Author(s): Tyler G Chin, Alyxandra M Soloway, MD, Joseph Colombo*, PhD, DNM, OHS and Stephen Soloway, MD, FACP, FACR, CCD
Glutamic Acid Decarboxylase 65-kilodalton isoform (GAD-65) is associated with cocaine induced limbic encephalopathy mimicking GAD-65 limbic
encephalopathy in humans. A 20-year-old white female presented with a clinical picture of a limbic encephalopathy and a positive ANA. She has a
hypermobility disorder with dysautonomia with POTS. Her workup revealed a GAD-65 antibody greater than 250 nmol/L, a normal lumbar puncture,
and a normal brain MRI. Her GAD-65 associated limbic encephalopathy was treated with IVIG 2 g per kilogram per month. She received three treatments with no improvement. Due to arthralgias, a soft tissue rheumatic pain, she was referred to pain management. The patient admitted to using cocaine. Her IVIG was discontinued. A repeat test for GAD-65 antibody remained elevated.
After a stint in drug rehabilitation and cessation of cocaine her symptoms of limbic encephalopathy abated and GAD-65 normalized. This is the 1st case report of GAD-65 antibody mimicking cocaine induced limbic encephalopathy. While GAD65 related autoimmune neuropathies are rare, one must consider cocaine toxicity as a mimic of both autoimmunity and immune neuropathies, including the spectrum of GAD-65-related disorders.
Glutamic Acid Decarboxylase 65-kilodalton isoform (GAD-65) antibody is a biomarker of autoimmune central nervous system (CNS) disorders and, more commonly, non-neurological autoimmune diseases [1]. GAD-65 is associated with cocaine induced limbic encephalopathy mimicking GAD-65 limbic encephalopathy in humans. An example of limbic encephalopathy is shown in Figure 1 [2]. It’s been shown in Male Syrian hamsters (Mesocricetus auratus) that use of cocaine is associated with changes in GAD-65. Hamsters treated with low-dose (0.5 mg/kg/day) cocaine throughout adolescence compared to the control group of the hamsters treated with saline reflected significant differences in the area covered by GAD65 puncta in several notable aggression regions, including the anterior hypothalamus, the medial and central amygdaloid nuclei, and the lateral septum [3].
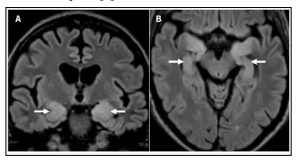
Figure 1: Brain magnetic resonance imaging in autoimmune limbic encephalitis. On coronal fluid-attenuated inversion recovery (FLAIR) image, bilateral T2-hyperintensity of the medial temporal lobes is seen (A, arrows). (B) Bilateral T2-hyperintensity of the medial temporal lobes is also shown on an axial FLAIR image (arrows) [2].
Stiff man syndrome, Type 1 diabetes, autoimmune thyroid disease, and pernicious anemia are the most frequent GAD-65 autoimmune associations [4]. Other less frequent associations are cerebellar ataxia, epilepsy, opsoclonus-myoclonus ataxia, and Miller Fisher syndrome. One or more of these disorders coexists in approximately 70% of patients with GAD- 65 neurological autoimmunity [1]. While the exact cause of encephalitis is often unknown, cocaine is known to induce neuroinflammation, central nervous system vasculitis, impede metabolic substrate delivery via vasoconstriction, and directly interfere with cell physiology [5,6]. Microglial cells, astrocytes, and pericytes are activated by cocaineinduced impairment of autophagy leading to neuroinflammation [7,8,9]. Autophagy protects cells from the endoplasmic reticulum stress caused by misfolded proteins and other defective products of biosynthesis [8,9]. Limbic encephalitis is a form of encephalitis, a disease characterized by inflammation of the brain. Limbic encephalitis is often caused by autoimmunity [10] which may be incited by severe or chronic inflammation. This is a case study of a healthy 20-year-old female with hypermobility and cocaine abuse with symptoms of limbic encephalopathy with a positive antinuclear antibodies (ANA).
A 20-year-old white female, first menstrual cycle age 9, presented with a clinical picture of a seizure and progressive short-term memory loss. Limbic encephalopathy was diagnosed, and a positive ANA 1-40 homogeneous. She has a hypermobility disorder. The patient specifically denied family history of any neurologic disorder, type 1 diabetes, thyroid disease. The patient graduated high school with good grades and participated on the cheerleading squad. She had no known medical problems. She specifically denied chest pain, shortness of breath, muscle weakness, hearing loss, double vision, vision loss, and visual disturbances. She specifically denied abdominal pain, bloating, diarrhea, muscle weakness, dysphagia, and color changes in the hands or feet. Her CBC revealed a white count of 6000, hemoglobin of 13.4 g, and platelet count of 242,000. Sodium, potassium, chloride, and CO2, were normal her BUN was 15 and Creatinine 0.5, her GFR was 120. Her AST and ALT were 14 and 12, respectively. Her CPK was normal her D-dimer was normal. A GAD-65 antibody greater than 250 nmol/L, a normal lumbar puncture, and brain MRI showed hyperintensity in the temporal lobes bilateral with no hippocampal involvement. Urine drug screen was positive for cocaine. Negative for benzodiazepines, barbiturates, and other illicit substances. Serologies negative including double- stranded DNA, ENA panel, SSA, SSB, NMO, CCP, protein electrophoresis, negative anti- neuronal antibody, and negative phospholipid antibodies. ESR was 24, with normal is less than 20, and CRP was 18, with normal less than 8.0, The patient admitted to daily cocaine use by nasal inhalation and never smoking it.
She was evaluated and treated by neurocardiology who confirmed dysautonomia with POTS. For the dysautonomia, she was prescribed Midodrine (2.5 mg tid) and Propranolol (10mg qd). Her GAD-65 associated limbic encephalopathy was treated with IVIG 2 g per kilogram per month. She received three treatments with improvement in memory loss to a minor degree and no further seizures were noted. IVIG was discontinued. She continued treatment for dysautonomia. A repeat test for GAD-65 antibody remained elevated. After a stint in drug rehabilitation and cessation of cocaine her symptoms of limbic encephalopathy abated and GAD- 65 normalized.
Review of the literature by PubMed and Medline failed to show a case of cocaine induced GAD-65 limbic encephalopathy, hence this is the first case report of GAD-65 antibody mimicking cocaine induced limbic encephalopathy. While GAD-65 related autoimmune neuropathies are rare, one must consider cocaine toxicity as a mimic of both autoimmunity and immune neuropathies, including the spectrum of GAD-65-related disorders. Cocaine toxicity is seen in many autoimmune/rheumatologic conditions including cutaneous vasculitis, midline granuloma, cerebral vasculitis, coronary aneurysms and myositis.
Conflicts of Interest: None
Funding: None
