Author(s): Karl Stonecipher*, Henry Amis and Ben Likins
Introduction: A 22-year-old myopic male presented for LASIK. The patient’s work environment, in the pet cremation services industry, is prone to jobrelated dust and other particles. After an incident-free LASIK, grade 1 Diffuse Lamellar Keratitis (DLK) was found in the patient’s left eye the next day, along with a UCVA of 20/50; the right eye showed signs of inferior punctate keratopathy but was otherwise normal. By day 3, the DLK had progressed to grade 4, also described as Central Toxic Keratopathy (CTK), with mud-crack striae visible despite aggressive hourly topical steroids.
Methods: Case report, incidence report, and literature review.
Results: The patient developed Central Toxic Keratopathy (CTK) in the left eye with a noted hyperopic shift in refraction and mud crack appearance after LASIK on postoperative day 3. Treatment involved hourly topical Difluprenate .05% and Gatifloxacin 0.3%; in addition, a dexamethasone ophthalmic insert (Dextenza®, Ocular Therapeutix, Bedford, MA) was placed in the left eye, with complete resolution occurring within two weeks.
Conclusion: This case demonstrates the use of a dexamethasone ophthalmic insert (Dextenza®, Ocular Therapeutix, Bedford, MA) as a potential treatment of rapidly progressing DLK.
The patient is a 22-year-old male with a normal slit lamp examination and topography. His past ocular history includes a contact lens-related corneal infection of the right eye in 2016 and the left eye in 2017. The cultures were negative. The pachymetry was 504 in the right eye and 509 in the left eye on the initial presentation. He was scheduled for a routine femtosecond LASIK in both eyes using the Alcon Wavelight® FS 200 (Alcon, Fort Worth, TX, USA) to make the flap (110 microns in both eyes) and the Alcon Wavelight® EX500 excimer laser with Phorcides Analytic software (Alcon, Fort Worth, TX, USA). His manifest refraction on presentation was OD: -4.25+2.00x090 and OS:-4.50+2.00x090.
Intraoperatively, both flaps were made without incident. The lifting, laser ablation, and replacement of the flaps were done without incident. On postoperative day one, he was 20/20 OD and 20/50 OS with a bilateral UCVA of 20/20. His right eye had grade 1-2 inferior punctate keratopathy but was otherwise normal; however, his left eye showed grade 1 Diffuse Lamellar Keratitis (DLK) (Figures 1A and 1B, respectively). Difluprednate 0.05% was increased to every hour from every two hours, and
Gatifloxacin 0.3% was continued three times per day. The day two exam was equivocal, but by day three, the left eye UCVA was 20/30, but the DLK exacerbated to grade 4, also sometimes referred to as Central Toxic Keratopathy (CTK), with mud-crack striae present (Figure 2). The refraction in the right eye was plano, with BCVA 20/20 and +0.75 BCVA 20/25.
On postoperative day three, a silicone Super Eagle punctal plug (Katena) was placed in the inferior puncta of the right eye. A Dextenza® ophthalmic insert of 0.4 mg (Ocular Therapeutix) was placed in the inferior puncta of the left eye, the DLK-afflicted eye. The patient was encouraged to continue Difluprednate and Gatifloxacin as before. He was also instructed to use non-preserved artificial tears in both eyes in between therapeutic drops.
Two weeks after placing the Dextenza plug in the left inferior puncta, the patient’s visual acuity had improved to 20/20, and the central cornea was clear with almost complete resolution of the mud-crack striae. The final UCVA was 20/20 OU with a plano- refraction OD and +0.5D spherical OS. The patient's occupational history is significant as he works at a pet crematorium, resulting in exposure to dusty environments and the associated chemicals. This suggests a possible etiology for rapidly progressing DLK, but due to the severe rarity of this condition, more research is necessary for verification.

Figure 1: Slit-Lamp Photography Illustrating Grade 1-2 Inferior Punctate Keratopathy of the Right Eye [A] and Grade I Diffuse Lamellar Keratitis of the Left Eye [B].
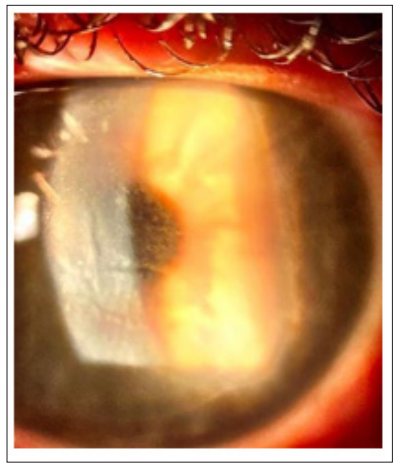
Figure 2: Slit-Lamp Photography of the Left Eye, Illustrating Centralized Condensation of Grade 4 Diffuse Lamellar Keratitis with a Mud-Crack Stria.
To the best of our knowledge, this is the first reported case of CTK associated with exposure to aerosolized dust and chemical debris from an occupational exposure. Secondarily, this report demonstrates the potential therapeutic role of Dextenza®, a dexamethasone ophthalmic insert, for the treatment of CTK.
DLK is a rare, suspected noninfectious complication of refractive surgery. The opacification of the cornea, brought on by white inflammatory infiltrates, results in an interface that resembles sand or grains. DLK is often referred to as the "Sands of the Sahara Syndrome” because of this phenomenon. Fraenkel et al were the first to describe this phenomenon in 1998 [1]. Sridhar reports that tightly entwined in the stroma layer of the human cornea are 200 to 250 types of lamellae, or layers of fibrils, which enable the structural integrity and transparency of the cornea [2].
The condition has been studied since 1998 and is classified into four grades, measured by how the cornea is affected [3,4].
Due to the rarity of this condition and the etiology of DLK not being widely understood, further research is warranted. In a large, prospective series by Stonecipher (personal data), the incidence of CTK was only 0.007% in 4 of 59,135 eyes that had LASIK. The hallmark of CTK is a mud-crack opacification (see Figure 2) of the stromal bed while the flap is spared with stromal tissue loss, with a consequent hyperopic shift and an associated reduction in the quality of vision. Although the etiology of DLK is unknown, Davis and Fahmy report that the inflammatory infiltrates are believed to be caused by surgical manipulation of the corneal surface [5]. Further investigation of the same study concludes that meibomian gland secretions, red blood cells, and other intraoperative inflammatory inciters can also lead to DLK. Non-medical factors, such as exposure from a work and home environment, should be considered as seen in this case.
Sonmez and Maloney postulated that the tissue loss and collapse of the central cornea were due to keratocyte apoptosis, which has subsequently been corroborated in studies using confocal microscopy to show changes in keratocytes at the affected corneal stroma under the flap [6]. They further hypothesized that the underlying etiology of CTK was a toxic reaction to a substance that undergoes photoactivation by the laser. Other theories include a toxic reaction to the powder from gloves, povidone-iodine, secretion of the meibomian glands, or postsurgical debris from the microkeratome blade [7-9]. In our case, it is possible to conjecture that the patient's occupational exposure to chemicals or aerosolized debris contributed to the toxic reaction post-LASIK.
Once CTK is identified, there are minimal to no known treatments to resolve this condition, and therefore most ophthalmologists will observe in the hopes that it will self-resolve over time. In this report, the surgeon opted to treat with a corticosteroid insert in the inferior punctum of the problematic left eye. Previous authors have suggested corticosteroids are not effective in the course of the disease process [6]. However, within two weeks of treatment, our patient had nearly complete resolution of the central corneal opacification, with an associated improved visual outcome. This illustrates a potential therapeutic option for post-LASIK patients complicated by CTK.
The importance of identifying and managing post-operative complications is paramount. Identifying possible etiologies, including past exposures, can help educate patients and physicians on certain risks associated with this surgery. Similarly, the potential treatment of CTK with Dextenza® is hopeful, as there are virtually no current therapeutic options for a patient with this condition other than waiting and watching, and due to the rarity of CTK, long-term studies are difficult to conduct.
