Author(s): Dayan Dissanayaka, Kanakka Hewage Dammika Madhusankha*, Dilruk Rathnayaka and Sanath Bandara
Traumatic brain injury is a common cause of disability among young adults. It causes a huge socioeconomic burden to the society. Management includes a multidisciplinary team approach. Both conservative and surgical options are available as a treatment option, but the outcome is often poor. Decompressive craniectomy is widely practiced surgical option for intracranial hypertension.
Traumatic brain injury is a major cause of disability and death among young adults. In United Kingdom head injury is the commensals cause of death and disability in the population aged 1-40 years [1]. In Sri Lanka studies are found that most of the patients who suffer from traumatic brain injury (TBI) are working age males [2, 3]. Often outcomes of patients who suffer from traumatic brain injury are poor. An observational study done by Samanmalee S Et al found that among the patients sustaining moderate to severe TBI in Sri Lanka reveals that only 46% patients were alive after 6months of discharge and only 20% patients achieved a good recovery [4]. Another observational study done by JP Rankothkubura et al found that After craniectomy for TBI in sri lanka only 27% patients survived up to one year and only 19% achieved good outcome. These show the socioeconomic burden of TBI.
Traumatic brain injury is defined as an impact penetration or rapid movement of the brain within the skull results in altered mental state [5]. Head injury is categorized according to the initial Glasgow Coma Score (GCS).accordingly there are three categories, mild (GCS 13-15), moderate (GCS 9-12) severe (GCS 8 or less). Primary brain injury occurs at the time of the injury and it can be localized or diffuse (diffuse axonal injury). Secondary brain injury occurs from the insults after the primary impact. These includes this includes hypoxia, hypovolemia, cerebral edema and increased intracranial pressure [6].
Primary target of management of TBI is lowering the intracranial pressure medically or surgically if indicated [7]. Here we present a case of a 29 years old man who presented with a traumatic brain injury following an assault who underwent a decompressive craniectomy with temporal lobectomy and good recovery
29 years old previously healthy patient admitted with a sword cut injury to left parioto-temporal region and to the left wrist.
On admission to the accident and emergency department he was maintaining the airway, and the breathing was alright with normal air entry. And oxygen saturation was 100%. He was pale, tachycardic with low volume pulse rate of 150 bpm. His initial blood pressure was 80/60 and dropped to 70/50. Fluid resuscitation started with normal saline followed by uncross matched O negative blood.
His initial GCS was 13/15 and soon after admission he developed a generalized tonic clonic convulsion (GTC) and GCS dropped to 3. The convulsion was managed with intravenous midazolam, and he was intubated using the rapid sequence induction to secure the airway. His both pupils were 2mm in size reacting to the light and random blood sugar was 330 mg/dl.
He was having large deep cut wound in the left temporo-parietal region. His left hand was completely amputated from the wrist joint.
Initial Non contrast CT (NCCT) brain showed left sided compound chipping off sharp cut temporal bone fracture with underlyingfronto-temporo-parietal acute subdural hematoma (SDH) with midline shift. Towards the right-side Cerebral edema and tight brain stem also evident in the NCCT brain.
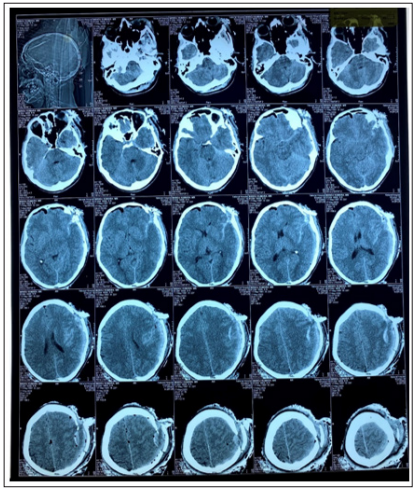
Figure 1: Initial NCCT brain
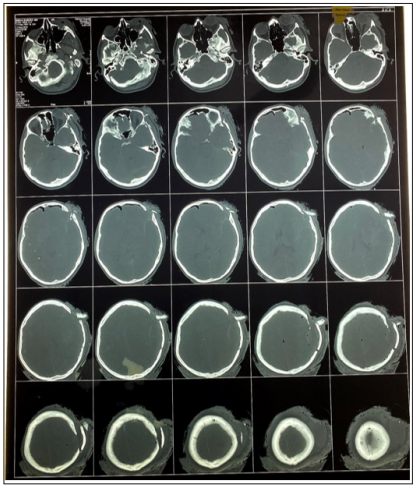
Figure 2: CT Bone Window
Emergency decompressive craniectomy planned and the patient taken to the theater after the intial haemidynamic stabilsation. Decompressive craniectomy was performed through the exsisting sharp cut wound and bone flap removed. After achiveing the haemostasis dura was sutured.during the same time rhe surgery to control the bleeding from the amputaion side was performed with ligation of both ulnar and radial arteries. Pateint was admitted to the ICU for further ventilatory and post-operative care. For the control of seizures patient was on phenytoin.
In the Repeat post-operative NCCT done after 12 hours and there was cerbral odema with features of incresd ICP. Intially the raised ICP managed medically with 3% saline, paralysis and mechanical ventilation. Despite the medical treatment the ICP remained continuasly elevated and planed to do the trmporal lobectomy.
Following day patient underwent the left sided deompression and temporal lobectomy. Patient was admitted to the ICU for post operative care. Repeat CT was satisfactory and there were no features of raised ICP. patient was weaned off from the ventilator after 48 hours. Patient was extubated after 72hours of the surgery and was having satisfactory revovery with a GCS of 14. He was having right sided weakness after the extubation. After 20 days of hospital stay patients motor function recoverd completely and was dischraged from hospital.

Figure 3: Patient before Discharge
Prevention of secondary injury is the cornerstone of the management of traumatic brain injury. This includes maintenance of cerebral perfusion pressure and application of other neuroprotective measures.
Cerebral perfusion pressure (CPP) will depend on intracranial pressure (ICP) and mean arterial pressure (MAP).
CPP = MAP- ICP
Management of ICP will play a crucial role in the treatment according to the equation. Intracranial hypertension after TBI could be due to
1. Traumatically induced mases
2. Cerebral oedema
3. Hyperaemia secondary to vasomotor paralysis
4. Hypercapnia
5. Obstruction of CSF pathways
6. Increased intrathoracic or intra-abdominal pressure [8]
There are clinical symptoms of increased ICP such as headache and vomiting. But in cases of moderate to severe TBI these symptoms are difficult to elicit as in our patient because of reduced GCS. Though the papilledema is a reliable sign it is uncommon after head injury and also difficult to assess. Among Other signs of I raised ICP includes anisocoria and decerebrate posture [8]. In the CT scan signs raised ICP includes cerebral oedema, compressed basal cisterns and midline shift. All these findings were there in our patient’s initial CT scan of the brain.
Prevention or treatment of factors that may exacerbate the intracranial hypertension plays a major role in management. These includes position of the head 30 degrees elevated to allow venous drainage, paralysis and ventilation to maintain normoxia and normocarbia, and prevent seizures and fever [8]. All these conservative methods were employed in our patient.
Acute convulsions can occur because of severe TBI. These categorized as early if they occur within 7 days of the injury, or late if they occur after 7 days of injury. Phenytoin sodium is recommended to prevent early post traumatic seizures although the levetiracetam is increasingly being used [9]. In our patient phenytoin was used as he had an early post traumatic seizure. Hyperosmolar therapy usnig manitol or hypertonic saline also proven to be effetive in controling the intracranial pressure. In some studies hypertonic saline was more effective in reducing the ICP than mannitol. Hypertonic saline has definite advantage over mannitol in hypovolemic and hypertensive patients as mannitol is relatively contraindicated in hypovolemia [8]. In our patient hypertonic saline was used to treat the intracranial hypertension.
Surgical options to treat refractory intracranial hypertension includes resection of mass lesion including evacuation of hematoma, cerebrospinal fluid drainage and decompressive craniectomy (DC) [8, 10, 11].
In our patient decompressive craniectomy was used as a modality of reducing the intracranial pressure. In brain trauma organization guidelines they doesn’t give a level one recommendation on decompressive craniectomy, however recommends a large frontotemparoparietal DC over a smaller one [9]. RESCUEicp trial concluded that decompressive craniectomy in patient with TBI resulted in lower mortality rates and higher vegetative states after six months [12]. In an observational study done in national hospital of Sri Lanka found that following DC after TBI, 27% of patients survive and 19% of them had good outcome at the end of one year [2].
In our patient temporal lobectomy also done in the second opening. Evidence regarding this practice are limited, but a retrospective observational study done by Hakan AK et al found that 60% of the patient survived and all the survivors were functionally independent, but only 10 patients were included in the study. Nussbaum et al also found that 40% of the patients who underwent early decompression with complete temporal lobectomy are functionally independent [13].
In conclusion traumatic brain injury is a major cause of morbidity and mortality among young population. Management of these patient include a multidisciplinary approach including emergency physicians, aneasthetists, neurosurgeons and intensivists. Prevention of secondary injury to the brain by preventing the intracranial hypertension is the cornerstone of the management. To achieve this goal both medical and surgical interventions needed simultaneously in severe or refractory cases.
