Author(s): Maneeth Mylavarapu, Patel Neel Kalpeshbhai, Vu Thi Thu Hien, Parakh Patel, Puneet Kahlon, Amna Minhas, Zain Ul Abdin and Marjan Assefi*
The consequences of End Stage Liver Disease i.e., Liver Cirrhosis has been a growing cause of morbidity and mortality in the developed countries, making it 14th most common cause of death worldwide and 4th in the Europe [1]. Patients often delay seeking medical care, since they are asymptomatic in the early stages of Liver cirrhosis and are admitted later due to the complications associated with it. It is a condition whose prognostic value plays a significant role in predicting the mortality rate and treatment options of the affected individuals [2].
In the past, multiple criteria’s and scoring systems like Child-Pugh score, MELD, etc. have been used to identify high-risk patients. One of the widely used prognostic markers i.e., Child-Pugh
score, was framed in 1964 by Child and Turcotte to categorize patients who would benefit from shunt surgery to relieve portal hypertension, but later became the primary tool to assess the prognosis in liver cirrhosis [3]. The scoring system was further modified by Pugh et al in 1973 to increase its prognostic value and multiple adjustments have been made to the criteria to determine the same [2]. It has been classified as A, B and C attributing to the liver function as good, moderately impaired, and advancely impaired respectively [4]. Another scoring system named Model for end-stage liver disease (MELD) was conceptualized in 2001 to determine the survival rate in patients post trans jugular intrahepatic portosystemic shunts (TIPS). Later it has shown to predict survival in patients with complications in Liver Cirrhosis [5]. The scoring system has been modified to generate more accurate results in predicting the prognosis of patients in liver cirrhosis, but along with the advantages of the modified version, MELD came with some disparities that needs further improvement [6]. In modern practice we can also use them to determine whether patient has acceptable chances of survival if given treatment (like resection of liver, arterial embolization) or whether resources we spend on the therapy is justified (such as transplant). Child Pugh score and MELD are like two peas in a pod yet very distinct. Both have done fairly similar in most of the studies, yet each has its own advantages and disadvantages. The aim of this article was to compare the differences of Child-Pugh score and the MELD score. And, to further elaborate different variables that affect the prognostic value of them.
Ascites, hepatic encephalopathy (HE), nutritional status, total bilirubin, and albumin were all included in the original Child- Pugh score. Nutritional status was removed from the Child-Pugh classification and prothrombin time or international normalized ratio (INR) was added. In clinical practice, the Child-Pugh score has been utilized extensively to evaluate the degree of liver dysfunction.
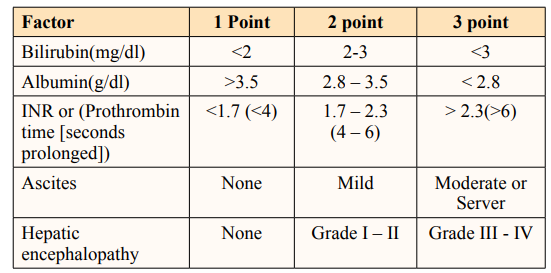
Figure: Different Factors and points [7].
The Child-Pugh score is useful for predicting not just the risk of dying from any cause but also the chance of dying from variceal hemorrhage and other complications resulting from liver disease. The Child-Turcotte A, B, and C classifications were developed in 1964 to help determine which patients would be suitable candidates for elective surgery to relieve portal hypertension [7]. Categories A and B refer to patients with normal liver function, while C describes those with severe liver damage [8]. Five clinical and laboratory criteria were utilized in the original grading system.
Anyone who works with patients who have severe liver disease or who are on dialysis should be fluent in the Child-Pugh grading system. The score and its interpretation can be used to guide care, reducing the risk of harm due to improper monitoring or delayed actions and boosting positive patient outcomes [9]. Numerous research have compared their discriminative capacities up to this point. Even so, the findings were still debated. Studies were split on whether or not the Child-Pugh score should be used [10]. This systematic review aimed to examine studies that used the Child- Pugh score to evaluate prognosis in cirrhotic patients and find out the relevance of the value to both patients and medical officers.
How significant is the Child-Pugh score to evaluate prognosis in cirrhotic patients to doctors and patients?
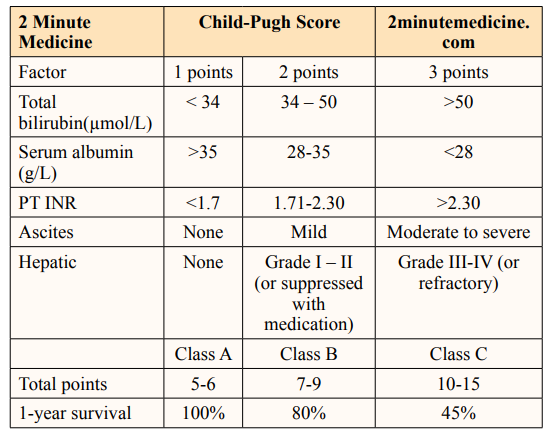
The prognosis of patients with liver cirrhosis has been mainly measured using the child PUGH (CP) score and model of end- stage liver disease (MELD). The variables associated with each of these scoring systems affect their prognostic value and neither of the criteria has been proven to be superior (Durand & Valla, 2004). A general overview of the comparison between both studies is shown in the table below.
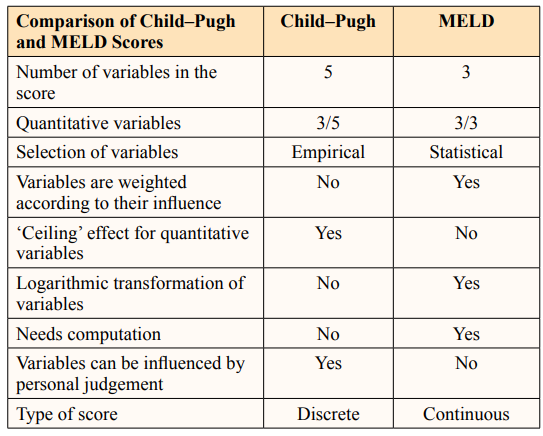
Table depicted to compare the parameters between Child-Pugh and MELD scores. Durand, F., & Valla, D. (2005).
However, to understand the similarities and differences between the Child Pugh score and the MELD score, various papers with different types of studies were analyzed to obtain the information of the predictability, and prognostic values of the Child Pugh score and the MELD scores under various circumstances. A total of 66 research papers were assessed and 14 papers were selected which contained a comparison study on the Child Pugh score and the MELD score.
Salerno et al., conducted an experimental study 140 cirrhotic patients undergoing trans jugular intrahepatic portosystemic shunt (TIPS) to determine the prognostic value of Child PUGH score and MELD for a better understanding of further treatment options. During the study time with a median follow-up of 23.7 months, it was found out that the 3-month prognostic value of the MELD score was found to be superior to the Child Pugh score (0.84 vs. 0.70, P= 0.038) [11].
In a prospective observational study by Dr. Jerome and his colleagues to compare the accuracies of MELD and Child Pugh scores in predicting 6-month mortality in cirrhotic patients, it was observed that Child Pugh score, MELD and MELD Na scores predictions were very close. Out of the 308 cirrhotic patients initially observed, 154 patients had decompensated cirrhosis. In a 6 month-up period, 42 people died. The area under the R.O (receiver operating) curve for prediction of 6-month mortality of Child Pugh was 0.882, MELD was 0.866, and MELD Na was 0.887 for the whole study group. For patients with decompensated cirrhosis who died in the 6- month period, the scores were 0.796 for Child Pugh, 0.800 for MELD, and 0.833 for MELD Na [12].
In the cohort, study was conducted among a group of 102 patients with decompensated cirrhosis for a 6-month follow-up period to pick the best score among MELD, Child Pugh, and Creatinine modified Child Pugh scores in predictability of survival. In the area under the R.O curve, no significant differences were seen among the three scores, but all the three had average accuracy in predicting the survival (areas: 0.71 to 0.79). In Cox regression analysis, MELD (c- statistics: 0.73) and Creatinine modified Child Pugh score (c-statistics: 0.69) had better predictability when compared to Child Pugh score (c-statistics: 0.63). Marked increase in the predictability was seen in all the three scores (c-statistics: 0.77 to 0.81) when adjustments for gamma-glutamate trans peptidase levels were made [13].
Giannini et al., conducted a similar cohort study in which they wanted to analyze that whether inclusion of serum creatinine parameter into Child Pugh score can increase in accuracy of predicting the mortality and then compared it versus the MELD score. However, they only focused on short-term prognosis. In a cohort of 145 cirrhotic patients, they calculated Child Pugh score, Serum creatinine modified Child Pugh score, and MELD and compared them. They found that inclusion of serum creatinine as a parameter increased the accuracy of the traditional Child Pugh score (P= 0.012). But the MELD still came out to the best in accuracy of predicting mortality in short term prognosis when compared to creatinine modified Child Pugh score (P= 0.047) (Giannini et al., 2004).
Angermayr et al., conducted an observational study to compare the predictive power of Child Pugh score and MELD and to access the predictive value of determinants used in the two scores. A total of 475 patients fulfilled their inclusion criteria out of the 501 patients who underwent elective TIPS placement. They followed the patients for long time, with median follow-up of 5.2 years and median survival of 4.6 years. During the follow-up time, 230 people died, out of which 75 died in first 3 months. In stepwise proportional hazards analysis, they found that both were equally predictive for 1 month, 3 months, and 1-year survival according to c-statistics. But stepwise Cox model showed that MELD was a better predictor of survival [14].
An observational study conducted by Rahimi-Dehkord et al., to predict the best score to use the mortality and need for removal from the waiting list for liver transplantation due to poor medical conditions. They have observed a total of 257 patients over a period of 9 months. MELD and Child Pugh was calculated at the time of the listing. They used ROC- curve and Area under the curve to calculate the predicting ability of both the tests. During the follow-up period, 22 patients died and 9 were removed from the waiting list due to poor medical conditions. They observed that the AUC for Child Pugh score (0.75) was bigger than MELD (0.69). They have found that sensitivity of both Child Pugh score and MELD were same (0.74) but Child Pugh score (0.74) had higher specificity over MELD (0.58) [15].
In a study by Lee et al, the c statistic of MELD (0.73-0.84) was insignificantly slightly superior to that of Child-Turcotte-Pugh score (0.67-0.809), making it unnecessary for the well-established child Pugh score for the use of prognosis of HCC in cirrhotic patients. However, MELD score was perceived to be superior for the allocation of transplant receiving patients.
In a prospective descriptive study on comparison of the prognostic value of mortality of Child Pugh score and MELD score conducted by Valenzuela Granados et al., at Hospital Nacional Cayetano Heredia, Lima-Peru, they found that Child Pugh score and MELD score did not have a significant difference (Valenzuela Granados et al., 2015).
One thousand six hundred and eleven patients with chronic liver disease were studied by Said et al., in order to determine the predictability of MELD in alcoholic hepatitis. They observed the survival predictability curves to evaluate the predictive ability of the MELD score for survival. They also used Receiver operating characteristic (ROC) curves compare the MELD score to the traditional Child Pugh score. The MELD score for 1-year mortality in chronic liver disease (c-statistics for all subgroups ≥0.75) and for 3- and 6-month, mortality in alcoholic hepatitis (c-statistic ≥0.83) were like traditional Child Pugh score. However, they found that Hepatic encephalopathy was an independent predictor of death (Hazard ratio—2.8, P<0.0001) [16].
A prospective observational study was conducted by Chaurasia et al., to find the best prognostic factor to determine the survival in hospitalised decompensated cirrhosis patients. 216 patients were observed over the course of their hospitalization. Their MELD and CTP scores were calculated at admission and throughout until discharge or death. The study reported MELD and CTP scores to be higher in expired cases (31.91 ± 4.92, 12.44 ± 1.07) than discharged 23.97 ± 5.36 , 11.32 ± 1.28) (p<0.001), further confirming the validity of both scores in determining mortality. They also examined the ROC curve for serum creatinine (0.887), blood urea (0.836), MELD score (0.864) and the traditional Child Pugh score (0.738). (Chaurasia et al., 2013).
In a retrospective cohort study conducted by Si-Zhe Wan and her colleagues in First Affiliated Hospital of Nanchang University, on predictability of prognosis by Child PUGH, MELD and ALBI scores in patients with decompensated cirrhosis, it was found that all three methods) proved to be reliable in predicting the mortality for both short term prognosis and long-term prognosis in patients with decompensated cirrhosis. It was recommended that ALBI can be used for assessing short term outcomes, whereas to predict long term outcomes MELD would be of better use [17].
According to Peng et al., Out of 119 papers they deemed to be eligible for a systematic review of Child–Pugh Versus MELD Score for the Assessment of Prognosis in Liver Cirrhosis, 269 comparisons were present between Child Pugh and MELD. 44 papers favored toward MELD, 16 papers favored towards Child Pugh and 99 papers did not find any difference between them, which is statistically Significant, and 110 comparisons did not report any statistical significance. They concluded that MELD and Child Pugh had very similar prognostic significance in most of cases. They also recommended for development of new tests in order to facilitate more accurate prediction the prognosis of patients suffering with liver disease [2].
The goal of this scoping review was to examine the current level of knowledge on the widespread application of Child-Pugh scores in predicting outcomes for cirrhotic patients, and to describe those findings. A comprehensive literature search was conducted to establish the current state of knowledge and identify any gaps in understanding that exist on the topic of the study. The team did not impose any limits on the search in terms of language or approach. Researchers gathered information from the sources by browsing and doing simple searches. The questions posed in the study served as a sort of population terms glossary for the researchers. The original criteria were adjusted and reapplied to better reflect the centrality of the subject that had motivated the scoping review as the research team moved through the process of study selection and developed a deeper grasp of the nature of the available literature.
Information was gathered on publishing mode, year, methodology, country, and outcome factors. Data from the included research was retrieved and summarized by one reviewer, and then checked by a second reviewer to ensure correctness. During the process of assembling and reporting the data, the team was able to identify gaps in the literature using criteria such as study design, issue area, setting, implementation-strategy cluster, related barriers and facilitators, and outcome. The following conditions were set for eligibility in the research: patients had a confirmed diagnosis of liver cirrhosis; Child-Pugh scores were determined; areas under receiver operating characteristic curve were compared for Child- Pugh scores.
Through electronic searches, the team located thirty references. After removing duplicates and reading abstracts for only a handful of publications, the team narrowed the field down to 27 articles for a full-text review, of which 20 were ultimately deemed to be eligible for inclusion. After submitting a query to the database, the team was provided with links to 10 pertinent reports and research from various sources. Nine articles satisfied the criteria for this scoping review.
According to Chiriac commonly employed scores for evaluating liver function are the Child-Pugh and the Model for End-Stage Liver Disease (MELD) [18]. In order to arrive at the Child-Pugh score, the values of serum bilirubin, albumin, prothrombin time, hepatic encephalopathy, and ascites must be determined [19]. In the study conducted by, with equal predictive significance and moderate discrimination, Child-Pugh scores were evaluated in this meta-analysis of their prognostic performance [20]. As anticipated, the Child-Pugh score in the research by [21]. (2019) was related to outcomes and had predictive value for 28-day, 90- day, and 6-month death.
In the review by, it was hypothesized that adding hyaluronan to the Child-Pugh classification of liver cirrhosis would increase its predictive value for the long-term assessment of this condition, and this study tested this hypothesis [22]. A more accurate prognosis for individuals with liver cirrhosis may be made with a CP tweak that included markers of ECM. The diagnostic accuracy of the Child-Pugh classification (CP) for liver cirrhosis is greatly enhanced with the addition of HA, especially when the cause is alcohol abuse.
The Child Pugh and MELD scores were being used as main sources to determine the mortality in prognosis of patients with liver diseases, especially liver cirrhosis. Multiple studies have been conducted since years, to study the accuracy in their predictability and to determine the best score of the two. Over all those studies, it has been proven that both Child Pugh score and MELD faired good enough and has a lot of similarity in their ability of predicting mortality. Even though MELD has better results in many experimental studies, the difference is not huge. MELD score was a better tool to predict the short-term prognosis, especially after TIPS, according to Salerno et al.
According to Boursier et al., Child Pugh is a better tool to use regularly in clinical practice because it is simple, effective and does not fall behind MELD. The addition of factors like serum- creatinine has given a new life to the traditional Child Pugh score and increased its accuracy high, which can be seen in the cohort studies conducted by Papatheodoridis et al, and Giannini et al. Although MELD may have advantage on the traditional Child Pugh score in terms of sensitivity, Child Pugh score has higher specificity than MELD as seen in observational study conducted by Rahimi-Dehkord et al. However, both scores were found to be inferior to Renal failure as a prognostic factor as seen in the observational study by Chaurasia et al. Said et al. suggested that addition of hepatic enchelopathy as a factor will increase the accuracy of MELD score.
Similar to the study by Cui et al. (2022), the Child-Turcotte-Pugh (CTP) criteria have been shown to be a valuable clinical tool in studies evaluating short- and long-term prognosis in patients with cirrhosis using proper statistical methodologies. Despite CTP’s widespread acceptance and use in clinical practice for decades, it was never subjected to the kind of rigorous validation that would have confirmed its reliability and validity in a variety of illness settings and patient populations [23]. Clinically, the CTP classification does not differentiate between a ‘mild’ grade C patient and a ‘severe’ grade C patient in a meaningful way, in part because of the grading system. In addition, it does not include a test for renal function, which is a proven indicator of cirrhosis and acute liver disease prognosis.
According to, an improved prognosis is seen in alcoholic cirrhotic who abstain from alcohol, even if they are severely jaundiced to begin with, but it is unclear whether this is also the case for people with diseases in which bilirubin declines with therapy, such as primary sclerosing cholangitis (PSC) and PBC [24, 25]. Although the CTP score has been shown to be superior to the MELD score in predicting survival in patients with chronic liver disease who are not on liver transplant waiting lists, the exact mechanism by which this advantage is attained remains unknown. Given that the CTP score is an ‘empirical score’ that has never been statistically validated, this comes as a surprise.
Presently, INR is more commonly used than PT by medical professionals. Based on the findings by, the severity and prognosis of chronic liver disease and cirrhosis are evaluated using updated versions of the Child-Pugh score [26]. It is also used in conjunction with the MELD to rank patients in need of a liver transplant. Child-Pugh grading was the first of its kind to categorize the severity of liver failure; however, it is no longer the standard. Patients undergoing liver transplantation are evaluated using the Model for End-Stage Liver Disease (MELD); however, both scores appear to be roughly similar [27]. In patients with hepatic impairment, the MELD score may be a more precise measure of perioperative mortality. The serum bilirubin, creatinine, and international normalized ratio are used in a linear regression model to determine the score (INR).
Patients with end-stage liver disease have been evaluated using a variety of prognostic factors in order to ascertain the best course of treatment. The Child score was the standard for evaluating cirrhosis prognosis until the late 1970s, when it was superseded by the modified Child-Turcotte-Pugh (CTP) score. The CTP scores were found to have similar prognostic values across most instances in a large systematic review, however their benefits varied in some circumstances [28]. Therefore, it is not clear if the CTP score should be abandoned permanently. Patients with end-stage liver disease in a Northern Indian study cohort had excellent predictive CTP scores for 3-month death. For 3-month mortality prediction, however, the CTP score typically performs better [29]. Different clinical contexts and etiologies of liver disease in various parts of the world may affect the efficacy of any given scoring approach for advanced liver disease. The CTP score may be more reliable for a patient with hepatic encephalopathy and ascites because it takes into account these symptoms.
Similar to the findings in study, this review found that the Child-Pugh score and its constituents (bilirubin, albumin, and prothrombin time) remained strong predictors. In spite of this, Child-Pugh score has a few drawbacks [30]. The first problem is that the score used subjective criteria (ascites and encephalopathy) that made it hard to place patients into appropriate illness severity categories. The Child-Pugh score also depends on clinical evaluation, which might lead to scoring variations. The Child-Pugh score does not account for aspects such as the etiology of cirrhosis, the possible combination of numerous causes, or the persistence of a destructive process such as chronic alcohol misuse or chronic hepatitis B infection (HBV), which reflect similar observations by [31]. Despite the fact that its broad illness classifications make it useless when deciding which patients should receive a liver transplant first, it is nevertheless commonly utilized.
Unless further problems (such as hepatocellular cancer or uncontrolled bleeding owing to portal hypertension occur, people in Child-Pugh class A have an excellent medium-term survival without a liver transplant. Patients in Child-Pugh class C are typically the ones who need liver transplantation.
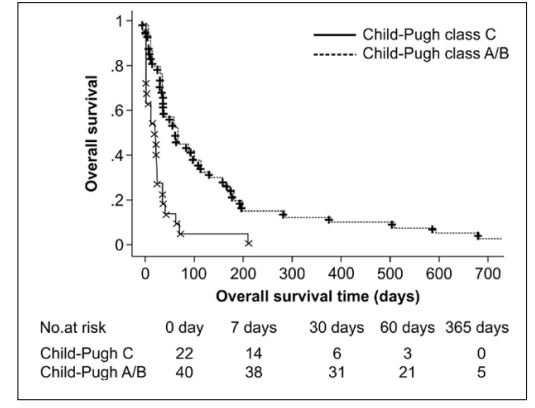
Figure:Comparison between Child Pugh Class A, B, and C [32].
Patients in Child Pugh class B are a varied bunch, since their health can improve gradually over the course of a year or abruptly spiral out of control [32]. Prognostic techniques are urgently needed to determine whether individuals with liver cirrhosis and portal hypertension should undergo surgery. While empiric evaluation was used to construct the CPS classification, several subsequent research have proven that it is predictive in determining prognosis for individuals with liver illness. These investigations showed that the CPS categorization as a whole, as well as each of the five specific clinical characteristics, could accurately predict outcomes.
Ultimately, the Child-Pugh Score is a prognostic indicator of the progressive severity of liver disease and an individual’s likelihood of survival. The prognosis and likelihood of dying are both affected by the severity of liver damage, which can be estimated with this score. Using this information, doctors will be able to better determine whether or not a patient is a good candidate for elective surgery [7]. In addition, knowing one’s score might aid in determining what kinds of permanent modifications to one’s way of life might help mitigate the likelihood that one’s score will worsen over time. The severity of chronic liver disease can be measured using the Child-Pugh score and stratified into five groups. A therapy plan can be better mapped out using this information. The severity of liver illness is measured by ascites, bilirubin and albumin levels in the blood, prothrombin time, and encephalopathy, and this data is used in the modified Child-Pugh classification. Class A (well compensated disease) is indicated by a Child-Turcotte-Pugh score of 5 or 6, class B (substantial functional compromise) by a score of 7 to 9, and class C (very severe disease) by a score of 10 to 15 [9].
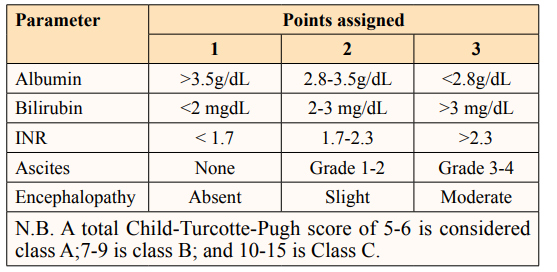
Figure: Different Parameters Child Pugh Score [9].
There were two major flaws in this study. First, while many papers were included in the systematic review, not all of them satisfied the criteria for our meta-analysis. Second, the studies that were included in the meta-analysis had varying threshold values for the Child-Pugh score used to determine the patient’s prognosis. Thus, we were unable to determine reliable cutoffs for distinguishing between high- and low-risk patients.
The aim of this study was to provide a review of the literature comparing Child-Pugh scores for the purpose of determining prognosis in liver cirrhosis. The prognostic impact of higher and lower Child-Pugh scores was roughly the same. However, given their unique advantages for some conditions, more research may be required to specify both the patients for whom the Child- Pugh score should be used and the circumstances under which it should be used to determine prognosis. Its original purpose was to predict surgical mortality, but today the Child-Pugh score is used to establish a patient’s prognosis, as well as whether or not intensive care or a liver transplant are warranted. Proposing new ratings based on prospective research is also necessary for a more precise assessment of the prognosis of patients with liver disease. The Child-Pugh score, however, is also subject to differences in scoring because to the importance placed on clinical examination. Cirrhosis can have several causes, and the Child-Pugh score does not take into consideration the etiology, the possibility of many causes, or the persistence of a damaging process such chronic alcohol abuse or chronic hepatitis B infection (HBV). Commonly used despite its ineffectiveness in prioritizing people in need of a liver transplant due to its overly generalized ailment categories; to conclude both Child Pugh and MELD scores has their own significance. Child Pugh score is a better parameter when used in a generalized settings where in. MELD is most effective when used for decompensated patients. Child Pugh score performed better in predicting generalized, intermediate to long term prognosis but MELD was best for short term prognosis, but both the scores are far from perfect and we need a new scoring system to have an accurate and reliable method for calculating the prognosis of the patients with liver disease.
