Author(s): Aicha Ibourk*, Sofia Haitami and Ihsane Ben Yahya
A frenum, a triangle-shaped fold of tissue connects the lip, tongue and buccal musculature to the alveolar bone in the oral cavity. Any abnormalities in the size and location of the frenum can cause functional and esthetic problems which require surgical excision. Frenectomy can be accomplished either by the routine scalpel technique or by using lasers such as diode laser. The 1st case is an 8-year-old healthy boy with the chief complaint of spacing between his upper front teeth and a palatoversion of the left central incisor. Intraoral clinical examination revealed the presence of midline diastema (1 mm) with high, fibrous labial frenal attachment. The 2nd case is a 6-year-old boy consulted with the complaint of difficulty in speech associated to the limitations of the lingual movements. Intraoral examination revealed partial ankyloglossia. In the 2 cases, the frenectomy was then made with a 980 nm diode laser.
Frenectomy involves the complete removal of the frenulum, including its attachments to the underlying alveolar process. Any abnormalities in the size and location of the frenulum can cause functional and esthetic problems which requires surgical excision. The most common location for the development of frenum abnormalities are maxillary and mandibular central incisors and canine and premolar areas.
These abnormalities can result in gingival recession, development of midline diastema, and speech difficulties. Blanch test is the most commonly used method for the diagnosis of high frenum attachment. It involves application of tension over the frenum by pulling it and visually detecting the movement of papillary tip or any blanching produced [1].
Frenectomy can be accomplished either by the routine scalpel technique, electrosurgery or by using lasers such as diode, Er:YAG, and Nd:YAG [2].
The diode laser is used almost exclusively for soft tissue surgery. The erbium laser can be used for hard- and soft-tissue surgeries. Each laser produces different wavelengths and has advantages and risks. The diode laser is a semiconductor that uses solidstate elements (i.e., gallium, arsenide, aluminum, and indium) to change electrical energy into light energy. The light energy from the diode is highly absorbed by the soft tissues and poorly absorbed by teeth and bone. When used in a contact mode, the continuous-wave diode laser at low power is a useful instrument for excising tissues and reducing bacteria [3].
Therefore, the purpose of the present article is to describe a series of clinical cases of frenectomy, which were approached by diode laser. Additionally, information on the indications, contraindications, advantages and disadvantages of the technique is presented.
An 8-year-old healthy boy consulted with the chief complaint of spacing between his upper front teeth and a palatoversion of the left central incisor. Intraoral clinical examination revealed the presence of midline diastema (1 mm) with high, fibrous labial frenal attachment [Figure 1]. A simple blanch test was performed and positive blanching of the papilla was noted. Various treatment options and their possible limitations were explained to the patient. It was decided to perform surgical (labial frenectomy) and orthodontic procedures for long-term success of management strategies.
Under a small amount of anesthesia, a 980 nm diode laser was used in CW (continuous wave) in contact mode with a power of 15W to prevent tissue heating and therefore carbonization, a saline serum was used regularly during the surgery. The optic fiber was applied perpendicularly to the frenum
Bleeding was minimal and arrested completely after applying pressure with gauze for 10 min [Figure 2]. There was no need for sutures.
A 1-week follow-up showed good mucosal healing [Figure 3]

Figure 1: A midline diastema with high, fibrous labial frenal attachment

Figure 2: immediately post-operative view: no bleeding and no need of sutures

Figure 3: mucosal healing at 2 weeks follows up
A 6-year-old healthy boy patient consulted with the complaint of difficulty in speech associated to the limitations of the lingual movements. Intraoral examination revealed partial ankyloglossia [Figure 1] and was classified as class I [Figure 2] according to Kotlow’s classification. A lingual frenectomy was planned by using 980 nm diode laser. The diode laser was applied at 2 W in a continuous mode perpendicularly to the lingual frenum. Before performing the surgery, the patient received a small amount of anesthetic that was injected with a short needle into the region around the lingual frenulum [Figure 3].
After 14 days the operated area was totally healed and the patient did not present any pain or edema during the healing process.
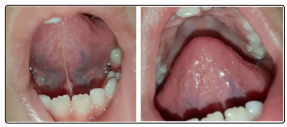
Figure1&2: Ankyloglossia and limitation of the lingual mouvements, front view

Figure 3: Immediately after the laser lingual frenectomy: no bleeding
A frenum is a mucous membrane fold which contains muscle and connective tissue fibers that attach the lip and the cheek to the alveolar mucosa, the gingiva and the underlying periosteum
The maxillary labial frenum develops as a post-eruptive remnant of the ectolabial bands which connect the tubercle of the upper lip to the palatine papilla. When the 2 central incisors erupt widely separated, no bone is deposited inferior to the frenum. A V-shaped bony cleft between the two central incisors and an abnormal frenum attachment results. The mandibular frenum is considered as aberrant when it is associated with a decreased vestibular depth and an inadequate width of the attached gingiva [4].
The abnormal frenum are detected visually by applying tension over the frenum to see the movement of the papillary tip or the blanch which is produced due to ischaemia in the region. The frenum is characterized as pathogenic when it is unusually wide or when there is no apparent zone of the attached gingiva along the midline or the interdental papilla shifts when the frenum is extended [2]. In the 1st case, the presence of midline diastema with high fibrous labial frenal attachment was noted; a simple blanch test was performed and positive blanching of the papilla was observed.
The labial frenal attachments have been classified as mucosal, gingival, papillary and papilla penetrating, by Placek et al (1974) .
Ankyloglossia is an oral anomaly characterized by the abnormal insertion of the lingual frenulum, which compresses the mucosa, dense connective tissue, and, occasionally, superior fibers of the genioglossus muscle [5]. Based on the distance of the insertion of the lingual frenum to the tip of the tongue, Kotlow’s classification of ankyloglossia is as follows: [6]
The 2nd case presented a partial ankyloglossia and it was classified as class I according to Kotlow’s classification.
The problems associated with mechanical limitation of tongue are difficulties in breast feeding among neonates, malocclusion, gingival recession, improper oral hygiene and speech difficulties in pronunciation of consonants like t, d, n, and l, and difficult to roll a “r.” Therefore, management of ankyloglossia should be considered at any age depending on the patient’s history of speech, feeding, mechanical or social difficulties.
Treatment options include conventional surgical (scalpel) techniques (frenotomy, frenectomy, frenuloplasty) and lasers. Frenectomy is defined as complete excision, that is, removal of the whole frenulum
Laser transmits energy to the cells causing warming,welding, coagulation, protein denaturation, drying, vaporization and carbonization. The diode laser was introduced in dentistry and oral surgery in the mid-90s. The diode laser devices have specifications such as relatively small size, portable and lower cost that attract the dental practitioners and oral surgeons for use in various surgical indications in comparison to other laser equipment [8].
Diode lasers have several advantages when compared to conventional scalpel surgeries. They are compact and portable in design, with efficient and reliable benefits for use in soft tissue oral surgical procedure. Laser-assisted frenectomy is easy to perform with excellent precision, less discomfort, minimal or no bleeding due to sealing of capillaries by protein denaturation and stimulation of clotting factor VII production, shortened healing time with reduced postoperative bleeding and oedema [9]. Histologically, laser wounds have been found to contain significantly lower number of myofibroblasts resulting in less wound contraction and scarring, and ultimately improved healing, with better postoperative perception of pain and function than with the scalpel technique [10,11]. In the 2 cases, the bleeding was minimal and there was no need for sutures.
Furthermore, the association of the surgical procedure made with highpower laser and the application of low-power laser has its efficacy scientifically proved. Low-power laser has biomodulatory effects, acting directly in the cellular mitochondria, accelerating cellular metabolism and consequently generating benefits to individuals. Low-power laser used in adequate parameters assists on healing process and inhibits the appearance of pain or edema [12].
The disadvantages reported in researches on diode laser application were somehow similar to other lasers, like, delayed repair which is prominent in larger lesions and charring tissue in smaller lesions compared to the application of conventional scalpel surgical procedures. However, the control of the parameters to avoid the tissues heating allows avoiding these complications [14].
