Author(s): Liana Monica DEAC Babes
Hand hygiene has been identified as the treating intervention strategy that will drive down cross-transmission of pathogens in the healthcare environment. Educational programs need to be developed to address the issue of poor hand hygiene. Many studies from CDC and another healthcare organizations have shown that the bacteria’s who cause hospital infections are most frequently spread from one patient to another on hands of healthcare workers. The World Health Organization (WHO) has developed an evidence-based measure of hand hygiene called the five moments of hand hygiene, which refer to washing hands before touching a patient, before performing an aseptic or clean procedure, after potentials exposure to body fluids, after touching a patient, and after touching the patient surroundings. Also the WHO has recommended guidelines for hand hygiene (wash hands with soap and water when it is visibly dirty or soiled with blood or other body fluids or after toilet use and it is recommend even washing with water and soap or an alcohol-based hand rub) Just a little [1]. History elements here, for comp rounding names and done situations. The word Hygiene is derived from the name Hygeia, who was the Greek goddess of healing. In modern usage hygiene usually refers to cleanliness and especially to any practice which leads to the absence or reduction of harmful infectious agents. In 1546, physician Girolamo Fracas Toro came up with the revolutionary idea that infection could be passed on, not only directly from person to person, but also via hands and surfaces such as clothes and the hands and so it was create the germ theory - identifying microorganisms as the cause of many diseases. In the 1800s studies by Ignaz Semmelweis in Vienna and Oliver Wendell Holmes in Boston, established that hospital-acquired diseases were transmitted via the hands of Hand care workers (HCWs). By the mid-1980s, hand washing was a central focus of CDC guidelines, on prevention of healthcare associated infections -HCAI. Handwashing with water and soap was the recommended method, with healthcare workers instructed to undertake vigorous rubbing together of all surfaces of lathered hands for at least 10 seconds, followed by thorough rinsing under a stream of water. It was the start for the first national hand hygiene guidelines. In 1995 and 1996, the CDC/Healthcare Infection Control Practices Advisory Committee (HICPAC) recommended that either antimicrobial soap or a waterless antiseptic agent can be used for cleansing hands upon leaving the rooms of patients with multidrug-resistant pathogens. In 2000 Pittet, introduced an alcohol-based hand rub for the reduction of HCAI. On same year, it appeared the First Global Patient Safety Challenge developed by the WHO Hand Hygiene Improvement Strategy (9). In 2002 it was defined, alcohol-based handrubbing for hand hygiene practices in health-care settings. After a pilot testing during 2007-2008 it was performed a strategy for Hand hygiene, as one of the most effective and basic measures to prevent the spread of infection in hospitals. Systematic published literature, indicate that effective hand decontamination can significantly reduce the rate of HCAI. Hand hygiene data, make a good understanding, about how vital it is, for maintaining health to patients and in their clinical entourage.
Healthcare-acquired infections (simple HAIs): are also known as nosocomial infections, are infections that patients get while receiving treatment for medical or surgical conditions [2]. HAIs occur in all settings of care, including hospitals, surgical centers, ambulatory clinics, and long-term care facilities such as nursing homes and rehabilitation facilities [4]. It is important to determine.
Who is on risk? -All hospitalized patients are susceptible to contracting a nosocomial infection. Some patients are at greater risk than others-young children, the elderly, and persons with compromised immune systems are more likely to get an infection.- Other risk factors are long hospital stays, the use of indwelling catheters, failure of healthcare workers to wash their hands, and overuse of antibiotics.
Estimation In: American hospitals alone, CDC estimates that HAIs account for 1.7 million infections and 99,000 associated deaths each year. Most of these infections are: 32% percent of all healthcare acquired infection are urinary tract infections; 22% are surgical site infections; 15% are pneumonia (lung infections); 14% are bloodstream infections.
recommendations for cleaning hands include: Healthcare providers cleaning their hands with soap and water, or an alcohol-based hand rub before and after caring for every patient; catheters being used only when necessary and removed as soon as possible; cleaning the skin where the catheter is being inserted or the surgical site, and providers wearing hair covers, masks, gowns and gloves when appropriate. The hands as vectors of microorganisms certainly. Healthcare workers may contaminate their hands by contact with a patient’s inanimate environment and the level of contamination depends on the duration and nature of the activity, though it is not known how many organisms are required for transmission or which activities are most likely to result in transmission. Health-care-associated pathogens can be recovered not only from infected or draining wounds, but also from frequently colonized areas of normal, intact patient skin. The perineal or inguinal areas are usually most heavily colonized, but the axillae, trunk, and upper extremities (including the hands) also are frequently well colonized too. The number of organisms differ and almost are: S.aureus, Proteus mirabilis, Klebsiella spp., and Acinetobacter spp. present on intact areas of the skin of certain patients. HCWs can contaminate their hands with gram-negative bacilli, Escherichia Coli Enterococci, or Clostridium difficile; Nosocomial pathogens can be recovered from: body fluids or infected areas of skin in patients, but also from intact skin of hospitalized patients. The level of contamination depends on the duration and nature of the activity in medical units, though it is not known how many organisms are required for transmission or which activities are most likely to result in transmission.
transmission of microorganisms via the hands of healthcare workers: The 2009 World Health Guidelines for Hand Hygiene for Healthcare Settings identifies five ways the nosocomial transmission of pathogens from one patient to another via a healthcare worker’s hands can occur. Microorganisms must be present on the patient’s skin or have to be shed into the patient’s environment such as nearby inanimate objects; .Microorganisms must be transferred to the hands of the healthcare worker; The microorganisms that have contaminated the worker’s hands must be able to survive on their hands. .The healthcare worker must either omit hand hygiene or inadequately perform it. The healthcare worker’s contaminated hands must come into direct contact with either another patient, or with an inanimate object that will come into contact with a patient, such as a shared portable vital signs monitor.
Performance Indicators: The following performance indicators are recommended for measuring improvements in HCWs’ handhygiene adherence: Periodically monitor and record adherence as the number of hand-hygiene episodes performed by personnel/number of hand-hygiene opportunities, by ward or by service. Provide feedback to personnel regarding their performance; Monitor the volume of alcoholbased hand rub (or detergent used for handwashing or hand antisepsis) used per 1,000 patient-days; Monitor adherence to policies dealing with wearing of artificial nails When outbreaks of infection occur, assess the adequacy of health-care worker hand hygiene [5]. According to the latest guidelines from the WHO, HCW should practice proper hand hygiene: before touching the patient, after touching the patient, after touching inanimate objects in the patient’s surroundings, after exposure to bodily fluids and before clean/aseptic procedures. Hand hygiene has been identified to drive down cross-transmission of pathogens in the healthcare environment [10]. Healthcare providers should encourage not only the patient, but also their family members and visitors, to regularly practice hand hygiene frequently when indicated to minimize contamination and potential transmission. More Educational programs need to be developed to address the issue of poor hand hygiene in population [11]. It has been postulated that if adequate hand hygiene protocols are strictly followed by healthcare personnel and it could lead to a significant 15-30% reduction in hospital acquired infection [6].
Availability of hand hygiene agents: Hand hygiene products are available in a wide variety of forms to meet the specific clinical needs of the healthcare environment. Most products currently available to healthcare workers in hospitals are alcohol-based as alcohol has significant activity against a wide variety of bacteria and viruses [7]. Typical agents include plain (non-antimicrobial) soap, alcohols, chlorhexidine, chloroxylenol, hexachlorophene, iodine and iodophors, quaternary ammonium compounds or triclosan [3]. The Food and Drug Administration classifies healthcare antiseptic drug products into three unique categories: a. Surgical hand scrubs - an antiseptic containing preparation that substantially reduces the number of microorganisms on intact skin.; b. Antiseptic hand washes - antiseptics containing preparation designed for frequent use, reducing the number of microorganisms on intact skin to an initial baseline level after adequate washing, rinsing, and drying; Patient preoperative skin preparations - fast-acting, broad-spectrum and persistent antiseptics containing preparation that reduce the number of microorganisms. Hand hygiene agents must be carefully selected in order to ensure compliance, efficacy and safety for both the healthcare worker and patient. Several factors must be taken into consideration: Cost of the agent; Ease of use for healthcare workers; Potential for dermal irritation and skin reactions; Efficacy of the agent. Product availability and accessibility within the healthcare facility; Drying time necessary after applying the agent; Staff support for the selected product. In addition, adjuncts to prevent contact dermatitis such as hospital grade lotions must be considered to ensure a low risk for adverse events [8]
techniques for hand hygiene: Soap and water is still considered the gold standard for hand hygiene. When using soap and water, it is important to wet the hands first. Then apply 3 to 5 mL of soap to the hands, avoiding bar soap. Next rub the hands together for a minimum of 15 seconds covering all surfaces of the hands and fingers. Finally rinse the hands off with water, dry thoroughly with a paper towel and use the paper towel to turn off the faucet. When soap and water is not available, alcohol-based hand rubs (wipes, gels, or foams) should be applied.
When using an alcohol-based product: Healthcare workers must completely follow the manufacturer’s label to ensure that the desired efficacy is reached [12]. Advantages of Cleaning Hands with AlcoholBased Hand Rubs: tooked less time to use; made more accessible than sinks; caused less skin irritation and dryness; ere more effective in reducing the number of bacteria on hands; making alcohol-based hand rubs improved hand hygiene practices in our clinical study. Alcoholbased agents may be used in the following cases: When hands are not visibly soiled or contaminated with blood or body fluids; Before direct contact with patients; After direct contact with a patient’s skin; After contact with bodily fluids or excretions, mucous membranes, broken skin or wound dressings; When moving from a contaminated to a clean body site; After contact with an inanimate environment (equipment or furniture near patient); After removing gloves; Emergency situations where sinks are not available and hands are visibly soiled. When using agents containing alcohol, such as wipes, the entire surface of the hand must be covered by the product and allowed to dry prior to donning gloves. Sanitizing hand lotionshave become increasingly popular. Alcohol-based hand sanitizers kill most types of bacteria, viruses and fungi in a few seconds. To be effective, alcohol-based hand sanitizers must contain at least 60 percent alcohol. In fact, alcohol-based hand sanitizers are tremendously effective in preventing the spread of the seasonal flu, H1N1, Simple. Resp. infection and other viral- and bacterial-based diseases. Also, the alcohol evaporates quickly after killing the first layer or so of germs on your skin. This means that, although benevolent bacteria are killed, enough remain on lower levels or elsewhere up the arm to re-colonize. Fast evaporation, coupled with moisturizers, also means this won’t dry out your skin.
WHO recommanded Hand Washing technic and Manners For HcW: Using warm or lukewarm running water, wet your hands and apply soap-antibacterial is not required to have clean hands; Rub your hands together to make a lather; Rub your palms together and intertwine your fingers to make sure you get between them; Don’t forget the back of your hands. For a proper hand washing, this step should take no less than 20 seconds; Rinse your hands well; Dry your hands well. See Fig. 1.
cDc Hand Hygiene Guidelines for HcW: Make cleaning your hands faster, more convenient and easier on your hands; increase adherence of healthcare workers to recommended hand hygiene procedures; reduce the spread of microorganisms in healthcare settings. See Fig. 2 and 3 for a better understanding, as even for a conclusion fact.
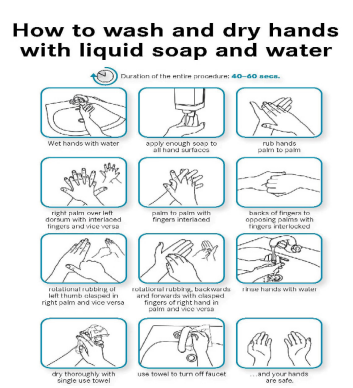
Fig 1. WHO Recommanded Hand Washing Technic For HCW?

Fig. 2. Postulate attitudes.

Fig. 3. Postulate attitudes.
1. The hands of HCWs, are the most common carrier of transmission
of microorganisms from one patient to another, from one area of the
patient’s body to another and from a polluted environment to patients.
2. Hand washing should become an educational priority in all
world hospitals.
3. Proper hand hygiene is the single most important, simplest, and
least expensive, which means of reducing the prevalence of NI and the
spread of antimicrobial resistance.
4. Healthcare-associated infections lead to added suffering,
morbidity, mortality, and financial burden to patients and society.
5. Hand hygiene (HH) is an important element in ordinary
precautions and is the most effective measure for preventing infections,
almost NI in our clinics.
1. World Alliance for Patient Safety. The Global Patient Safety Challenge 2005-2006
Clean Care is Safer Care”. Geneva, World Health Organization, 2005.
2. Vincent JL (2003) Nosocomial infections in adult intensive-care units. Lancet
361:2068-2077.
3. Stone PW, Braccia D, Larson E (2005) Systematic review of economic analyses of
health care-associated infections. American Journal of Infection Control 33:501-509.
4. Rosenthal VD (2008)International Nosocomial Infection Control Consortium report,
data summary for 2002-2007, issued January 2008. American Journal of Infection
Control 36:627-637.
5. Pittet D (2006) Evidence-based model for hand transmission during patient care and the
role of improved practices. Lancet Infectious Diseases 6:641-652.
6. Sanderson PJ, Weissler S (1992) Recovery of coliforms from the hands of nurses and
patients: activities leading to contamination. Journal of Hospital Infection 21:85-93.
7. 7 Ojajarvi J (1980) Effectiveness of hand washing and disinfection methods in removing
transient bacteria after patient nursing. Journal of Hygiene (London) 85:193-203.
8. Luby SP (2005) Effect of handwashing on child health: A randomized controlled trial.
Lancet 366:225-233.
9. Pittet D (2000) Effectiveness of a hospital-wide programme to improve compliance
with hand hygiene. Lancet 356:1307-1312.
10. Gopal Rao G (2002) Marketing hand hygiene in hospitals--a case study. Journal of
Hospital Infection 50:42-47.
11. Rosenthal VD (2003) Effect of education and performance feedback on handwashing:
the benefit of administrative support in Argentinean hospitals. American Journal of
Infection Control 31: 85-92.
12. Hugonnet S, Perneger TV, Pittet D (2002) Alcohol-based handrub improves
compliance with hand hygiene in intensive care units. Archives of Internal Medicine,
162:1037-1043.
