Author(s): Roxanne Jillan V Mauleon*, Ma Flordeliz Abad Casintahan and Melanie Joy Doria Ruiz
ABSTRACT
Background: Xanthomas are cutaneous lesions, ranging from papules to nodules and plaques, consisting of infiltrates of lipid-containing histiocytic foam cells. These usually result from disturbances in lipoprotein metabolism leading to the accumulation and/or deposition of lipoproteins in plasma or tissue. This case report aims to present a patient with coexisting tubero-eruptive and planar xanthomas, associated with underlying hyperlipidemia.
Case Report: A 49-year-old Filipino female presented with multiple, well-defined, yellowish papules, nodules and plaques on the elbows, hands, knees, feet, antecubital and popliteal fossae, which started 8 years prior. Initially diagnosed as a case of benign fibrous histiocytoma, she was lost to follow-up until new lesions emerged. Blood tests done revealed hyperlipidemia. Histopathological examinations were consistent with xanthoma. She was referred to Internal Medicine and was prescribed Atorvastatin 40 mg ODHS and Fenofibrate 200 mg OD. She also underwent a series of surgical excisions for some of the large nodules that caused discomfort and mobility problems.
Conclusion: This case highlights the importance of the groundwork that history-taking and physical examination establish. Accurate diagnosis of xanthoma is crucial because it may uncover underlying atherosclerotic cardiovascular disease, which, when managed promptly, can delay its progression. Given the potential familial or hereditary nature of hyperlipidemia, it is essential to stress the importance of testing not only the patient, but also family members, even those without cutaneous manifestations. Despite the limited use of complex assays and genetic testing in the Philippines, returning to basics such as simple lipid profile tests can reveal serious health implications.
Xanthomas are lesions that consist of infiltrates of lipid-containing histiocytic foam cells that usually result from a disturbance of lipoprotein metabolism leading to accumulation and/or deposition of lipoproteins in plasma or tissue. They can be classified according to their cutaneous manifestation and anatomical location which are namely, eruptive, tuboeruptive, tuberous, tendinous or planar, and can presentanywhere from the extensor surfaces of hands, arms, knees, elbows to the buttocks and intertriginous areas. Data regarding the prevalence of the various types of xanthoma are lacking, however, vast majority of cases are xanthelasma palpebrarum. The presence of these lesions should warrant an investigation of lipid levels because xanthomas are not just a disease entity in itself, but rather a marker of an underlying disease, that could eventually lead to serious cardiovascular disease if left untreated [1-3].
A 49-year-old female, Filipino, born to non-consanguineous parents, presented into our institution with multiple, well-defined, firm, yellowish papules, nodules and plaques on both elbows, knees, thighs, feet, hands and both antecubital and popliteal fossae. Lesions started 8 years prior, initially manifesting as a solitary, yellowish nodule on the left ankle with no associated symptoms such as pruritus, pain or discomfort. Patient sought consult with a physician at a private hospital where blood chemistry was done which, according to the patient, reportedly revealed hypercholesterolemia. She was prescribed an unrecalled medication which she only took for 1 month with no subsequent follow-ups. On interim, there was noted appearance of similar lesions on both elbows which prompted consult at another private hospital 3 years prior to consult, where biopsy done on the solitary, yellow to brownish nodule on the ankle of the left foot, revealed Benign Fibrous Histiocytoma. Patient was then advised to seek consult with a dermatologist; however, she was again lost to follow-up. Thereafter, yellowish papules and plaques started appearing as well on the hands, elbows and feet with gradual increase in size, and with some lesions, particularly the nodules on both elbows and feet, which were associated with pain upon manipulation. Past medical history showed that the patient is hypertensive, maintained on Losartan 50mg once daily. She is a non-smoker and non-alcoholic beverage drinker, and her diet mainly consists of fried food, pork, rice and bread. Family history revealed that her mother and most of her siblings were also hypertensive, and one of her elder brothers also presented with similar lesions, but unfortunately passed away due to a cerebrovascular accident. History of dyslipidemia in the family is unknown. There was reportedly, a family history of diabetes mellitus with two of her brothers, and psoriasis with her father and fifth elder brother as well.
On cutaneous examination, the patient presented with multiple, well-defined, firm but mobile, irregularly-shaped, non-tender, yellowish papules and erythematous nodules with yellow dots ranging in size from the smallest measuring 1 x 1 cm, to the largest measuring 2 x 3 cm on the dorsal aspect of both hands including the metacarpal, proximal and distal interphalangeal joints, as well as multiple, well-defined, firm, yellowish, papules and multiple, well-demarcated, yellowish plaques on the dorsal and palmar aspects of the hands and fingers, specifically overlying the creases (Figure 1). There were also noted multiple, well-defined, firm, yellowish to hyperpigmented papules and grouped nodules on both elbows, each ranging in size from the smallest being 1 x 1.5 cm to the largest measuring 3 x 3.5 cm, as well as multiple, yellowish linear plaques on both antecubital fossae (Figure 2). On the lower extremities, there are multiple, well-defined, yellowish to hyperpigmented plaques and nodules on the left knee, and few, yellowish linear-plaques on both popliteal fossae (Figure 3), as well as multiple, well-defined, yellowish to hyperpigmented nodules on both feet, measuring from 2 x 1.5 cm to 3 x 3.5 cm (Figure 4). The rest of the physical examination was unremarkable.

Figure 1: Hands. A. Multiple, Well-Defined, Firm, Irregularly- Shaped, Non-Tender Yellowish Papules and Erythematous Nodules with Yellow Dots on The Dorsal Aspect of Both Hands. Multiple, Well-Defined, Firm, Yellowish Papules and Multiple, Well-Demarcated, Irregularly-Shaped, Yellowish Plaques on The Palms and Fingers of Both Hands.
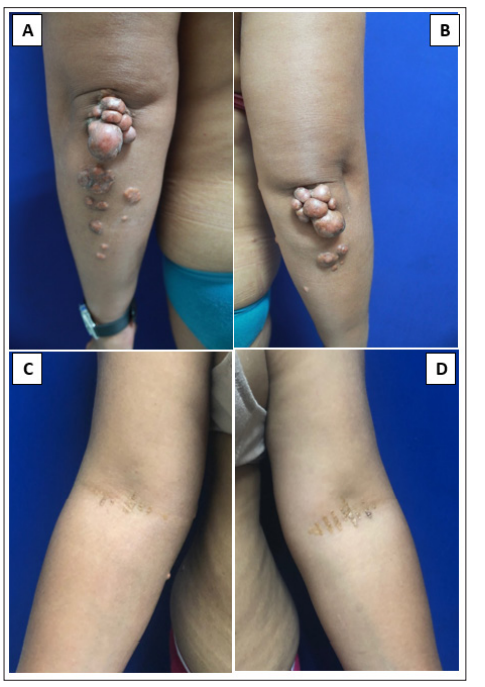
Figure 2: Elbows and Antecubital Fossae. A, B. Multiple, Well- Defined, Firm, Yellowish to Hyperpigmented Papules and Grouped Nodules on Both Elbows. C, D. Multiple, Ill-Defined, Yellowish Papules Coalescing into Linear Plaques on Both Antecubital Fossae.
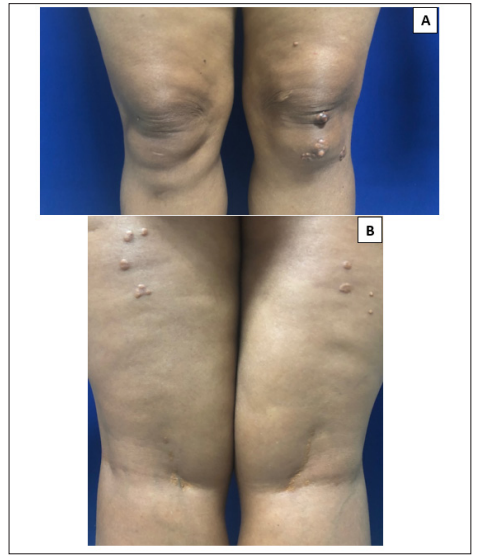
Figure 3: Knees and Popliteal Fossae. A. Multiple, Well-Defined, Firm, Yellowish to Hyperpigmented Plaques and Nodules on the Left Knee. B. Multiple, Well-Defined, Yellowish Papules on The Posterior Thighs and Multiple, Coalescing into Linear Plaques on Both popliteal Fossae.

Figure 4: Feet. A, B, C, D. Multiple, Well-Defined, Pedunculated, Yellowish to Hyperpigmented Nodules on Both Feet
An excision biopsy was done on a yellowish nodule on the right posterior forearm and histopathological examination revealed a flat epidermis with a compact stratum corneum, dermal fibrosis, and sheets of foam cells extending into the deep dermis (Figure 5).
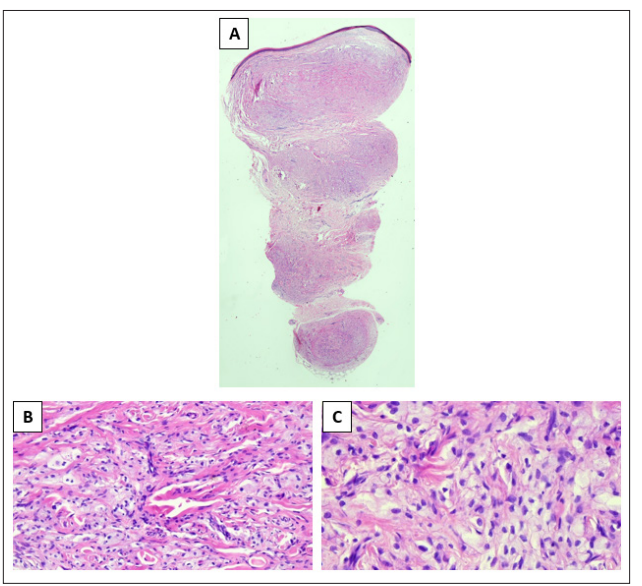
Figure 5: Histopathologic Findings (H&E Stain). A. Epidermis is Noted to be Flat. B, C. Dermis Contains a Dense Population of Foamy Histiocytes.
Dermoscopy of the nodule on the 3rd digit of the right hand, the plaque on the right posterior forearm, and the nodule on the 3rd digit of the right foot, all revealed bright yellow globules on a background of erythema and telangiectasia with white streaks representing areas of fibrosis [4]. (Figure 6)
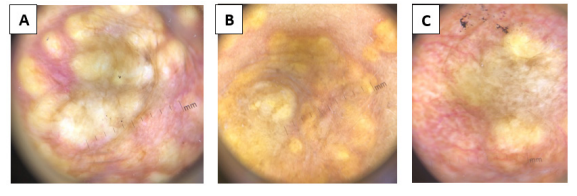
Figure 6: Dermoscopy A. Nodule on the 3rd Digit of the Right Hand. B. Plaque on the Right Posterior Forearm. C. Nodule on the 5th Digit of the Right Foot. All show bright yellow globules on a background of erythema and telangiectasia with white streaks
On the basis of history, clinical examination, dermoscopic, and histopathologic findings, a diagnosis of tubero-eruptive and planar xanthoma was made. On further investigation, blood tests showed hyperlipidemia (cholesterol of 638 mg/dL, triglycerides of 315 mg/dL, and LDL of 239 mg/dL) but with normal HDL of 102 mg/dL. CBC, blood glucose tests, and renal, liver, and thyroid function tests were all within normal limits. Testing of the patient’s family members was advised to probe into a familial cause of the patient’s dyslipidemia; however, it was unsuccessful as both of her parents were already deceased, and her siblings declined to participate in further investigation.
The patient was then referred to Internal Medicine for medical management, where she was started on Atorvastatin 40 mg ODHS and Fenofibrate 200 mg OD. Slight improvement of her lesions, particularly the tubero-eruptive xanthomas on her palms, was noted with continuous intake of the prescribed medications. She was also referred to Orthopedics to rule out any possible bony involvement if surgical excision was to be done; X-rays of both hands, elbows, and feet were requested, which revealed no osseous pathology. Subsequently, she underwent a series of successful surgical excisions of the large nodules that caused discomfort and mobility problems but was lost to follow-up afterward.
Xanthomas are cutaneous lesions, ranging from papules to nodules and plaques, containing lipid-laden foam cells occurring most frequently in patients with disorders of lipid storage and lipid metabolism. They develop because of leakage of lipid from the vasculature into the surrounding tissues, where macrophages subsequently phagocytize them. Because cholesterol is not degraded, it accumulates within these cells, creating foamy macrophages [5].
The diagnosis of xanthomas is usually apparent, especially when the classic red-yellow lesions are evident at presentation. However, in some cases, particularly when lesions have just started to appear, misdiagnosis may occur. This was the case in our patient, who was initially diagnosed with benign fibrous histiocytoma. Clearly, the two conditions are managed differently and have contrasting prognoses. Xanthomas, as mentioned previously, are not just a disease entity in itself but a marker of an underlying disease, notably atherosclerotic cardiovascular disease. Immediate testing and treatment upon diagnosis are warranted to prevent worse outcomes. Unfortunately, for our patient, what was initially thought to be a benign condition turned out to be much more serious, with subsequent growth of papules, nodules, and plaques, all over her extremities, causing pain and mobility problems in some areas.
Xanthomas vary in clinical presentation and are classified as eruptive, tuberous, tubero-eruptive, tendinous, or planar. Eruptive xanthomas typically appear suddenly as multiple, erythematous- yellow, dome-shaped papules on the extensor surfaces of the extremities, buttocks and hands. Early lesions may have an erythematous halo and are associated with pruritus and tenderness. They occur almost exclusively in the setting of elevated plasma levels of chylomicrons, with the most common causes of chylomicronemia being secondary forms of hyperlipoproteinemia namely, uncontrolled diabetes mellitus, alcohol ingestion, or exogenous estrogens. Tubero-eruptive and tuberous xanthomas usually appear on the elbows, knees, and buttocks. They are thought to be at two ends of a spectrum, with the former appearing as dermal papules that may have an inflammatory component, and the latter encompassing the larger, non-inflammatory, nodular lesions that may extend beyond the subcutaneous tissue [2,6,7].
Tendinous xanthomas can diffusely infiltrate tendons, tendon attachments, ligaments fascia and periosteum. They form free movable, hard nodules or spindles covered by normal skin. Sites of predilection are the Achilles’ tendons, tendons on the backs of the hands and fingers, as well as elbows, knees and heels. Planar xanthomas are yellow-orange plaques that usually involve the peri-orbital areas, neck, upper trunk and flexural folds. They can also be associated with secondary hyperlipidemia, especially in cholestasis, as well as monoclonal gammopathy [3,8,9].
Etiologies of xanthomas may be categorized into primary dyslipidemias which may have a familial component, secondary dyslipidemias, which are usually acquired, or normolipemic states. For the primary dyslipidemias, the World Health Organization (WHO) formally adopted the Fredrickson classification that distinguished five major types of hyperlipoproteinemia. Each type represents a characteristic defect and pattern of lipoprotein accumulation. These are Type I for familial lipoprotein lipase (LPL) deficiency or familiar hyperchylomicronemia, Type IIa for familial hypercholesterolemia, Type IIb for familal combined dyslipidemia, Type III for dysbetalipoproteinemia, Type IV and V for familial hypertriglyceridemia, with Type IV defined by an increase in LDL, and Type V defined by an increase in VLDL and chylomicrons. In addition to the abnormality and lipoprotein excess described, each phenotype has also been associated with a specific xanthoma type. Combined planar, tuberous, and tubero- eruptive xanthomas, accompanied by hypercholesterolemia and hypertriglyceridemia, as seen in our patient, are suggestive of Type III hyperlipoproteinemia or dysbetalipoproteinemia. It is also worth noting that planar xanthoma presenting on the palms, or xanthoma striatum palmare, is almost always pathognomonic for dysbetalipoproteinemia [10-13].
Confirmation of this diagnosis would entail complex assays such as ultracentrifugation and electrophoresis, as well as genetic testing to identify the affected gene involved. However, these are costly and not widely available in many countries, including the Philippines. Hence, in our clinical practice and setting, the importance of taking a detailed personal and family history, clinical signs, and basic laboratory tests such as a lipid profile is highlighted. This would have been our initial approach to determine if there was a familial nature to our patient’s dyslipidemia; however, even after much prodding, the family members declined to undergo testing.
Histopathologically, xanthomas are characterized by fibrosis in the superficial dermis, and the presence of large sheets and clusters of lipidized macrophages, the so-called foam cells, diffusely scattered throughout the dermis. In some areas, the foam cells lie in thin streaks between collagen bundles and occasionally, a perivascular arrangement is seen. All these findings were noted in our case [8,14].
Management for xanthomas is pretty clear-cut; the goal is to reduce plasma cholesterol levels, which would lead to a subsequent reduction of lesions and incidence of cardiovascular disease. The initial step is a lifestyle change and diet modification. Combined drug therapy, such as HMG-CoA reductase inhibitors, ezetimibe and fibrates, has been reported to have a positive effect on the patient’s lipid profile and on xanthoma regression. For larger lesions that do not regress with medical management alone, especially those that cause pain and mobility problems, surgical excision is advised. Other modalities such as lipoprotein apheresis, are also recommended for those who suffer from familial lipoprotein disorders such as familial hypercholesterolemia, while laser therapy has also been utilized for planar xanthomas [10,15-18].
As dermatologists, we are usually the first in line to see patients with xanthomas. Therefore, this case highlights the importance of the groundwork that history-taking and physical examination establish. Accurate diagnosis of xanthoma is crucial because it may uncover underlying atherosclerotic cardiovascular disease, which, when managed promptly, can delay its progression. Co-management with Internal Medicine, Cardiology, and Surgery/Dermatologic Surgery is recommended to treat patients comprehensively. Additionally, given the potential familial or hereditary nature of hyperlipidemia, it is essential to stress the importance of testing not only the patient, but also family members, even those without cutaneous manifestations. Despite the limited use of complex assays and genetic testing in the Philippines, returning to basics such as simple lipid profile tests can reveal serious health implications.
The authors have no conflicts of interest to disclose
The authors have not received funding for this manuscript
