Author(s): Aimen Vanood1, Rafid Kasir1,2* and Jad Khalil 1,2
Background: Epidural steroid injections (ESI) are commonly used in treatment of chronic lower back pain. Conus medullaris and cauda equina syndromes are rare complications of ESI. However, these typically occur after multiple injections within a few minutes to hours. Some reported cases are also transient, with patients completely regaining neurological function. We discuss a unique case of a patient developing conus medullaris syndrome over 24 hours after a single epidural steroid injection without resolution of symptoms.
Case Presentation: An 88-year-old male patient was admitted for lower extremity weakness the day after receiving an ESI for chronic lower back pain. MRI revealed T11-L5 subdural hematoma and a diagnosis of conus medullaris syndrome was made. After surgical decompression he regained some strength but permanent deficits remained.
Conclusion: Our case highlights the dangerous complications of epidural steroid injections and emphasizes the need for other treatment alternatives to alleviate CLBP.
Lower back pain is a common musculoskeletal conditions, affecting over 80% of adults [1,2]. Pain lasting greater than 12 weeks is characterized as chronic lower back pain (CLBP). Often, this pain is radicular in nature, with patients feeling pain from their lower back down to their buttocks and lower extremities. While vertebral disc herniation, spinal stenosis, and malignancy are the most common etiologies of radicular pain, the pain itself is caused by the inflammation of the affected nerves, rather than the compression itself [3].
One treatment modality for controlling CLBP are epidural steroid injections (ESI), with lumbosacral injections use more than quadrupling over the past two decades [4]. The procedure begins with anesthetizing the skin and subcutaneous tissue. A fluoroscopicguided approach is used to position the needle. In an interlaminar approach, the needle is inserted until it pierces the ligamentum flavum, while a transforaminal approach involves advancing the needle below the 6’o clock position of the pedicle. While injection site pain and infection are common complications of ESI, more serious adverse events, including paralysis, have been reported [5]. It remains unclear how steroid injection lead to paralysis, with one hypothesis being that particulate steroid matter is propelled into the radiculomedullary artery supplying the spinal cord [6].
Rarely, conus medullaris and cauda equina syndromes are reported as developing after treatment with ESI. Conus medullaris refers to the tapered end of the spinal cord, extending from T12 to L2, while the cauda equina is the bundle nerve roots at the distal end of the spinal cord [7]. While lower motor neurons comprise both, only the conus medullaris also consists of upper motor neurons. For this reason, cauda equina syndrome is thought to have better outcomes because lower motor neurons have greater propensity to regenerate [8]. Imaging is important when differentiating between these syndromes as they clinically overlap and require a high degree of suspicion to diagnose. Complications include paraplegia, saddle anesthesia, and urinary and fecal deficits [9].
We present the case of an 88-year-old retired anesthesiologist admitted for worsening lower extremity weakness. The day prior, he received an ESI for CLBP secondary to spinal stenosis. He presented with increasing lower extremity weakness over the course of the day. On physical exam, his muscle strength was found to be 0/5 bilaterally in the lower extremities, but sensation remained intact. He had no bowel or bladder incontinence. An MRI was performed revealing a T11-L5 subdural hematoma [Figure 1] compressing and displacing the conus medullaris and cauda equina anteriorly.
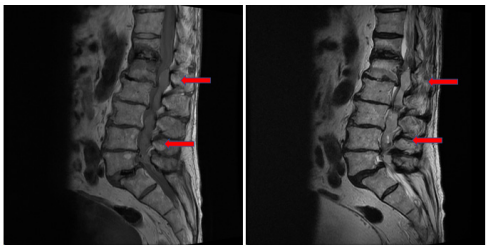
Figure 1: T1 [left] and T2 [right] weighted MRI of lumbar spine showing subdural hematoma (red arrows) extending from T11 to L5.
The patient was treated with surgical decompression of the hematoma (via bilateral laminectomy, medial partial facetectomy, and foraminotomy over T12-S1). Deficits remained constant throughout admission with minor improvement in right hip strength to 3/5. These findings are consistent with conus medullaris syndrome which did not regress with initial surgical intervention, leaving the patient with significant functional deficits. The patient was discharged after 49 days of hospitalization with recommendations to continue physical therapy.
This is the first case of conus medullaris syndrome developing over 24 hours after a single ESI in an otherwise neurologically uncomplicated patient. The majority of cases of conus medullaris and cauda equina syndromes reported occur after a patient’s second steroid injection [10,11]. Symptoms most commonly manifest within a few minutes to hours of the injection and in some instances resolve within a few hours [12-15]. There was one reported case of cauda equina syndrome developing after one day in a patient who received a single ESI. However, the course was complicated by a paraganglioma at the L2/L3 level which the needle penetrated [16]. There was a case reported of cauda equina syndrome developing 13 days after a patient’s third epidural steroid injection, however this was in a patient with concurrent staphylococcus meningitis that had developed after the patient’s second injection [17].
Our patient adds to the growing body of literature highlighting the dangerous complications of ESI. This raises the need for treatment alternatives to alleviate CLBP in the adult population.
• Epidural steroid injections are widely used in the treatment of chronic lower back pain.
• This case highlights a unique case of conus medullaris syndrome occurring days after a single epidural steroid injection.
• Epidural steroid injections can lead to significant adverse outcomes and should be used with caution.
