Author(s): Jason Mammino*, DO and Jere Mammino, DO, FAAD, FAOCD
A 47-year-old male was seen in a rural Nicaraguan community for difficulty shaving his beard. The patient stated his face changed roughly 10 years
ago and since has never looked the same. He presented at the clinic with an eczematous rash confined to the sun exposed surfaces on his skin. His face and posterior neck were covered in a confluent lichenified erythematous eruption sparing only the forehead and eyelids. The upper chest, forearms, and dorsal hands were hyperpigmented with various hypertrophic and hyperkeratotic lesions. The diagnosis of chronic actinic dermatitis was made due to the overall clinical picture along with limitations in further diagnostic capabilities. After initial therapy, the patient ecstatically returned to the clinic with greatly improved skin
Chronic actinic dermatitis (CAD) is an uncommon dermatosis in which an eczematous, sometimes lichenified skin reaction occurs, following exposure to ultraviolet (UV) B, UVA, visible light, or in combination. Reactions are more severe in the summer months, possibly presenting from a delayed type hypersensitivity response to photo induced endogenous antigens [1]. A skin condition indicative of CAD was first detailed in 1933, but it was not until 1979 that Hawk and Magnus coined the now widely accepted term CAD [2]. Alternative names frequently used interchangeably are actinic reticuloid, a severe clinical variant, and chronic photosensitive dermatitis, a milder UVB and UVAsensitive variant [1].
Patients developing CAD are found globally with no preference for specific locations or races. Classically, this disease affects older men who become exposed during occupational or recreational activity, with an average age of onset in symptoms around 50 years old [1,3]. Recent studies have found that female patients with Fitzpatrick skin types V and VI, are being diagnosed at a younger age, roughly 40 years old, with an earlier onset of photosensitivity compared to lighter skin types [3]. Despite the difference in age of onset, Fitzpatrick skin types V to VI reacted equally severely to phototesting as compared to Fitzpatrick skin types I to IV [3].
The pathogenesis of CAD is partially understood and considered to be an idiopathic or a primary photosensitivity disorder. Photosensitive skin can react in either phototoxic or photoallergic reactions [4]. These types of cutaneous responses require the interaction of both chemical and physical substances, as reaction with drugs* or light individually will not illicit a response. Phototoxic reactions are ones in which 100% of the population should occur in, supposing appropriate wavelengths and sufficient dose of drugs [4]. These reactions result in damage to underlying DNA, producing an either unexpectant or desired response. Common substances that trigger phototoxic reactions are psoralens, chlorpromazine, coal tar, tetracycline, and sulfanilamide [4]. Photoallergic reactions are much less common and result from an immunologic response to cutaneous photosensitivity. Chemicals in the skin become absorbed and when irradiated, are converted to bind soluble or membrane-bound proteins which form the antigen [1,4,5]. Following the primary sensitization, a delayed type hypersensitivity skin reaction occurs on successive exposures. Due to their antibacterial properties, topical antimicrobials (example: 3,5,3’,4’-tetrachlorosalicylanilide) were a common cause of photoallergic reaction until their ban from integration within soaps, household, and cosmetic products [1,4,5]. Both theories result in cellular damage that would affect the sun exposed surfaces to skin.
Clinical manifestations are primarily found on the face, neck, forearms, upper chest, and dorsum of hands. Acute eczematous to chronic lichenified patches develop proportionally with the amount of UV light exposure. Skin surfaces such as eyelids, base of skin furrows, and the web space between fingers are spared due to limited sun contact [1,6]. Classic findings of sharp demarcations between unaffected and affected skin can assist in leading one to the diagnoses of CAD. Erythroderma and hyperpigmentation can present with long standing reactions, along with superficial excoriations from intensely pruritic skin [1,6].
With the overwhelming number of chemicals and medications employed in everyday life and for skin cosmesis, patch and photopatch testing are essential to rule out any underlying allergic component to eczematous skin [1,3,7]. Cutaneous biopsies are also recommended to analyze the CD4 to CD8 T lymphocyte ratio in the epidermis. Patients diagnosed with CAD have dermal infiltrates with an increased concentration of CD8 T lymphocytes, decreasing the ratio [7,8,9]. One major differential diagnosis to rule out is the eczematous variant of cutaneous T-cell lymphoma, which has an increase in the CD4 to CD8 ratio, compared to CAD [7,8,10]. Other dermatoses for differential diagnoses include allergic and aerogenic contact dermatitis, chronic atopic dermatitis, polymorphous light eruption, and phototoxic reaction to drugs [1,5,6,11].
The best method for treatment with CAD is complete photoprotection. Strict avoidance from all amounts of UV light will help prevent any future flares. For acute management, topical corticosteroids and oral prednisone along with daily emollients can be utilized [1]. If sun exposure is expected, one should apply a broad spectrum or inorganic sunscreen and wear long sleeves with a wide brim hat [12]. Physicians should keep in mind that sunscreen could be the underlying cause, for which patch testing should eliminate that possibility. Specialized UV light blocking window tinting for vehicles can be applied. For refractory disease, there are various case reports of using topical tacrolimus, azathioprine, and tofacitinib [13,14,15]. There are also reports of spontaneous regression in a low percentage starting after 10 years [1].
The patient is a 47-year-old Nicaraguan male with insignificant past medical history initially presenting with difficulty shaving his beard. When questioned about his skin, he explained that his skin started changing in his late 30’s. His skin was originally smooth but started to take on a sunburn and peeling look; eventually over many months to the current state today (Figure 1). He attempted to self-cure with various moisturizers and local remedies. Over many years of little to no response from therapy, the patient had struggled but accepted his new look.
Over his working life, the patient has held several outdoor occupations, with the most recent being a daytime outdoor security guard. He works most days of the week, with a baseball cap as his only method of sun protection. The patient states he sometimes goes shirtless during his shifts due to the extremely hot temperatures.
On examination of patient’s skin, his face, neck, upper chest, forearms, and backs of his hands had an eruption clearly different in color and texture compared to his non-sun exposed skin. The face, neck, and v-shaped area of his upper chest displayed a slight erythema, with a confluent eczematous and lichenified reaction with sharp demarcation between the normal appearing skin of the forehead, upper eyelids, and lower chest. The patient’s forearms and dorsal hands displayed a less exaggerated reaction, with fewer lesions and a less defined textural change between the upper arms and forearms. Excoriated lesions were noted in the arms and neck.
In a rural setting, such as Nicaragua, the diagnosis was suggested based on the clinical picture of eczematous reaction clearly defined by sun exposed skin and lack of possible further testing. For this patient, the need for ultraviolet light avoidance was explained in detail. Asking for the nighttime shift at work and wearing long sleeves while outside, were a couple of easy ways to greatly reduce exposure. Application of a broad-spectrum or physical blocking sunscreen was stressed if the patient was to spend any amount of time in the sun. To calm down the inflamed skin, we prescribed a topical corticosteroid with an oral prednisone tapering dose, in addition to a daily antihistamine for mild pruritus.
After 16 days the patient returned to the clinic with a huge smile, immensely grateful for his care (Figure 2). He first made it known that shaving his face had become much easier. He had switched his security position to a nighttime shift and has been abiding by our recommendations for his sun avoidance, skincare, and maintenance. The patient stated, he could not remember the last time his face was this clear and almost did not recognize the man in the mirror.
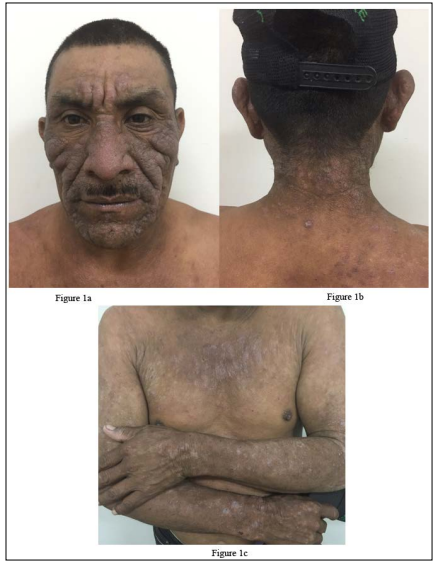
Figure 1: Chronic Actinic Dermatitis: A Patient’s face displaying chronic hyperpigmented and lichenified reaction from successive bouts of exposure to ultraviolet light. Note the sparing of the forehead and upper eyelids. B Posterior neck and post auricular skin is shown to be hyperpigmented with an eczematous reaction. Note the clear demarcation from involved to uninvolved skin and the excoriated lesion. C Lichenification to the upper chest and hyperpigmentation with eczematous lesions on the forearms.

Figure 2: 16 days after therapy started, the patient’s face and upper chest are shown with an overall improvement in lichenified skin with normalization of cutaneous color and texture.
reating hypertension or diabetes at underserved clinics is relatively manageable. Nevertheless, when an uncommon illness, like CAD, surfaces not every clinic is equipped to confidently manage patient care. Basic medications to control routine profiles are readily available at most rural clinics, due to gracious donations. Drugs, like oral prednisone, are available in major city drug stores, but with the financial struggles and logistical hurdles, most patients that fall into this population do not utilize optimal therapy for their disease. Besides medication, laboratory testing is another obstacle patients and clinicians face. The clinic in Nejapa where this patient was seen is fortunate to be outfitted with a laboratory, where technicians can run simple hemograms, CMPs, and cholesterol levels. Unfortunately, more complex exams such as patch and photopatch testing, punch biopsies, and lymphocytic analysis would only be available in major cities. Due to these limitations, physicians must rely heavily on their history and physical exam for the correct diagnoses.
Further complicating this scenario for our patient is the location in which he lives. Nicaragua is a troublesome setting for anyone with a photosensitive dermatosis. The amount of UV energy increases as you approach the equator. This is mainly due to the decrease of the zenith angle, thus allowing for less absorption by atmospheric particles and more radiation to pass onto Earth’s surface [16]. Nicaragua and other peri-equatorial countries have high ultraviolet indices, thus producing an even more severe response to photosensitive skin.
Despite having a visually distressing condition, treating our patient proved acutely successful. Switching his shift at work, to avoid the sun altogether, was the single best way to change his outlook moving forward. Continuity of care for this patient will be challenging since he lives a few hours via city transportation each way. Therefore, educating him on how and why his skin transformed the way it has, and thoroughly explaining prophylactic measures will be invaluable to continuing to improve and maintain his skin.
Future research to elucidate a more complete understanding of the pathogenesis will guide physicians in the management of CAD and refractory cases. The main limitation is the small patient population presenting with CAD symptoms.
To better help patients such as the one presented above, reaching out and donating time to rural clinics and underserved patient populations of the world, has profound effects on the communities you serve. There are numerous organizations you can contact, who are looking for physician help.
We report a case of chronic actinic dermatitis, seen in a rural community in Nicaragua. Despite living in a hometown with a high ultraviolet index and little access to healthcare, simple measures of photoprotection and education, along with topical and symptomatic medications, can be utilized to greatly improve the lives of patients battling chronic actinic dermatitis. *The term drug is an umbrella term designated to include any environmental substances, household items, food preservatives, and agricultural and industrial chemicals.
