 12(33.3%), upper quadrant field defect was 4 (11.1%) and 4 (11.1%),three quadrant field defect was 2(5.6%), 2(5.6%) in right and left eye respectively. Atypical field defect was in 2 (5.6%) in left eye.
Table 8: Pattern standard deviation of visual held in dB according to Cranio-caudal diameter (n=36)| Craniocaudal diameter (mm) | Right eye (n=32) | Left eye (n=35) | ||
|---|---|---|---|---|
| n (%) | Right eye(dB) | n (%) | Left eye(dB) | |
| 12 - 21 | 4(11.11) | 4.91 ± 3.84 | 4(11.11) | 4.54 ± 3.20 |
| 22 - 31 | 12(33.33) | 6.51 ± 4.38 | 11(30.55) | 4.94 ± 3.56 |
| 32 - 41 | 11(30.55) | 6.44 ± 4.03 | 13(36.11) | 8.89 ± 4.63 |
| 41 - 55 | 5(13.88) | 12.38 ± 2.95 | 7(19.44) | 12.47 ± 1.56 |
Table 8 shows pattern standard deviation of visual field in different cranio-caudal diameter. Maximum mean PSD was 12.38± 2.95 dB and 12.47± 1.56dB in right and left eye respectively in cranio-caudal diameter of 41-55 mm.
Table 9: Mean deviation of visual held in dB according to Cranio-caudal diameter (n=36)| Cranio-caudal diameter (mm) | Right eye (n=32) | Left eye (n=35) | ||
|---|---|---|---|---|
| n (%) | Right eye(dB) | n (%) | Left eye(dB) | |
| 12 - 21 | 4(11.11) | -7.20 ± 3.95 | 4(11.11) | -8.05 ± 5.66 |
| 22 - 31 | 12(33.33) | -9.42 ± 6.28 | 11(30.55) | -9.31 ± 6.95 |
| 32 - 41 | 11(30.55) | -12.95 ± 9.45 | 13(36.11) | -12.24 ± 5.30 |
| 41 - 55 | 5(13.88) | -16.43 ± 3.28 | 7(19.44) | -18.48 ± 2.57 |
Most patients were within cranio-caudal diameter of 32-41mm and mean deviation was -12.95±9.45 (dB)on right eye and -12.24±5.30 (dB) on left eye and numbers of eyes were 11 and 13 respectively. Second large were within cranio-caudal diameter of 22-31mm, 12(-9.42±6.28 dB) on right eye and 11(-9.31±6.95 dB) on left eye & third was within 41-55mm 5(-16.43±3.28 dB) on right eye and 7(-18.48±2.57dB) on left eye which also showed highest deviation
Table 10: Mean deviation of visual held in dB according to duration of symptoms (n=36)| Duration of symptom (months) | Right eye (n=32) | Left eye (n=35) | ||
|---|---|---|---|---|
| n | Right eye | n | Left eye | |
| <12 | 9(25.00) | -10.65 ± 4.62 | 11(30.55) | -12.52 ± 6.41 |
| 13 - 24 | 11(30.55) | -11.16 ± 9.31 | 12(33.33) | -12.59 ± 5.83 |
| >24 | 12(33.33) | -12.32 ± 7.57 | 12(33.33) | -11.18 ± 7.34 |
Table 10 shows mean deviation according to duration of symptoms. Maximum patient was in symptom duration>24 group and number were 12 on each eye with mean deviation of -12.32±7.57 dB, - 11.18 ± 7.34dB in right and left eye respectively. Next was in symptom duration 13-24 group and number was 11 on right eye, and 12 on left eye with mean deviation of -11.16 ± 9.31 dB, -12.59 ± 5.83 dB in right and left eye respectively
Table 11: Correlation of mean deviation of visual with craniocaudal diameter (n=36)| Right eye | Left eye | |||
|---|---|---|---|---|
| r value | p-value | r value | p-value | |
| Cranio-caudal diameter | -0.358 | 0.044 | -0.527 | 0.001 |
Pearson Correlation was performed to get r and p-value. The p-value is 0.044 in right eye, 0.001 in left eye.
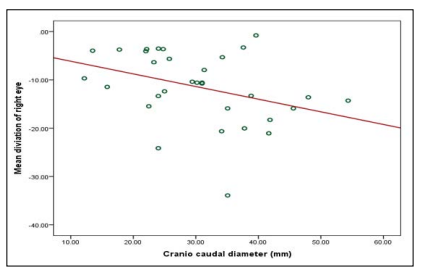
Figure 1: Correlation of mean deviation of visual of right eye with cranio-caudal diameter
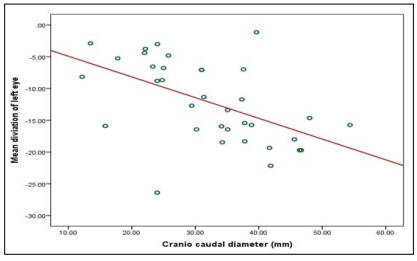
Figure 2: Correlation of mean deviation of visual of left eye with cranio-caudal diameter
Table 12: Correlation of mean deviation of visual with volume of the tumor, age and duration of the symptom (n=36)| Right eye | Left eye | |||
|---|---|---|---|---|
| r value | p-value | r value | p-value | |
| Volume of the tumor (cm3 ) | -0.129 | 0.483 | -0.261 | 0.131 |
| Duration of the symptom | -0.102 | 0.612 | 0.026 | 0.896 |
Pearson Correlation was performed to get r and p-value
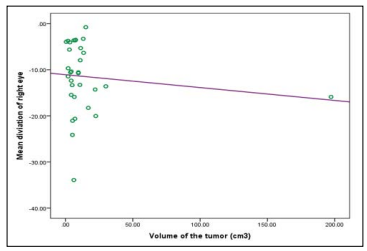
Figure 3: Correlation of mean deviation of visual of right eye with volume of tumor

Figure 4: : Correlation of mean deviation of visual of left eye with volume of tumor
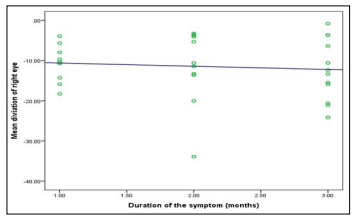
Figure 5: : Correlation of mean deviation of visual of right eye with duration of the symptoms
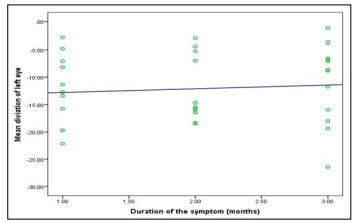
Figure 6:: Correlation of mean deviation of visual of left eye with duration of the symptom
Various patterns of visual field defects (VFD) have been described in patients with pituitary adenomas with the precise type of defect depending on the anatomy of the optic chiasm and its relation to the tumor. The typical VFD associated with pituitary tumor is bitemporal hemianopia, occurring when the body of the chiasm (which is comprised of the crossing nasal fibers of each optic nerve) is compressed by the enlarged gland. The defect may be complete, involving the whole hemi-field or partial, usually beginning superiorly and progressing inferiorly, depending on the degree of nerve compression. Anterior placed lesions can cause central scotomas and while posterior lesions may involve the optic tracts producing a homonymous hemianopia [10].
The relationship of pituitary tumor size and VF defects has been reviewed in several studies. The patients with VF abnormality had larger tumors and only the size of the adenoma was a significant factor for VF defects [13]. To quantify VF defects, we used the MD and PSD values of Humphrey perimeter. MD provides useful information concerning overall abnormality of a single field, as well as information regarding the worsening or improvement of fields over time. PSD shows the pattern of a localized abnormality. Both of the parameters are expressed numerically, so those are useful to quantify the VF defects more accurately. Using the Humphrey perimetry we measured VF defects quantitatively.
This study was conducted on 36 cases of pituitary macro adenoma in the Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh. In our study we found that, most of the patients were between 31 years to 42 years of age (41.7 %), with mean age of 39.00 ± 11.59 years. Pituitary adenomas occur in all age groups, with highest incidence between the third and sixth decades of life. As a general rule, functioning pituitary tumors tend to be more common among younger adults, whereas nonfunctioning adenomas become more prominent with increasing age. We found the mean age was 45.8 ± 15.6 years, ranging from 19 to 86 years of 39 patients [1]. We found the mean age was 52.2years±1.25 (range, 16-81), and the median was 54 years of 73 patients [7]. Age distributions of pituitary tumor were almost similar to above mentioned study.
Our study showed males outnumbered the females, male 22(61.6%) and female 14(38.9%) and is ratio is 1.6:1. Various studies showed different sex frequencies of pituitary macro adenomas patients [1]. Described the 39 patients, of whom, 24 were male and 15 were female. 28 patients were female (38.4%) and 45 were male (61.6%) of 73 patients [7]. Sex distribution of our study was similar to the study [1].
In our study, headache was the most common symptoms. Most of the patients complained of headache, 32 (88.9%) which had no specific variation and severity. Second most common symptoms were gradual loss of vision to blindness. Patients having no vision were excluded from this study. Visual field analysis was not possible in blind patients. We found 24 (66.7%) patients with dimness of vision. Our study showed 20 (55.5%) patients had hormonal abnormality and they were producing different symptoms. Growth hormone secreting macro adenoma was more common hormone secreting tumor 12(40%) and the rest 8 (22.22%) was prolactinoma [2]. Described that most common presentation was headache in 86.8% of patients. Five (13.9%) patients had visual symptoms.
In 36 patients, we have calculated 67 eyes instead of 72 eyes. Right eye of one patient had the visual acuity of FC at 1 foot and three patients had no PL/PR. One patient had visual acuity of HM from one foot on left eye. Because of severely compromised visual acuity, the bilateral visual field analysis could not be performed on the Humphrey Field Analyzer on these patients. Distribution of patients regarding fundal photograph pallor was found in 15(41.7%), 16(44.4%) atrophy in 4(11.1%), 3(8.3%) and normal in 17(47.2%), 17(47.2%) in right and left eye respectively. Our study is almost similar that of Barzaghi et al. (2012) where fundus was normal in 33/65(50.8%) and pallor/atrophy was in 32/65(49.2%).
Distribution of patients according to x-ray findings reveals that anterior clinoid process was eroded in 3(8.3%), posterior clinoid process eroded in 5(13.9%). 201 patients (366 eyes), all with preoperative visual field impairment, the preoperative mean MD was -17.50 ±0.82 dB (range -30.80 to -1.40). Among 139 eyes of 73 patients all with preoperative abnormal perimetry, the preoperative mean MD was -11.9±0.6dB (range, -31.9 to -1.6), and the median MD was -11 dB. We used computerized perimetry which have high sensitivity, reliability, standardization and reproducibility of results [7]. Computerized perimetry not only allows locating the defect but also quantify its severity based on comparison between the patient and a healthy population.
In our study mean volume of tumor is found to be 16.01±32.31 cm3. In our study Pearson correlation test between volume of tumor and mean deviation of visual field showed r value is -0.129 and p-value is 0.483 in right eye and r value is -.261 and p-value 0.131 in left eye which is not significant. In the study, the mean tumor volume was 14.36 ± 6.23cm3 (range 2.15-31.70cm3) [14].
Generally speaking, larger volume tumors will usually result in a higher risk of compression at the optic chiasm; however, this relationship is not found when tumor extension mainly occurs at the infrasellar or parasellar region instead of the suprasellar region.
In our study mean cranio-caudal diameter was 31.72mm±10.31 (range 12.16-54.37 mm) on magnetic resonance imaging (MRI). Antero-posterior diameter was 24.30±12.53mm (7.51-79.85) and horizontal diameter was 25.57±15.52mm (4.97-104.20). Study of Lee et al. also shown similar result where anteroposterior diameter was 21.8±8.8 mm and horizontal diameter was 23.6±9.7 mm. The mean cranio-cauda ldiameter was 31.0 mm±0.7 (range, 16-53), and the median was 30 mm [7]. The mean diameter of the tumor was 32.97mm ± 1.03 (13?60) of 100 patients.
Visual field analysis of our study shows temporal field defect was present in 13 (36.1%), 12(33.3 %) in right and left eye respectively. Upper quadrant field defect was present in 4 (11.1%), 4 (11.1%), three quadrant field defect in 2(5.6%), 2(5.6%) in right and left eye respectively. Atypical field defect was present 2(5.6%) in left eye [2]. Showed that at presentation, 12 (66.7%) patients had visual field changes while 6 (33.3%) did not. A range of visual field defects was noted; temporal defects were the most common abnormality. A range of visual field defects was noted; temporal defects were the most common abnormality. Our study shows maximum patients presented with temporal field defect. This is because pituitary tumors usually compress the chiasmatic crossing fibres leading first to bitemporal hemianopia.
In analysis of mean deviation according to cranio-caudal diameter, most patients having diameter 32-41 mm and mean deviation of visual was -12.95±9.45 dB,-12.24±5.30 dB in right and left eye respectively. Cranio-caudal diameter more than 41 mm was present in five patients and highest mean deviation was -18.48±2.57 dB. It was also found that there was deteriotion of mean deviation of visual field with increase of cranio-caudal diameter due to compression of optic chaisma. In fact, we found that if the adenoma grows in the vertical direction, it will usually result in more severe visual impairment. If the adenoma grows in the horizontal direction, it will usually cause less vision damage, but there is a greater chance of adenoma recurrence. This is because horizontal growth of the adenoma may invade the cavernous sinus which makes it difficult for the surgeon to completely remove the tumor. Therefore, only the vertical size of adenomas was investigated in this study
In symptom duration less than 12 months, 13-24 months and more than 24 months mean deviation was -10.65 ± 4.62dB, -12.52 ± 6.41 dB and-11.16 ± 9.31dB, -12.59 ± 5.83 dB and -12.32 ± 7.57 dB, -11.18 ± 7.34 dB in right and left eye respectively. Demonstrated that mean deviation was -10.45±0.6 dB wheresymptoms was <12months and mean deviation was -14.7±1.1 dB where symptoms was >12 months [7].
Pearson correlation duration of symptoms and mean deviation of visual field has shown that p-value is 0.612 and 0.896 in right and left eye respectively. So our study shows that there is no significant relation of mean deviation with duration of symptoms [15]. Study, showed similar result but study of Barzaghi et al. (2012) showed significant correlation. In correlation between cranio-caudal diameter and mean deviation in right eye, it was significant. We did Pearson’s correlation test r value was -0.358and p-value was 0.044 in right eye. It indicates if cranio-caudal diameter increases mean deviation decreases. Study of Barzaghi et al. (2012) also showed similar result.
In left eye r value was -0.527 and p-value was 0.001. Visual presentation of pituitary adenoma varies depending on the size of the tumor and its proximity to optic pathway. Our study demonstrates that if craniocaudal diameter increases it results in poor field of vision. Several studies confirm that poor preoperative visual field has lower probability of recovery compared to a patient displaying better preoperative mean deviation of visual field. So there is a need for increasing awareness among the colleagues of other disciplines, especially the ophthalmologists for timely referral of these patients for assisting prompt neurosurgical intervention. Progressive deterioration of visual fields is often the principle neurological criterion on which surgical management decisions are based.
When pituitary macro adenomas grows in vertical direction it results in deterioration of visual field by compressing the optic chiasm. Progressive deterioration of visual fields is often the principle neurological criterion on which surgical management decisions are based. The present study ascertains that there is significant correlation between the cranio-caudal diameter of pituitary macro adenoma and changes in visual field. This study will help to build awareness among the colleagues of other disciplines especially the ophthalmologist for early diagnosis of these patients and prompt neurosurgical intervention needed to save vision [16-29].
The limitations of the study were lack of Randomization of the sample so there may be sampling bias, study duration of study, small sample size and only preoperative deviation of visual field in association with cranio-caudal diameter was studied. Long term post-operative follow could strengthen our study.
Conflict of Interest: There were no conflicts of interests
Ethical Clearance: Appropriately taken
Funding: Self-funded
