Author(s): Moheb S Eskandaros, Ahmed A Darwish and Mohammed Fayek*
Laparoscopic sleeve gastrectomy (LSG) is a widely used procedure in treating morbid obesity. The LSG can lead to complications some of which can be fatal as leakage. Several strategies can be used to treat leakage after LSG as conservative management, endoscopic stenting, exploration and drainage with feeding jejunostomy or conversion to Roux en Y bypass with or without a proximal gastrectomy.
Laparoscopic sleeve gastrectomy (LSG) is a widely used procedure in treating morbid obesity. It is increasingly performed every day and the commonest procedure in our region [1]. The LSG, though very effective, can lead to complications, some of which can be fatal. Leakage is considered a major complication after primary LSG with a reported rate up to 7% [2,3]. Several strategies can be used to treat leakage after LSG. These strategies include conservative management, endoscopic stenting, exploration and drainage with feeding jejunostomy or conversion to Roux en Y bypass with or without a proximal gastrectomy [1].
In this study we tried to evaluate the use of double pig tail inserted by endoscope as a procedure of internal drainage in the management of leakage and fistula formation after laparoscopic sleeve gastrectomy in attempt for fistula healing without the need for surgical intervention.
This study was designed as a prospective case series clinical trial in which all patients suffering from leakage after laparoscopic sleeve gastrectomy in Ain Shams University Hospitals were included. The study took place from November 2016 till October 2020. An informed consent was obtained from the patients as approved by the Ethical Committee of the Faculty of Medicine, Ain Shams University, and the General Surgery Department.
• Leakage after primary sleeve gastrectomy
• Stable patient with no signs of sepsis
• No generalized peritonitis
• Good general condition
•Previous gastric surgery or redo
• Unstable patient
• Explored patients after leakage
• Signs of peritonitis
Patients suspected to have leakage from the drain if present or its site were subjected to full clinical examination, lab investigations and CT scan to detect the size and location of the leakage.
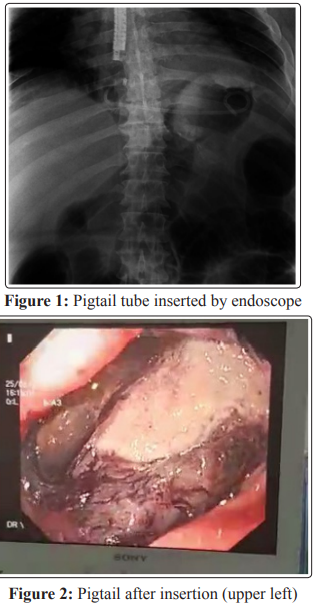
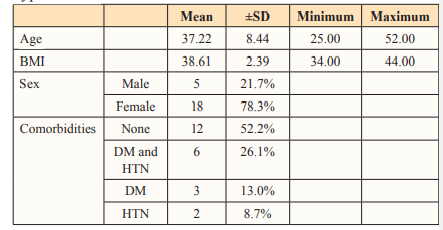
After ruling out of any other complications and after stabilization of the patients, they were subjected to upper endoscopy with double pig tail insertion (7 F) as shown in (Figure:1 and 2). This was accompanied with insertion of post-pyloric Ryle tube (18 F) in order to bypass the stomach, allow decompression and maintain enteral feeding.
The patients are placed under coverage of broad-spectrum antibiotics and IV fluids with enteral feeding started through the Ryle tube when feasible. Repeating the endoscope was performed as required for repositioning or replacement of blocked or migrated double pig tail tube. The patients underwent feeding jejunostomy if enteral feeding through Ryle tube was not adequate.
Follow up was done to the size of the leakage and the amounts of fluid discharge from the site of the fistula or drain if still present. Gastrograffin meal was done as required to detect the healing process and the residual leakage.
The study took place at Ain shams university hospitals from November 2016 till October 2020 where 436 primary sleeve gastrectomies were performed with 23 cases (5.27%) of leakage meeting the inclusion criteria.
The collected data was revised, coded, tabulated and introduced to a PC using Statistical package for Social Science (SPSS 20.0.1 for windows; SPSS Inc, Chicago, IL). Data was presented and suitable analysis was done according to the type of data obtained for each parameter. Mean and Standard deviation (± SD) and range for parametric numerical data, while frequency and percentage were used to describe of non-numerical data.
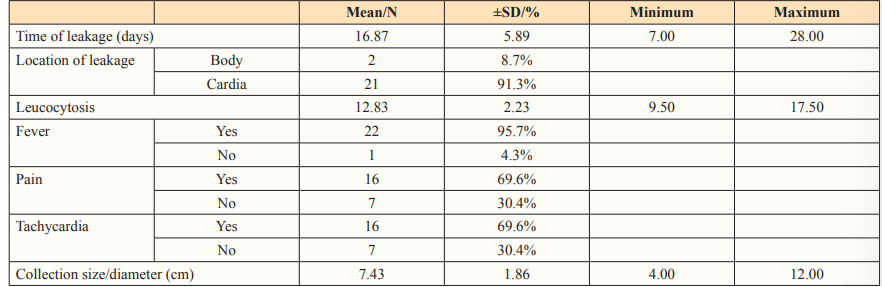
The mean, standard deviation and range of the age, sex, BMI and comorbidities of patients before the sleeve gastrectomy are shown in table 1.
Table 1: Age, sex, body mass index (BMI) and comorbidities distribution of the study group. DM: Diabetes mellitus, HTN: hypertension
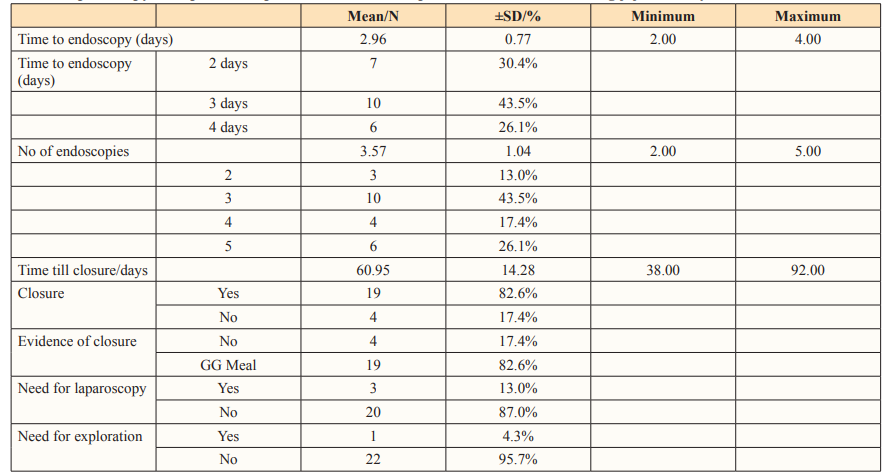
The mean time for presentation with leakage was 16.87±5.89 days ranging from one week to four weeks postoperative. All patients were subjected to computed tomography scan (CT scan) to show the site of leakage and the size of the collection present. The most common site for leakage was at the cardio-esophageal junction (91.3%) compared to the body of the stomach (8.7%). The maximum diameter of the collection intraabdominal ranged from 4-12 cm with a mean of 7.43± 1.86 cm with CT criteria. At the time of presentation, patients suffered from fever (95.7%), pain (69.6%) and tachycardia (69.6%). The leucocytic count ranged from 9.5-17.5 x 103 . These data are summarized in table 2.
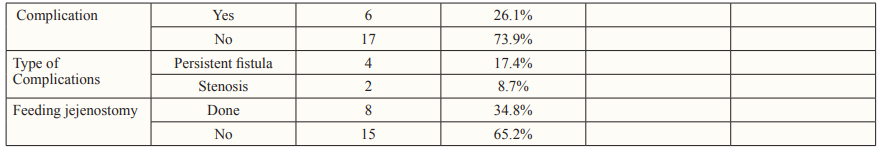
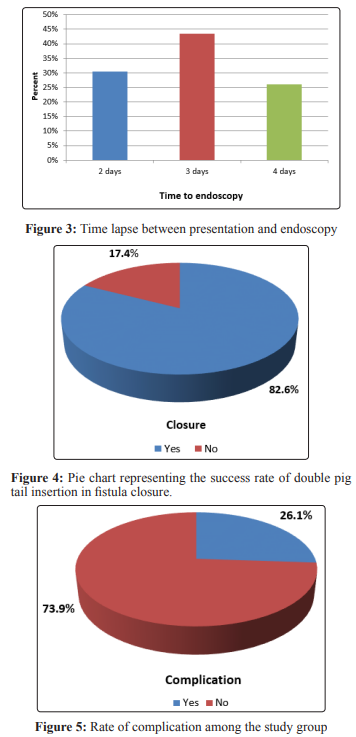
All 23 patients were subjected to upper GI endoscopy after resuscitation. The mean time for endoscopy was 2.96±0.77 days ranging from 2-4 days after presentation Figure: 3. The endoscopies were repeated as required every 10-14 days with a mean of 3.57±1.04 times and ranging from 2-5 endoscopies/patient. Closure was achieved in 19 patients out of 23 patients (82.6%) as evidenced by gastrograffin meal while 4 patients (17.4%) suffered from persistent fistulae. Time taken for closure was 60.95±14.28 days ranging from 38-92 days Figure:4. This was shown in table 3.
Four patients required surgical intervention due to failure of healing. Three patients underwent laparoscopy with lavage and drainage with insertion of feeding jejunostomy. One patient underwent exploration due to development of early sepsis at day 17 with peritoneal lavage, drainage and feeding jejunostomy.
Four other patients required feeding jejunostomy along the course of the management at day 38,40, 43 and 51 due to inadequacy of total parenteral nutrition and Ryle tube for maintaining of goon nutritional status and positive nitrogen balance till leakage closure.
As regard the complications, four patients had persistent fistulae who were managed as described. Two other patients had stenosis at the midbody after closure of the fistula due to excessive fibrosis. They were later subjected to endoscopic stenting to bypass the obstruction Figure:5.
The laparoscopic sleeve gastrectomy (LSG) became a wide spread operation in the management of morbid obesity. The increase in the number of patients and the number of operations had led to a rising learning curve with decreasing complications [2,4] However, the most distressing complication was and still the staple line leakage especially at the cardia. Many maneuvers were used to control this complication as re-exploration and stenting.
A new approach was adopted to try an internal drainage using a double pig tail tube inserted by endoscope as a method for closure of the leakage without the need to subject these fragile patients for another operation and more morbidities.
Along the course of this research, 436 patients underwent sleeve gastrectomies at Ain shams university hospitals from November 2016 till October 2020 with 23 reported cases of postoperative leakage that met the criteria of the study at a rate of 5.27% of total cases.
The mean time for presentation with leakage was 16.87 days ranging from one week to four weeks postoperative. All patients were subjected to computed tomography scan (CT scan) to show the site of leakage and the size of the collection present. The most common site for leakage was at the cardio-esophageal junction (91.3%) compared to the body of the stomach (8.7%). The maximum diameter of the collection intraabdominal ranged from 4-12 cm with a mean of 7.43± 1.86 cm with CT criteria. In a study done by Benosman et al. the mean size was 6.8±3.7 cm [5]. At the time of presentation, patients suffered from fever (95.7%), pain (69.6%) and tachycardia (69.6%). The leucocytic count ranged from 9.5-17.5 x 103 .
All 23 patients were subjected to upper GI endoscopy after resuscitation. The mean time for endoscopy was 2.96±0.77 days ranging from 2-4 days after presentation. In a study done by Benosman et al. the mean time was 27.4 ±22 days with a delayed time between diagnosis and intervention [5]. In a monocentric prospective study reported in 2011, Bège et al. observed a higher fistula healing rate when endoscopic treatment was started early (within 3 weeks) [6].
The endoscopies were repeated as required every 10-14 days with a mean of 3.57±1.04 times and ranging from 2-5 endoscopies/ patient.
Closure was achieved in 19 patients out of 23 patients (82.6%) as evidenced by gastrograffin meal while 4 patients (17.4%) suffered from persistent fistulae. Time taken for closure was 60.95±14.28 days ranging from 38-92 days. In a study done by Benosman et al. demonstrated that endoscopic treatment of fistula after bariatric surgery is efficient, with an efficacy rate of 88.4% [5]. These results are in agreement with the literature, which shows a fistula healing rate ranging from 73 to 100%. Another study, reported by Donatelli the advantage of the inner-drainage strategy was highlighted [3]. Focusing on a trans-fistula, double-pigtail, guided drainage, these authors showed, in two recent studies, healing rates of 74.6 and 97%, respectively, among 67 patients with fistula after LSG. These data add to those of Bouchard et al. who reported a 78.8% efficacy of trans-fistula drainage after bariatric surgery leakage in a group of 33 patients with similar results to this study [7].
Four patients required surgical intervention due to failure of healing, three underwent laparoscopy with lavage and drainage with insertion of feeding jejunostomy. One patient underwent exploration due to development of early sepsis at day 17 with peritoneal lavage, drainage and feeding jejunostomy. Four other patients required feeding jejunostomy along the course of the management at day 38,40, 43 and 51 due to inadequacy of total parenteral nutrition and Ryle tube for maintaining of goon nutritional status and positive nitrogen balance till leakage closure.
As regard the complications, four patients had persistent fistulae who were managed as described. In a study by Dammaro et al showed that the fistula healing becomes more difficult with delay to endoscopic intervention with better results the earlier the intervention [8]. Two other patients had stenosis at the midbody after closure of the fistula due to excessive fibrosis. They were later subjected to endoscopic stenting to bypass the obstruction.
We have also shown the major impact of the delay between the fistula diagnosis and first therapeutic endoscopy. When this delay was less than 3 weeks, a higher chance of healing or a faster recovery has been observed in the majority of published studies. Also, the attitude to internalization of drainage of collection has the same efficacy with avoidance of the morbidities of surgical intervention associated with enteral feeding through tube or feeding jejunostomy has shown to yield satisfactory results in fistula healing
The endoscopic internal drainage using double pig tail is a feasible method for the management of stable post sleeve gastrectomy leakage with localized collection. It yields satisfactory results especially if early intervention is initiated before a chronic fistula is developed. This is coupled by enteral feeding either by Ryle or feeding jejunostomy to ensure good nutritional status. Further studies with bigger scale are required for better judgement.
