Author(s): Louis Samuels*, Marissa Samuels, Sanjog Kalra and Marisa Cevasco
A 58-year-old man presented with fever, chills, nausea, vomiting, and diarrhea. A presumptive diagnosis of viral gastroenteritis was made and fluid resuscitation was undertaken. An initial nasopharyngeal COVID-19 swab was negative. CT scan of the chest and abdomen showed no acute pathology. The EKG, however, showed ST-segment elevation anterolaterally and an echocardiogram demonstrated severe LV dysfunction. His condition deteriorated requiring intubation. Cardiac catheterization showed normal coronary arteries and elevated right-sided filling pressures. Biventricular VADS were placed percutaneously (BiPella®). His condition failed to improve and support was escalated to VA-ECMO. The patient was transferred to a quaternary care center whereupon a repeat COVID-19 test was positive. Inflammatory biomarkers were markedly elevated. The diagnosis of COVID-19 associated fulminant myocarditis was made. The patient received IV steroids, broad-spectrum antibiotics, and enrolled in a Phase 1 convalescent plasma trial. In addition, CRRT was initiated for renal failure. His condition rapidly improved and mechanical circulatory support was discontinued. He was discharged and maintained on hemodialysis until his kidney function normalized several months later. His Ejection Fraction at the time of discharge was 65%.
The COVID-19 Pandemic in the year 2020 has proven to be a clinical challenge for physicians and surgeons worldwide. Initially believed to be predominantly a respiratory ailment, the systemic effects of this disease have become alarmingly apparent. Multiple organ systems have fallen prey to this virus and the myocardium is no exception [1]. The purpose of this report is to describe a case of COVID-19 associated fulminant myocarditis that presented initially as a gastrointestinal syndrome. Advanced surgical and medical therapies utilizing advanced mechanical circulatory support and anti-viral medications were successful in treating the multi-organ dysfunctions.
A 58-year-old man presented to the Emergency Department in June 2020 with altered mental status and a five-day history of gastrointestinal symptoms (i.e. nausea, vomiting, diarrhea), fevers and chills. He had no past medical or surgical history, worked as a driver/mechanic, (+) smoking and occasional alcohol, and (-) illicit drugs. There was no recent travel and no known exposure to toxic or infectious substances.
He was found to be tachycardic and hypotensive with anterolateral ST segment elevation on the electrocardiogram (ECG). The WBC was elevated with lymphopenia and monocytosis. The liver function test and creatinine were elevated along with a lactic acidosis. A chest radiograph, CT scans of the head and abdomen showed no acute pathology. An initial COVID nasopharyngeal swab test was negative. The presumptive diagnosis was viral gastroenteritis. He was admitted, volume resuscitated, and empirically started on broad spectrum antibiotics.
His condition deteriorated over the next twenty-four hours with the need for intubation and further cardiac evaluation. An echocardiogram showed severe biventricular dysfunction with an estimated LVEF of 15-20%. He was taken for left (LHC) and right heart catheterization (RHC). The RHC showed the following: RA 22 RV 40/15 PAP 34/23 PCWP 18 with an aortic BP 64/58. Coronary angiography showed no pathology. Despite multiple vasopressor and inotropes, the hemodynamic status was poor with the need for advanced mechanical circulatory support. Right and left sided Abiomed Impella® (Abiomed, Inc., Danvers, MA) ventricular assist devices (VAD) were placed percutaneously (BiPella®) with improvement in the blood pressure and reduction in vasopressors (Figure: 1). The devices flowed 5L/min. He was taken to the CCU for further management.

Figure 1: BiPella®
Over the next 24 hours, his condition deteriorated further with an increase in lactic acidosis and decrease in urine output. The decision was made to escalate to Veno-Arterial Extra-Corporeal Membrane Oxygenation (VA-ECMO). A 19 Fr percutaneous cannula was placed in the right femoral artery; a 23/25 Fr percutaneous cannula was placed in the left femoral vein. The right-sided Impella was removed and the left-sided Impella was left in place for LV unloading (Figure: 2). A Biomedicus (Medtronic, Minneapolis, MN) centrifugal pump and Quadrox (Maquet Cardiopulmonary AG, Hirrlingen, Germany) oxygenator were attached to the cannulae. His condition stabilized and arrangements were made for transfer to a quaternary care center for long-term LVAD and/ or transplant consideration.
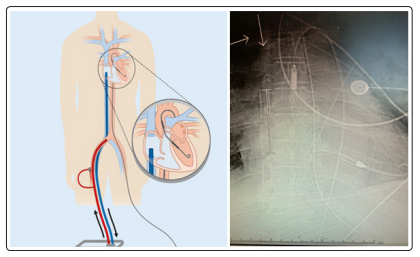
Figure 2: ECPella (ECMO and Impella®)
Upon arrival to the quaternary care center, a repeat COVID-19 Swab was performed and found to be positive. A diagnosis of COVID-19 associated fulminant myocarditis was made. In view of this determination, the patient was enrolled in a Phase-1 convasescent plasma study as well as received dexamethasone (6mg). In addition, he was continued on broad spectrum antibiotics (Cefepime, doxycycline, metronidazole, and Vancomycin). Over the course of several days, his condition improved for ECMO and Impella removal. Repeat echocardiography showed an LVEF of 45-50% which improved to 65% upon discharge approximately three weeks later. Repeat COVID-19 testing following treatment reverted back to negative. At eight months since the event requiring advanced mechanical circulatory support, the patient has completed physical therapy and wishes to return to work.
Fulminant myocarditis requiring advanced mechanical circulatory support is well documented and the results are favorable (ELSO Registry). However, the experience with COVID-19 associated fulminant myocarditis is limited and the use of advanced mechanical circulatory support specifically for this condition is scarce [2-8].
According to a manuscript from China published on April 10, 2020, the first case of COVID-19 fulminant myocarditis was reported [3]. In this paper, a a 63-year-old man was admitted with pneumonia and cardiac symptoms. The troponin I level was elevated and there was diffuse myocardial dyskinesia and a reduced ejection fraction (32%) on echocardiography. In addition, multiple biomarkers were elevated, particularly IL-6. The patient was treated with anti-viral therapy (lopinavir-ritonavir), interferon α-1b, methylprednisolone, immunoglobulin, piperacillin-tazobactam, and continuous renal replacement therapy (CRRT). Eleven days into the admission, the patient was placed on VA-ECMO for combined cardiorespiratory compromise refractory to aggressive therapies. While on ECMO and CRRT, the cardiac function improved dramatically to a normal EF (68%). The manuscript does not report the timing of this improvement and does not indicate that ECMO was discontinued. However, this patient developed a secondary pulmonary infection on the 26th hospital day with bronchial cultures positive for herpesvirus and a blood culture positive for Bacteroides ovalus. Septic shock and DIC developed and the patient died on the 33rd hospital day. The authors believe this to be the first reported case of COVID-19 fulminant myocarditis and if so, the first also to use ECMO for treatment. They also postulate that the elevated IL-6 level represents a cytokine storm and that CRRT and ECMO may play an important role in removal of cytokines from the blood.
A review article by Chow references this case report and comments on the role for VA-ECMO by identifying potential clinical scenarios for ‘Cardiac COVID’: cardiac injury, myocardial infarction with and without obstructive coronary artery disease, viral myocarditis, and decompensated heart failure [7]. These authors concluded that VA-ECMO may be considered in highly selected cases of refractory cardiogenic shock (CS) and echocardiographic evidence of biventricular failure. Published in April 2020 around the same time as the previously cited case report, the authors comment that “we anticipate that patient selection for VA-ECMO in the setting of COVID-19 infection will be a challenging task” and that decision-making for the use of ECMO in this setting should ideally be made by a multidisciplinary CS team.
In a similar case to the one presented in this case report a 44-year-old man was admitted with dyspnea and syncope in March 2020 [8]. He did, however, experience fever, dry cough, myalgia, and diarrhea for seven days prior to admission. Although initially discharged home, he soon returned with worsening symptoms. In addition, he was found to have severe bradycardia, hypotension, and signs of hypoperfusion. An ECG showed a third-degree AV block and echocardiography demonstrated a non-dilated hypokinetc LV with a markedly reduced EF (15%). All the major biomarkers were elevated and the SARS-CoV-2 test was positive. Despite escalating doses of vasoactive drugs, hemodynamic deterioration ensued for which VA-ECMO and IABP were instituted. The presumptive diagnosis was fulminant myocarditis. He was treated with methylprednisolone (1000mg), tocilizumab, hydroxychloroquine, azithromycin, and lopinavir-ritonavir. Several endomyocardial biopsies were obtained and failed to show any inflammatory infiltrates. The clinical status rapidly improved with a marked reduction in the inflammatory markers, lactate levels, and normalization of kidney and liver functions. In addition, LV function normalized (76 %) and VAECMO and IABP were successfully withdrawn after six days. Two days later he was weaned from the ventilator.
In our case, the presentation was gastrointestinal in nature and cardiac dysfunction was not initially considered. However, due to an abnormal EKG followed by a markedly abnormal echocardiogram, further investigation was rapidly undertaken. Indeed, following normal coronary angiography, the clinical scenario was most consistent with fulminant myocarditis, etiology unknown at the time. Escalation of hemodynamic support was necessary when intravenous inotropes and vasopressors failed to stabilize the situation. Since the respiratory function did not initially appear to be compromised, use of biventricular VADS (i.e. BiPella®) were utilized. However, hemodynamic and biochemical deterioration ensued and escalation to VA-ECMO with LV unloading via the left-sided Impella® was initiated. Following transfer to a quaternary care center, a COVID-19 diagnosis was made when repeat testing returned positive. Following treatment-as described in the Case details-including steroids and convalescent plasma- along with ECPella and CRRT, a dramatic recovery was observed and the mechanical support rapidly removed with restoration of cardiac function. He was initially discharged with the need for hemodialysis, but over the course of months the renal function normalized.
In conclusion, the use of advanced mechanical circulatory support for COVID-19 fulminant myocarditis appears to be favorable in a small number of patients described to date. The purpose of this paper is to add to the experience of this condition as the pandemic continues to effect multiple organs, the heart included.
