Author(s): Sandra Marcos González, Nerea Martín Cornejo, Jaime Trujillo Hernández and Javier Sánchez Conde*
Alterations in coagulation and decreased platelets are a frequent finding during pregnancy. This case presents an alteration of the PY2 pump of the platelets that contraindicates epidural analgesia and therefore the use of opioids such as meperidine is an option for the treatment of pain during childbirth.
Objective: To show a clinical case of a pregnant woman in whom meperidine was administered as a pain relief method during labor.
Presentation of the case: A full-term pregnant woman in the process of induction of labor who is administered meperidine to relieve pain during labor. A normal delivery occurs after which it is necessary to perform advanced neonatal resuscitation maneuvers due to respiratory depression in the newborn.
Conclusions: The efficacy of meperidine has been proven in various studies, but if the expulsive process is expected to occur within one hour or after four hours from its administration, the use of other drugs such as fentanyl or paracetamol should be considered given the results. similar, to avoid complications such as neonatal respiratory depression at birth.
Alterations in coagulation and decreased platelets during pregnancy are a frequent finding in its follow-up and usually occur in between 6 and 10% of pregnant women. The case that we are going to talk about next presents an alteration of the PY2 pump of the platelets. It must be taken into account that these cases imply a high probability of contraindication to epidural analgesia, therefore, the staff must be informed about which pain relief methods can be used as alternatives if the pregnant woman requests them at the time of delivery [1,2]. In the past, parenteral administration of opioids was widely used to relieve pain during childbirth, although today it is not the first-line therapeutic medication due to its complications, it is still an option if there are contraindications for other methods such as epidural analgesia. The most widely used drug is meperidine, whose onset of action is rapid, from 10 to 15 minutes, as well as being a very cheap drug. Currently, its use is not highly recommended due to its potential adverse effects (serotonergic crises, seizures, interactions with MAOIs...) and its efficacy (more sedative than analgesic effect, since the drowsiness it causes is what relieves the pregnant woman) [2]. Whenever meperidine is administered, it is recommended to use pulse oximetry, administer supplemental oxygen if necessary, and use antiemetics. Meperidine crosses the placenta and reaches the maximum fetal concentration between 2-3 hours after its administration, so it is recommended to administer it when the expulsive period is expected to occur within one hour or after four hours; which is very difficult to predict [3,4]. The objective of this work was to show a case of a pregnancy of a woman who presented this coagulation disorder and in which meperidine was used during labor to relieve pain.
We present the clinical case of a 32-year-old Spanish woman with a 40-week gestation who was admitted to the Delivery Room of the University Hospital of Salamanca in charge of the Obstetrics service for labor induction due to a small-for-gestational-age (SGA) fetus).
Hematological pathology (alteration of the P2Y pump of platelets that does not require controls or specific treatment). Without previous surgical interventions, or identified allergies.
It is the first pregnancy, without previous abortions. It is a pregnancy with a single and spontaneous fetus, with the date of the last menstruation: 02/02/2022.
Height: 169 cm. Weight: 54 kg. BMI: 18.91 kg/m2. Blood pressure: 110/73 mmHg. Blood group: 0. Rh: positive. Negative indirect Coombs. Serology: Immune to rubella and HBV, negative for toxoplasma, HIV and syphilis. First trimester analysis: Hb 11.4.Platelets 281,000. Normal coagulation. THS 1.35. Normal urine culture. First trimester combined screening: Low risk for trisomies 21 and 18. First trimester early preeclampsia screening: Low risk.
Morphological ultrasound within normality. Second trimester analysis: Hb 12. Platelets 272,000. Normal urine culture. O'Sullivan test normal (63/117 mg/dl). PCR SARS-COV 2 positive on 05/10/2022.
Ultrasound of the third trimester: SGA fetus is observed, with percentile 5 and normal fetal and maternal Doppler. Vaginorectal culture of Streptococcus agalactiae: positive. Third trimester analysis: Hb 12.2. Platelets 260,000. Normal coagulation.
The patient was admitted to the delivery room on 11/09/2022 at 5:30 p.m. On admission, a cardiotocographic record (RCTG) was placed: Basal fetal heart rate (FHRb) of 140 bpm, variability according to gestational age, presence of ascents, no decelerations. She does not present uterine dynamics. At 6:30 p.m., a mechanical pre-induction method is started by placing a Cook Balloon. External fetal monitoring is performed with periods of 30 minutes every two hours, observing during the same a GCR similar to that on admission but with the appearance of irregular uterine dynamics (Figure 1).
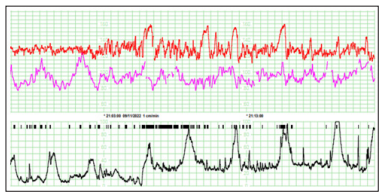
Figure 1: Control RCTG during pre-induction with Cook's balloon
At 00:20 the RCTG is withdrawn to allow night rest. The patient already perceives the uterine dynamics, identifying it as slightly painful. A shower with hot water and application of heat to the lower back is offered as a method of pain relief. As it was an induction of labor for a primiparous woman, it was expected to be long and painful due to the use of synthetic oxytocin for hours. For this reason, the Anesthesiology team had assessed the patient's situation and indicated that epidural analgesia or spinal anesthesia was contraindicated in her case due to the alteration of the P2Y pump. Therefore, for childbirth, the patient should use other pain relief techniques and in case of having to perform a cesarean section, it would be done under general anesthesia. During the night the fetus is monitored with periods of 30 minutes every three hours, until 07:30 on the morning of 11/10/2022, when continuous monitoring begins. The uterine dynamics is regularizing, the woman continues to perceive it as slightly painful, observing how the maternal heart rate increases coinciding with the contraction (Figure 2).
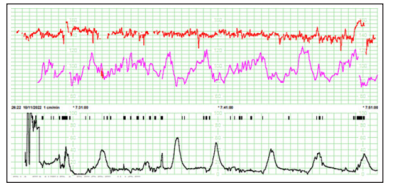
Figure 2: Control RCTG during pre-induction with Cook's balloon
At 11:00 a.m., the pregnant woman is assessed by the Gynecology medical team, who removes the Cook's Balloon and indicates the start of induction with intravenous administration of oxytocin. The oxytocin infusion is started (10 IU oxytocin/500ml of saline). Antibiotic prophylaxis with intravenous penicillin was also started because Streptococcus Agalactiae was isolated in vagino-rectal culture in the third trimester screening. Shortly after starting the oxytocin infusion, the patient reports the contractions as painful. You are offered postural measurements and breathing techniques to use during the pain of each contraction. The patient collaborates, uses all the material resources in the labor room (ball, birthing chair, liana…) and concentrates on each contraction to perform effective breathing to help her cope with each contraction. At 4:30 p.m., the pregnant woman reported unbearable pain. The use of inhalation analgesia with nitrous oxide is offered and explained. At 5:30 p.m., he reported again due to poor pain control, with no relief after the use of nitrous oxide. The Gynecology medical team prescribes intramuscular administration of meperidine (Dolantina®) and haloperidol for pain relief. At 6:15 p.m., internal fetal monitoring was placed through a fetal electrode, due to numerous losses of fetal heart rate, due to the continuous movement of the mother due to intense pain (Figure 3).
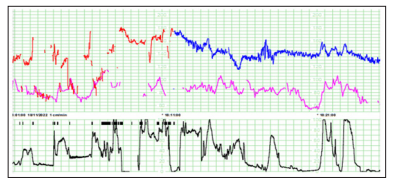
Figure 3: RCTG during induction with intravenous oxytocin and change from external to internal fetal monitoring
At 8:30 p.m. the expulsive process was completed through a normal delivery. A woman was born, weighing 2725 grams, with an Apgar score of 9/9. The newborn is placed in skin-to-skin contact with its mother. At 8:37 p.m., the newborn with 7 minutes of life manifested sudden hypotonia with absence of respiratory effort and generalized cyanosis. The pediatric medical team is notified and advanced neonatal resuscitation maneuvers are started in the resuscitation cradle, beginning with stimulation maneuvers and intermittent positive pressure ventilation with an initial FiO2 of 0.21%. The newborn has a heart rate of 100 bpm and an oxygen saturation of 94%. Upon arrival of the pediatricians, the newborn begins with respiratory effort, so he is left on CPAP ventilation, with good bilateral air entry, mild chest in drawing, and heart rate above 100 bpm with a maximum FiO2 of 0.3%. There is a progressive recovery of muscle tone, colour, and respiratory effort,allowing withdrawal of CPAP and observing vigorous crying, good tone and mobility, and good coloration. At minute 12 of life, he has a heart rate of 150 bpm and an oxygen saturation of 96%. The pH of arterial blood from the umbilical cord at birth is 7.21.
When meperidine crosses the placenta, it causes a decrease in fetal heart rate variability and sedation in the newborn with respiratory depression, making it necessary on several occasions to reverse it with naloxone. For all these reasons, its use during childbirth has been questioned [5]. In the case that concerns us, a decrease in the variability and the baseline of the fetal heart rate is observed (Figure 3). The authors compared several studies on the analgesic efficacy of intramuscular or intravenous meperidine for labor pain control versus other analgesics. Most of the articles showed lower analgesic efficacy compared to meperidine, except for the study by Keskin and colleagues comparing meperidine with tramadol and the study by Tsui and colleagues comparing it. with saline as placebo [6-18]. The study by Keskin et al showed a significant reduction in labor pain after the administration of meperidine compared to tramadol, according to the Wong-Baker visual analog scale, in the first 30-60 minutes, but after the pain control was similar [17]. Harrison et al found that meperidine and promazine had less effective analgesia compared to bupivacaine administered during epidural analgesia [6]. Various publications showed that intramuscular meperidine had significantly lower analgesic efficacy compared to bupivacaine for epidural analgesia, as well as remifentanil and diamorphine for labor pain control [7,8,11,14- 16]. In addition, intravenous patient-controlled analgesia (PCA) boluses of meperidine compared with epidural bupivacaine during spontaneous labor had significantly less analgesic efficacy [9]. Submucosal paracervical block with bupivacaine provided greater pain relief than intramuscular meperidine during labor [10]. Fleet et al and Elbohoty et al compared parenteral meperidine with subcutaneous or intranasal fentanyl and intravenous paracetamol, respectively, showing similar results in labor pain control [12,13].
Given the contraindication of epidural analgesia in the presentation of said clinical case, bupivacaine is not contemplated as a pain relief method. Despite the controversial use of meperidine, its efficacy has been proven in various studies, but if the expulsive process is expected to occur within one hour or after four hours from its administration, the possibility of using other drugs such as fentanyl should be considered. or intravenous infusion of paracetamol given similar results. In this way, neonatal complications such as respiratory depression that may require advanced neonatal resuscitation maneuvers, as in this case, could be prevented.
