Author(s): Jue Wang, Zhongpeng Fu and Hao Zhu*
Uterine septum is one kind of Müllerian duct anomaly with a prevalence ranging from 2.3% [1, 2]. Some cases are asymptomatic which are incidentally detected on the ultrasound and obstetric surveillance is recommended; others are associated with infertility, recurrent pregnancy loss or preterm labor [3- 5]. Expectant management and serial sonographic scanning are required. Salpingography and three-dimensional ultrasound helps to detect uterine anomalies [6, 7]. Hysteroscopic examination is valuable on the condition of either diagnosis or treatment before pregnancy [8]. However, ultrasonographic diagnosis turn to be difficult due to the septa shielded by the fetus and placenta. Here we present a case of delayed diagnosis of uterine septum developed from 14-33 gestational weeks (GW). The initial impression of the sonographic image interfered our judgment.
Uterine septum is one kind of Müllerian duct anomaly with a prevalence ranging from 2.3% [1, 2]. Some cases are asymptomatic which are incidentally detected on the ultrasound and obstetric surveillance is recommended; others are associated with infertility, recurrent pregnancy loss or preterm labor [3- 5]. Expectant management and serial sonographic scanning are required. Salpingography and three-dimensional ultrasound helps to detect uterine anomalies [6, 7]. Hysteroscopic examination is valuable on the condition of either diagnosis or treatment before pregnancy [8]. However, ultrasonographic diagnosis turn to be difficult due to the septa shielded by the fetus and placenta. Here we present a case of delayed diagnosis of uterine septum developed from 14-33 gestational weeks (GW). The initial impression of the sonographic image interfered our judgment.
A 29-year-old-woman gravida 2 para 0 was admitted for an increasing subchorionic cyst at 34+3 GW. The prenatal examination was unremarkable except for an evolving subchorionic lesion detected at 14 GW initially. The patient complained of intermittent vaginal bleeding since then. A mixed echoic mass appeared at the right edge of the placenta in 92x65x55 mm in size (Figure 1). Subchorionic placental hematoma was diagnosed at first impression. Vaginal bleeding ceased at 21 GW and the hypoechoic lesion remained stable between 75-85 mm in maximum dimension (Figure 2) in the sequential scanning until 33+0 GW. Ten days later, at 34+3 GW, the retroplacental structure turn to be homogeneous and lacks blood flow signal on the color Doppler which ruled out an ongoing hemorrhage. But the size of cyst increased to 111x110x69 mm (Figure 3) which was closely adjacent to the right uterus wall and the placenta. There was no report of medication such as aspirin or low-molecular heparin. The fetal growth measurement was appropriate for the gestational age. Both amniotic fluid index and umbilical artery Doppler wave were normal. Non-stress fetal testing was assuring. Her prior abortion was uncomplicated. On admission, her vital signs were stable and she had no uterine contractions. Maternal blood count and coagulation test were checked. In concern of the growing mass, magnetic resonance imaging was performed. As result, a normal placentation was revealed which was located on the left side of septum and the posterior wall of the uterus. Incomplete uterine septum (Figure 4A, B) was detected at the fundus. The same day of sonography confirmed the result (Figure 4C). Finally, the patient underwent selective cesarean section due to breech presentation at 39 GW but the septum was not excised during surgery
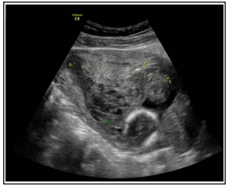
Figure 1: The sonogram showed a 92x65x55 mm heterogenous mixed echogenic mass at 14+3 GW.
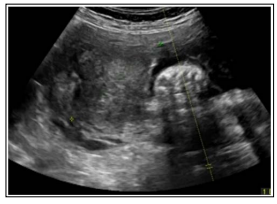
Figure 2: The intrauterine 74x60x25 mm mass was hypoechogenic at 33+0 GW

Figure 3: A large retroplacental cyst was detected at 34+3 GW
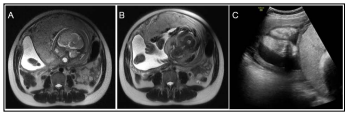
Figure 4: (A) The pelvic MRI showed an incomplete uterine septum at the fundus. The amniotic cavity (fetal limbs were detected) was separated by the septum on MRI (B) and ultrasonography (C).
Our case demonstrated pregnancy with fluid appearance near placenta without common obstetric symptoms that later was discovered to be incomplete uterine septum. Our case illustrated that a detailed examination of patient was critical including both ultrasound and MRI when the findings could not be explained.
Most uterine septum could be discovered earlier especially for infertility evaluation [9, 10]. The symptoms in our case were subtle. Vaginal bleeding at the mid-term was uncharacterized which might be related to so many obstetric diseases. Early pelvic sonographic scans revealed typical findings of subchorionic hemorrhage. Both subchorionic hemorrhage and incomplete uterine septum could contribute to bleeding. In consequent sonography, the signal of the intrauterine mass turned from heterogeneous hypo echoic to homogeneous sonolucent area with clear boundaries at late preterm. Considering the prior presence of subchorionic hemorrhage, the idea of hematoma absorption first came into our mind.
Fluid-fluid appearance near placenta was uncommon during pregnancy. It was detected when placental hematoma was absorbed [11]. Small lesions were asymptomatic so that the early sign was hard to catch on ultrasound. Previous case with massive hematoma ended up with placental abruption at early preterm [12]. Our study provided another unexpected answer of the intrauterine fluid sac in late pregnancy.
The significance of prophylactic septoplasty in patients with uterine septa without prior history of miscarriage or pregnancy complications remains controversial. Successful implantation was described in many studies [13, 14]. In our case, the term pregnancy was uncomplicated so that we did not perform metroplasty during cesarean section.
In the present case, a strong first impression of subchorionic hemorrhage interfered our judgments. When the subchorionic mass dissolved was still obscure. A reasonable MRI played a supplementary role in differential diagnosis. Intense fetal surveillance and sequential sonography will assist obstetricians in the counseling and management.
The authors would like to thank for an English language review.
The authors declared that the research was conducted in the absence of any commercial relationships.
None declared
