Author(s): Abhilash Dhuriya*, Neetika Katiyar, Anupama Dhuria and Kritika Sethi
Purpose: Cervical radiculopathy is one of the common musculoskeletal condition affecting a wide range of population from people involves in desk job to small scale jobs, from a young student to old age population. So it has been of great importance to find out evidence based effective treatment of cervical radiculopathy along with conventional treatment. This study is designed to find out the combined effect of neural mobilization and intermittent traction on cervical radiculopathy
Materials and methods: 30 patients were included in the study and randomly divided into two equal groups. In group A conventional physiotherapy treatment was given along with neural mobilization and in group B only conventional physiotherapy which include intermittent traction and isometric neck exercises treatment was given.NDI (Neck disability index) and VAS (Visual analogue scale) assessment was done on 2nd, 14th and 28th day of treatment.
Results: There was improvement in symptoms in both the group but was more in group A.
Conclusion: The study demonstrated that patients experiencing cervical radiculopathy can improve much earlier and more effectively after neural mobilization technique and therefore provides support to include this technique in conservative management methods of treating patients with cervical radiculopathy for better results.
Cervical radiculopathy is a common disorder characterized by symptoms like pain, numbness, tingling and some times heaviness of arm. Symptoms may be mild, but if turn severe, cervical radiculopathy will be associated with motor weakness [1-3]. It’s a common clinical condition or disorder of a nerve root and most often is the result of a compressive or inflammatory pathology due to space-occupying lesion such as a herniated disc, spondylitic spur, or cervical osteophyte [4-6]. The average annual incidence rate of cervical radiculopathy is 83 per 100000 of population, with an increased prevalence occurring in the fifth decade of life (203 per 100000) [7]. Cervical radiculopathy affects both the genders equally but males show early changes in cervical spine and subsequently leading to cervical radiculopathy, where as in females, the problem arises after the menopause [8]. The location and pattern of symptoms varies, depending on the level of affected nerve root and can include sensory or motor alterations according to involvement of dorsal or ventral nerve root [9-11]. Patients also present with complaints of symptoms which often result in significant functional limitations and disability [12]. Physical therapy interventions commonly used for the management of Cervical radiculopathy include cervical traction, postural education, exercise, and manual therapy applied to the cervical spine and thoracic spine [13, 14]. In addition, Neural Mobilization Technique (NMT) is now days widely used to neural treat pain as this technique mobilizes nerve tissue in conjunction with the surrounding tissue and mostly provides immediate result. Treatment aims to decrease pain related to movement or bodily position and therefore restore normal movement, posture and hence function. Also it may target through local area mobilization or distant from the target nerve tissue but still effective, due to the anatomical nature and relationships of directly and indirectly mobilized tissues [15]. Cervical traction and neural mobilization techniques (NMTs) have been advocated in the management of CR due to their immediate analgesic effect. The objective of this study is to analyse successively the effect of combined NMT and traction as treatment for cervical radiculopathy.
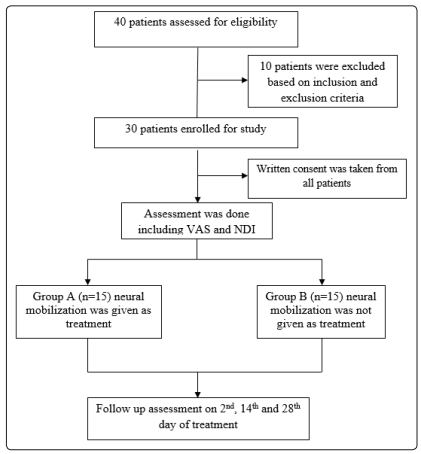
It was a pre-test post-test structured experimental study design. Total number of subjects 40 was assessed in which 30 were assigned fulfilling inclusion and exclusion criteria with their written consent. Group A contain 15 subjects and group B contain 15 subjects. Each group was containing 15 subjects. Subject was selected by convenience sampling method on the basis of the inclusion and exclusion criteria. Each two groups have 15 Subject which were used in this study. Subjects were taken at Integral University, Luck now and research was conducted after approval from institute ethical committee of Integral University, Luck now.
1. Age 18-70
2. Unilateral upper-extremity pain, parasthesia, or numbness
3. 3.3 of 4 tests of clinical prediction rule positive. Those are Spurling test, Distraction test, Upper-Limb Tension Test 1, ipsilateral cervical rotation 60°.
1. History of previous cervical or thoracic spine surgery
2. Bilateral upper-extremity symptoms
3. Signs or symptoms of upper motor neuron disease
4. Medical “red flags” (e.g. tumor, fracture, rheumatoid arthritis, osteoporosis, prolonged steroid use)
5. Cervical spine injections (steroidal) in the past 2 weeks
6. Current use of steroidal medication prescribed for radiculopathy symptoms
Variable: Visual analogue scale (VAS) and Neck disability index (NDI) were dependent variable and neural mobilization technique was independent variable.
Procedure: All participants underwent an initial baseline orthopaedic and neurological assessment and who fulfilled the selection criteria were informed about the study and requested to sign Consent form. Prior to the study pre scores of NDI and VAS were taken. Thirty subjects were divided into two groups.
Group a received conventional physiotherapy treatment along with intermittent traction and neural mobilization of upper limb. Conventional physiotherapy treatment includes neck isometric exercises, trapezius and lavatory stretching exercises and scapular muscle strengthening along with postural care.
Group B received only conventional physiotherapy treatment along with intermittent traction.
Treatment parameters for Neural Mobilization: Treatment was given 4 week for 5 times a week, 3 sets, and 10 repetitions per set with 3seconds hold.
Treatment procedure for Intermittent traction: The machine was set for 15 minute and 1/10 of body weight for pulling action to occur. The traction was put in intermittent mode with hold time 20 seconds and rest time 5 seconds during treatment session. Duration of treatment was 15 minute per session for 4 weeks (5 sessions per week).
Treatment procedure for Conventional treatment: Cervical isometric exercises and scapular muscle strengthening (10 seconds hold with 10 repetitions) trapezius and levator stretching (30 seconds hold with 5 repetitions) were done daily as home exercise program.
Data Collection: NDI and VAS measurements were taken from both groups on day 2, 14 and 28 of the treatment.
Data analysis: All statistical analysis was done by using Statistical Package for Social Science (SPSS) version 20.0. The level of significance of <0.05 was considered to be statistically significant with 95% confidence interval. The independent t test was used to compare the data of both the groups and paired sample t test was used to compare within group changes.
Results:
Thirty patients were taken in the study including 23 males and 7 females. The mean age of patients including in group A was 40.67±6.737 and in group B it was 39.33±6.608. Both the groups were similar age and gender, there was no significant difference in between groups (p value was less than 0.05).
The mean VAS and NDI before treatment in group A were 8.07±1.10 and 83.87±4.373 respectively. In group B mean VAS and NDI before treatment were 7.93±1.163 and 79.20±5.697. VAS and NDI before treatment were not different significantly indicating that baseline values were similar in both groups. Table 1 shows the changes in VAS and NDI in both the groups.
Table 1 showing changes in VAS and NDI in both groups
| Group A | Group B | P value | |
|---|---|---|---|
| Pretreatment VAS | 8.07±1.10 | 7.93±1.163 | 0.775 |
| Day 1 VAS | 7.60±1.242 | 7.40±1.183 | 0.624 |
| Day 14 VAS | 4.00±1.069 | 5.47±0.915 | 0.001 |
| Day 28 VAS | 1.13±0.640 | 3.73±0.884 | 0.000 |
| Pretreatment NDI | 83.87±4.373 | 80.53±4.926 | 0.098 |
| Day 1 NDI | 80.67±4.639 | 73.33±6.532 | 0.001 |
| Day 14 NDI | 44.80±6.038 | 54.00±6.414 | 0.001 |
| Day 28 NDI | 11.20±3.098 | 37.60±7.258 | 0.000 |
There was improvement in symptoms in both the groups on day 2, 14 and 28. On day 2 there was more improvement of patients in group A in comparison to group B but the difference was not significant in VAS changes, but was significant difference in NDI. On day 14 and 28 there was significantly more improvement in group A in comparison to group B in both values i.e. VAS and NDI.
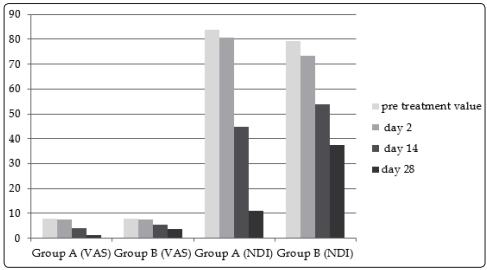
Changes in VAS and NDI in both groups
Table 2 shows paired changes within group and compares the pre treatment values of VAS and NDI with day 2, 14 and 28. All the comparison shows there is significant differences in within groups changes
Table 2 showing changes in VAS and NDI on day 1, 14 and 28 in comparison to pre treatment values
| Differences in mean | Std. Deviation | P value | ||
|---|---|---|---|---|
| GROUP A | VASPRE - VAS1 | 0.467 | 0.516 | 0.004 |
| VASPRE - VAS14 | 4.067 | 0.961 | 0.000 | |
| VASPRE - VAS28 | 6.933 | 1.223 | 0.000 | |
| NDIPRE - NDI1 | 3.200 | 2.242 | 0.000 | |
| NDIPRE - NDI14 | 39.067 | 4.267 | 0.000 | |
| NDIPRE - NDI28 | 72.667 | 6.079 | 0.000 | |
| GROUP B | VASPRE - VAS1 | 0.533 | 0.516 | 0.001 |
| VASPRE - VAS14 | 2.467 | 0.640 | 0.000 | |
| VASPRE - VAS28 | 4.200 | 0.775 | 0.000 | |
| NDIPRE - NDI1 | 5.867 | 5.041 | 0.000 | |
| NDIPRE - NDI14 | 25.200 | 7.476 | 0.000 | |
| NDIPRE - NDI28 | 41.600 | 8.288 | 0.000 |
Results showed that Group A which involves neural mobilization along with traction and exercises showed more improvement in all the days in comparison to treatment given in group B in which neural mobilization was not included in treatment protocol.
In Cervical Radiculopathy, the key concern is to take pressure off the nerve root and improve its blood flow and oxygenation [16]. Neurodynamic techniques are very known which are described extensively throughout the physiotherapy and biomedical literature. Mobilization of the nervous system has a mechanical effect that affects the vascular dynamics, axonal transport systems and mechanical features of the nerve fibers and connective tissues [17]. Neurodynamic or Neural Mobilization Technique (NMT) mobilizes the nerve trunk longitudinally. It is deemed positive with the reproduction of symptoms and / or the presence of antagonistic muscle activity to prevent further nerve bed elongation [18]. Also it facilitate reduction of nerve adherence, nerve gliding and decreased neural mechanosensitivity [19-20].
Conclusion: This study has investigated the additional effects of neural mobilization technique along with conventional treatment in patients experiencing cervical radiculopathy. This research has been demonstrated that patients experiencing cervical radiculopathy can improve much earlier after adding Neural Mobilization technique and therefore provides support for the use of Neural Mobilization technique in the conservative management methods of treating patients with this condition with satisfactory results. The results are important and helpful in treating patients with cervical radiculopathy accurately and with less number of sessions.
Limitations and suggestion: Further studies can be done with larger sample size, with long term follow up and also can be conducted to prove the efficacy of Neural Mobilization for other compressive Neuropathy like Sciatica. Quantitative method can be used as outcome measure.
The authors declare that there is no conflict of interest
