Author(s): Adel Hassan Mohamed Hassan*, Tarek Huissen kamel, Nesreen Ahmed Mosalam and Sherif Hasanein Ahmed
Background: The most common non-cutaneous malignancy for men is Prostate cancer (PCa). PCa diagnosed by biopsy and PSA detection. Bone metastasis (BM) causes a lot of complications, such as bone pain and pathological fracture that cause overall compromised quality of life. Bone scintigraphy (BS) is commonly used for monitoring and detection of (BM).
Objective: To correlate between serum PSA level and BM in PCa patients on series of 250 patients through detecting PSA levels and BSs.
Patients and Methods: In the present study Patients were stratified (group A) & (group B) according to BM. Out of the 250 patients, 180 patients (Group A localized PCa) were with age range from 57 -92 years, the remaining 70 patients (Group B metastasis PCa) the age range was 53-88 years. Prostate specific antigen (PSA) level for both groups were detected.
Results: By comparing group A and group B there was a highly significant difference in PSA value in favor of positive BS group (p-value < 0.001). The present study recommends BS in asymptomatic patients with PSA above 60 Ng/ml.
Conclusion: PCa is the most common malignant non-cutaneous tumor for men. The most common spread for PCa is bone spread. Age doesn’t correlate with BM in PCa patients. PSA total show highly significance with BM in PCa patients. PSA cut-off value for BM in PCa patients was 60 Ng/ml so it was recommended to perform BS for asymptomatic patients with PSA total above 60 Ng/ml.
The most common diagnosed malignancy in American men is PCa. Most often of PCa patients diagnosed in men ages range from 55 - 74 years (71 % from newly diagnosed cases) . The second cause of cancer death between American men is (PCa), and considered the 3rd cause of death from cancer all over the world [1-4]. The digital rectal examination (DRE) and a (PSA) test are the common tools for diagnosis PCa. Although 0-4 Ng/ml PSA levels is mostly considered the normal value, there is no accepted cut-off value worldwide. A lot of grouping scales were established for preoperative PSA levels. But the most commonly used one is low-risk (PSA<10 ng/ ml), (PSA 10-20 ng/ml) for medium-risk and (PSA>20 ng/ml) for high risk. PSA level is the most commonly used test for detecting who need to perform biopsy. However, a lot of studies stated that tumor aggressiveness may be correlated with level of PSA . The low specificity and high sensitivity of PSA testing in identification of PCa may be a drawback in clinical apply. Using PSA testing alone resulted in reduction of specificity because of the effect of prostate volume and alternative factors like manipulation and infection. Even with this disadvantage, however, PSA activity continues to be used in clinical apply as long as no new biomarkers are accepted for the detection of (PCa). The general cutoff value for the PSA level is 4.0 Ng/mL. With the use of this (PSA) cutoff value, cancer diagnosis percentage for 10- to 12-core biopsy ranges from 35% to 42.3% [5-10]. We’ll study the relation between the (PSA) and (BMs) in PCa within the last 5 years in El Demerdash Hospital (Ain Shams University).
This study aims to determine the association between (PSA) level and (BM) in PCa patients and to identify the cut-off value of the PSA total as an indicator for (BM).
Our present study is a retrospective study. It was conducted at Clinical Oncology & Nuclear Medicine Department, AINSHAMS University.
Two hundred fifty files of PCa patients were collected between January 2015 and December 2019 in Eldemerdash hospital AIN SHAMS University. They were included to participate in this study on the basis of the following criteria:
Sex: Male patients. Age: from 18 till 90. Biopsy proven PCa (adenocarcinoma). Baseline serum PSA level.
Patients with history of other malignancies. Double primary malignant tumor. PCa patients with visceral metastasis. Patients having previous therapy for prostatic cancer.
The following data were collected from patients’ files: Age. Clinical examination. Assessment of PSA level. Gleason score (GS). BS. Pathology report. MRI pelvis if present. CT pelvis if present. All patients were diagnosed by biobsy. (GS) was determined. Serum PSA concentrations were determined based on enzyme immunoassay. Normal PSA range in our laboratories is 0.0-3.0 Ng/ml. BS used to determine BM. The outcome of the results was tabulated and analyzed to correlate between PSA value and BSs results and also if there was a relation between Age and (GS) with the BM.
The Tandem-R PSA, monoclonal immuno-radiometric assay used for detecting The serum concentration of PSA with the normal range set between 0 and 4.0 Ng/ml.
(GS) - the sum (2-10) of the major + minor glandular patterns. For each pattern, range is from slight disorganization (1) to anaplastic (5).
The results of BSs were interpreted as BM if increased tracer uptake. Patients were diagnosed metastasis through BSs or CTs or MRIs. The results of BSs were considered free of metastasis under the following circumstances: No detection of abnormal increased radiotracer uptake. Radiotracer uptake was characterized by benign and medical disease (e.g. trauma, arthritis and fracture).
All measurement data were calculated as mean ± standard deviation (SD). The receiver operating characteristic (ROC) curves were used to get the sensitivity and specificity of (PSA) and (GS) for detecting (BM). The Pearson’s correlation-coefficient test was used to assess the correlation between Age, PSA and (GS). All statistical analysis was performed with SPSS 20.0 (IBM). Twosided P-values of less than 0.05 provided evidence for statistical significance.
A total of 250 patients with PCa were retrospectively analyzed based on histopathological investigation which were all prostatic adenocarcinoma. Patients were divided into two groups upon BM. Out of 250 patients 180 were with localized PCa considered as group A. the remaining 70 patients were with BM considered as group B (Figure 1).
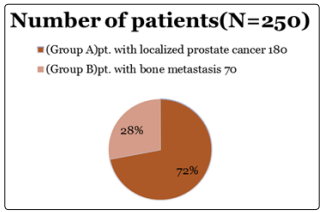
Figure 1: Number of patients with BM & localized PCa patients
The PSA levels were determined in all patients and (GS) as predictors for BM. The age range from 53-92 years for all patients (N= 250), with a mean age of 71.00 ± 6.31 years. Out of the 250 patients, 180 patients (Group A with localized PCa) were with age range from 57 -92 years and a mean age of 70.65±5.99, the remaining 70 patients (Group B with metastasis) the age range was 53-88 years and a mean of 71.89±7.03. However, no significant difference between the mean ages of the patients of both groups was detected (table 1).
| Metastasis | N | Mean | Std. Deviation |
Minimum | Maximum | p-value | |
|---|---|---|---|---|---|---|---|
| Age | (Group A)No | 180 | 70.65 | 5.99 | 57.00 | 92.00 | (0.165) Not significant |
| (Group B)Yes | 70 | 71.89 | 7.03 | 53.00 | 88.00 | ||
| Total | 250 | 71.00 | 6.31 | 53.00 | 92.00 | ||
The PSA levels in all patients (n=250) were ranging from 2.11 to 1404 Ng/ml with mean value of 111.02 ± 238.18 while the PSA levels in patients with localized PCa (Group A, n=180) were ranging from 2.11 to 196 Ng/ml with mean value of 38.28±40.87 on the other hand in Patients with positive BS (Group B, n=70) the PSA levels were ranging from 54 to 1404 Ng/ml and a mean value of 298.07±388.69.
By comparing group A and group B, a highly significant difference in PSA value was detected for positive BS group (p-value < 0.001) (Table 2).| Metastasis | N | Mean | Std. Deviation |
Minimum | Maximum | p-value | |
|---|---|---|---|---|---|---|---|
| Age | Group A | 180 | 38.28 | 40.87 | 2.11 | 196.00 | Group A |
| Group B | 70 | 298.07 | 388.69 | 54.00 | 1404.00 | ||
| Total | 250 | 111.02 | 238.18 | 2.11 | 1404.00 | ||
The (GS) levels were ranging from 4 to 10 in all patients (n=250) as well as group A and B cases. The mean values were of 6.67±1.27, 7.24±1.48 and 6.67± 1.27 respectively. When comparing (GS) levels of patients with positive BS and localized PCa group there was a statistically significant difference in favor of patients with BM with cut-off value of 7 (p value = 0.003) (Table 3)
| Metastasis | N | Mean | Std. Deviation |
Minimum | Maximum | p-value | |
|---|---|---|---|---|---|---|---|
| Gleason score | No | 180 | 6.67 | 1.27 | 6.00 | 10.00 | (0.003) |
| Yes | 70 | 7.24 | 1.48 | 6.00 | 10.00 | ||
| Total | 250 | 6.83 | 1.35 | 6.00 | 10.00 | ||
When calculating PSA cut-off value we found that when PSA is 60 Ng/Ml, it gave the most combined sensitive and specific values as out of the 70 patients (Number of patients above 60Ng/ml) 65 were with BM and only 5 patients were localized PCa, on the other hand the number of patients below 60Ng/ml was 180 patients. 175 patients were localized PCa and just 5 patients ((GS) >7(8, 8, 9, 9, 9)) were with BM. Table (4) Figure (2).
| Numb. Of pt. above cut of value | Numb. Of pt. below cut of value | |
|---|---|---|
| Total (N=250) | 70 | 180 |
| Total (N=250) | 5 | 175 |
| Pt. with BM (Group B) | 65 | 5 |
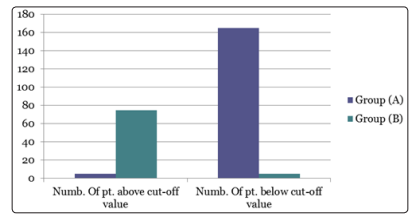
Figure 2: Clustered column showed the number of patients in Group A and B above and below cut-off value
When calculating PSA cut-off value it gave the most combined sensitive and specific value at the PSA 60 Ng/Ml. compared to other values (40,50,70) (Table 5)| cut point | Sensitivity | Specificity | Accuracy | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|---|---|
| 40 | 100.0% | 70.0% | 78.4% | 56.5% | 100.0% |
| 50 | 100.0% | 78.9% | 84.8% | 64.8% | 100.0% |
| 60 | 84.3% | 82.8% | 83.2% | 65.6% | 93.1% |
| 70 | 81.4% | 82.8% | 82.4% | 64.8% | 92.0% |
Sensitivity and specificity were 84.29% and 82.78% respectively with +ve predictive value 65.56% with PSA cut-off value of 60Ng/ ml. Sensitivity and specificity was 77%, 41% respectively with +ve predictive value of 34% with (GS) of 7. Another evidence by comparison to examine that PSA total is more appropriate to be considered as a metastasis marker, Table (6).
| Sensitivity | Specificity | (+ve) predictive test |
(-ve) predictive test | Accuracy | |
|---|---|---|---|---|---|
| PSA Total | 84.29% | 82.78% | 65.56% | 93.13% | 83.20% |
| Gleason score | 77% | 41% | 34% | 82% | 51% |
Shows that PSA total at 60Ng/ml is more sensitive (84.29%) and specific (82.78%) compared by (GS) (77% and 41%) for both sensitivity and specificity respectively. PSA total get 65.56% for (+ve) predictive test and 93.13% for (-ve) predictive test with accuracy 83.20% but (GS) at 7 get 34% for (+ve) predictive test and 82% for (-ve) predictive test with accuracy of 51%. We noticed that the 5 patients with PSA <60 Ng/Ml with positive BS their Gleason core was >7 (8, 8,9, 9, 9) The results showed that serum levels of PSA and (GS) are increased in patients with BM and combined detection of the two markers could improve +ve predictive value.
A receiver operating characteristic curve, or ROC curve, is graphical plot that illustrates the diagnostic ability of a binary classifier system as its discrimination threshold is varied. (Figure 4) shows that the area under ROC curve for PSA total was 0.924 with std. error 0.016 (p-value= 0.000) (figure 3)
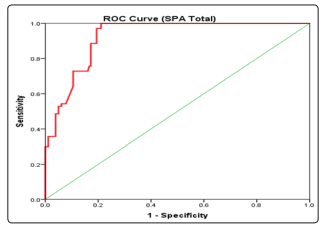
Figure 3: Shows ROC curve for PSA total
while for (GS) area under ROC curve was 0.619 with std. error 0.040 (p-value=0.003) (figure 4)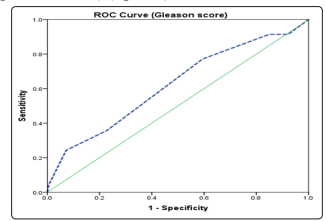
Figure 4: Shows ROC curve for (GS)
So, both PSA and (GS) can be considered as markers for metastasis but PSA is more appropriate as the area under its ROC curve is larger than the area under the (GS) ROC curve (figure 5).
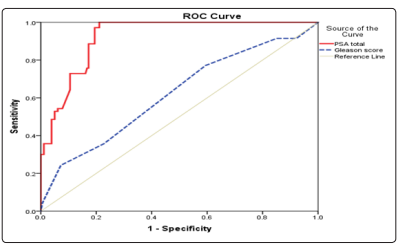
Figure 5: Show ROC curve for both PSA total and (GS)
Using 2 tailed test and Pearson correlation ,There was a significant relation between PSA total level and (GS), while age of the patients has no correlation with both PSA total and (GS) ( P= 0.370 and P=0.989 ) respectively.
This study is designed aiming to determine the association between PSA level and BM in PCa patients. Diagnosis of BM secondary to PCa changes patients’ treatment significantly. Nowadays the gold standard for detection of (BM) is (BSs) (11). Diagnosis of (BM) with (PCa) patients is important in predicting prognosis, and detecting or preventing complications happened by progression of the disease. However, if all newly diagnosed patients with (PCa) are offered (BSs) as the routine investigation, an increase in incidence would suggest an increasing load on the system of the health care. It is thus very important to get a balance between cost and benefit, associated to develop a formula to be the indication of a baseline (BS) (13).
Bone metastasis considered as one of the strongest negative prognostic factors for (PCa) as it not only compromises the survival outcome but also hampers quality of life in these patients (14). The serum PSA and biopsy (GS) are the independent parameters defined by many studies which can predict the occurrence of BM (15). However, the optimal cut-off of PSA level for defining high-risk disease for metastatic BS has always been a matter of argumentation. Currently, the American Urological Association and the EAU do not recommend staging BS in patients with welldifferentiated PCa with PSA <20 Ng/Ml (15). This inference was made from the studies which included western cohort. Besides BM incidence in patients with low PSA <20 Ng/ml is much higher in Asian men compared to western countries (14). It is thus possible that there is difference in intrinsic biological behavior of PCa between different geographic origin, race, and ethnicity.
In our study, 250 PCa patients were collected from 2015 till 2019. They were divided into two groups. Group (A) patients with localized PCa (N=180) and group (B) with BM (N=70). We determined PSA cut-off value and it was 60 Ng/ml. 175/180 (Group A) were with serum PSA <60ng/ml while only five patients were with serum PSA >60Ng/ml. And out of 70 patients (Group B) 65 patients were with serum PSA >60Ng/ml and only 5 patients were with serum PSA <60Ng/ml. Serum PSA at 60Ng/ml showed 84.29% sensitivity and 82.78% specificity (p value =0.001) highly significant, compared to (GS) 77% and 41% for sensitivity and specificity respectively for (GS) 7 (p-value=0.003) significant. In correlation between serum PSA and (GS) they showed positive correlation between each other. However, age was not found to be a predictor for BM (P =0.165) as reported in the literature. The prevalence of BM with higher (GS) >7 was established (P = 0.003). Our collected data from performed BSs support studies published previously confirming the close link between serum PSA level and BS positivity. A positive relation between the PSA level and the incidence of BM was found in our study (P = 0.001 with 95% CI of 0.893-0.954).
The incidence of BM in newly diagnosed prostate carcinoma in our study is (28%) comparable to other studies (0.8-50%). Even it was comparable to the other adjoining Asian nations, such as Pakistan (33%), China (33%), Indonesia (36.8%). It grossly differs with reported American (14%). and Italian (2.5%) studies. The incidence of BM in newly diagnosed prostate carcinoma in our study is comparable to Miller DC, study which reported near onefifth of the newly diagnosed patients will have a positive BS on initial evaluation (16-19). PCa remains disease of old age. In our study, mean age of presentation (71 ±6, 31 years) matches data provided by UK national statistics. Which shows incidences in UK from 2009 till 2011, men aged 75 years and over were 36% of cases, and only 1% were diagnosed in the under-50s.
Our results are comparable to other studies beyond Age. A study was done by Sharma et al. (12) on 89 patients aged 50 to 95 years, with a mean age of 71.4 + 8.3 years patients All 89 cases were histologically proven adenocarcinoma. In our study patients aged 53-92, with mean age of 71.00 +6.31. Another retrospective study was done by Lin et al. on 703 patients histologically proven adenocarcinoma. They reported mean age of 69.9 which correlate with the mean age in our study which is 71.4 . Another study was done by Chen et al. in Wuhan, China. 308 patients aged 73.1±8.9. Out of 308 patients 183 recorded with negative BS aged 73.0±8.7.The other 125 aged 73.1±9.2. In our study, cases with negative BS (N=180) aged 70.65±5.99.On the other hand cases with positive BS (N=70) aged 71.89 ±7.03. Another study demonstrates our results a study done by Chien et al. on 336 newly diagnosed PCa patients. Aged 71.9 ± 8.6. 64 patients recorded positive BS aged 71.3 ± 9.7 and 272 patients with no metastasis aged 72.1 ± 8.3. Our result incorporate the recommendations of European Association of Urologist (EAU), American Urological Association (AUA) and American Joint Commission on Cancer (AJCC), staging BS is not mandatory in patients with PSA < 20 Ng/ml and GS < 8, with no bony symptoms. Our results showed that we can increase the threshold of BS to 60 Ng/ml in asymptomatic patients with GS >7. Ito et al. declared an incidence of 36% (13/36 patients) of (BM) with PSA ≤ 10 Ng/Ml in Japanese mass screening program. Another study from China by Yang et al. (20-24) detected BM in 19% (5/26 patients) of patients with PSA < 20 Ng/Ml. In our study there were no metastatic PCa patients with PSA < 20 Ng/ml that indicates for an aggressive behavior of PCa in Asians as compared to Caucasians or it may be due to most of patients presented with advance stages (12). Indian studies had shown low incidences of BM in contrast to other Asian studies when serum PSA <20 Ng/ml. Another study by Singh, O. a number of sixty eight newly diagnosed (PCa) patients performed BS was retrospectively analyzed. Four groups were patients divided into upon their PSA level: The PSA level of the first group range from 0 to 10 Ng/ml (n = 4), the 2nd group was with PSA level range from 10.1 to 20 Ng/ml (n = 13), 3rd group had PSA levels 20.1-100 ng/ml (n = 23), and PSA >100 for the 4th group (n = 28).the results showed no incidence of BM proven by BS (0 out of 4) for PSA level 0-10 ng/ml; 38.46% (5 out of 13) for PSA level 10.1-20, 60.87% (14 out of 23) for PSA level 20.1-100 ng/ml, and 100% for PSA >100 (P < 0.005) (95% CI 1.01-1.1). For cut-off value of PSA ≤10 Ng/ ml, 100% and 19.05%sensitivity and specificity were, respectively, with 73.44% positive predictive value (14). Sharma mentioned that patients with PSA≤10 Ng/ml or simultaneously PSA≤50 Ng/ml and (GS)≤7 and clinical stage≤T2, BS is not mandatory. This is in accordance with EAU guidelines (12). Another study by Randi showed that at PSA cut-off value of 50 Ng/ml, BM was 77% in his study which showed the best sensitivity and specificity at PSA cut-off value of 50 Ng/ml.
In our study 2.9% from patients with BM ≤ 60Ng/ml, henceforth a recommendation to follow western trials for initial evaluation and for further researches to confirm not to perform BS when PSA ≤60Ng/ml in asymptomatic patients with (GS≤7). Also there are a lot of studies recently on PSMA PET/CT and its relation with (GS) PSMA PET/CT scans show that the SUVmax increases with increasing grade of the tumor. For instance, lower grade tumors (Gleason 3+3 and 3+4) typically have SUVs ranging from 5.9-9.6. Higher grade tumors (>Gleason 7 ) typically demonstrate much higher SUVmax, ranging from 16-21, Intermediate grade tumors (e.g. Gleason 4+3) have intermediate SUVs, ranging from 8.2-8.8 Thus, while PSMA uptake, as measured by SUVmax, correlates with (GS) it cannot be considered a surrogate for (GS) . 99mTcMDP whole-body BS is a highly sensitive diagnostic method that has been used for years to evaluate PCa BM depends on its cheapness and availability; however, because of increasing of this radiotracer in degenerative, inflammatory and traumatic lesions the specificity is relatively low. PSMA-PET/CT outperforms 99mTc-MDP-SPECT in detecting BM in PCa patients although the two studies can be complementary in some patients. 68GaPSMA is higher in the uptake in bone marrow metastases and osteolytic against osteoblastic metastases. Information derived from PSMA PET and CT complements each other for the best diagnosis of the different types of BM in PCa patients (27-30). Our study recommends performing BS in asymptomatic patients with PSA>60 Ng/ml & (GS) >7 Combined detection of the two markers (PSA & (GS)) could improve +ve predictive value. Our data supports previously published studies demonstrating the close link between serum PSA and BM. The major limitation in the study is that only PSA values and (GS) not tumor grading were included. Tumor grading has been suggested by a lot of authors as useful predictors of positive BSs. It has been stated that the probability of a positive BS increases with advanced stages and higher grades of PCa.
The most common non-cutaneous malignancy for men is (PCa). The most common spread for PCa is bone spread. Age doesn’t correlate with BM in PCa patients. PSA total show highly significance with BM in PCa patients. PSA cut-off value for BM in PCa patients was 60 Ng/ml so it was recommended to perform BS for asymptomatic patients with PSA total above 60 Ng/ml. (GS) shows also significance with BM in PCa patients. PSA and (GS) correlate positively with each other.
