Author(s): Agnis Saulitis*, Rihards Lulens, Egils Pukitis and Julija Dolgopolova
ABSTRACT
Objectives: To describe a rare complication of hydroxyapatite (HA) crystal deposition disease (HADD) – spinal canal stenosis. To discuss clinical features and surgical management of this entity.
Background: HADD is a crystal-induced arthropathy caused by para-articular and/or intra-articular deposition of HA crystals. Etiology is uncertain, predisposing factors include microtrauma, local ischemia, end-stage renal disease. Commonly, glenohumeral joint is affected, less often - elbow, wrist, hand, hip, knee, ankle, foot and spine. Rarely – deposition of crystals is associated with spinal canal stenosis.
Methods: We report a case of 34-year-old male who was admitted to the hospital with recurrent fever and elevated inflammatory markers for the past few months. Patient had a history of stage 5 chronic kidney disease treated with hemodialysis, anabolic-androgenic steroid use, arterial hypertension, tertiary hyperparathyroidism and multiple calcium deposits along glenohumeral, iliofemoral joints bilaterally, left foot and lumbar spine. Computed-tomography showed hyperdense calcifications in soft tissue along lumbar spine with minimal intraspinal involvement. Over the course of a few weeks’ symptoms worsened, the patient presented with lower back pain radiating in both legs, progressive lower paraparesis, walking difficulties. Magnetic-resonance imaging showed hypointense periarticular lesions with fluid levels on both T1 and T2-weighted images from L1 to L3 extending intraspinally with severe spinal canal stenosis, medullary cone compression. Surgical resection of the pathological tissue was indicated.
Results: The patient underwent L1-L3 laminectomy and resection of the lumbar soft tissue and intraspinal extradural calcified depositions. Histopathological examination confirmed diagnosis of HADD associated spinal canal stenosis. Physical rehabilitation followed, progressive recovery was seen, with almost complete resolution of motor deficits 6 months post-surgery.
Conclusions: HADD, affecting lumbar spine, can lead to inflammation, swelling and stenosis of the spinal canal resulting in severe back pain and progressive neurological deficits. Surgical treatment in such cases can be curative and lead to good outcomes.
Hydroxyapatite (HA) crystal deposition disease (HADD) is a crystal-induced arthropathy caused by para-articular and/or intra-articular deposition of HA crystals. Etiology is uncertain, predisposing factors include microtrauma, local ischemia, endstage renal disease. Commonly, glenohumeral joint is affected, less often - elbow, wrist, hand, hip, knee, ankle, foot and spine. Rarely - deposition of crystals is associated with spinal canal stenosis. Our objectives was to describe a rare complication of HADD- spinal canal stenosis and discuss clinical features and surgical management of this entity [1, 2].
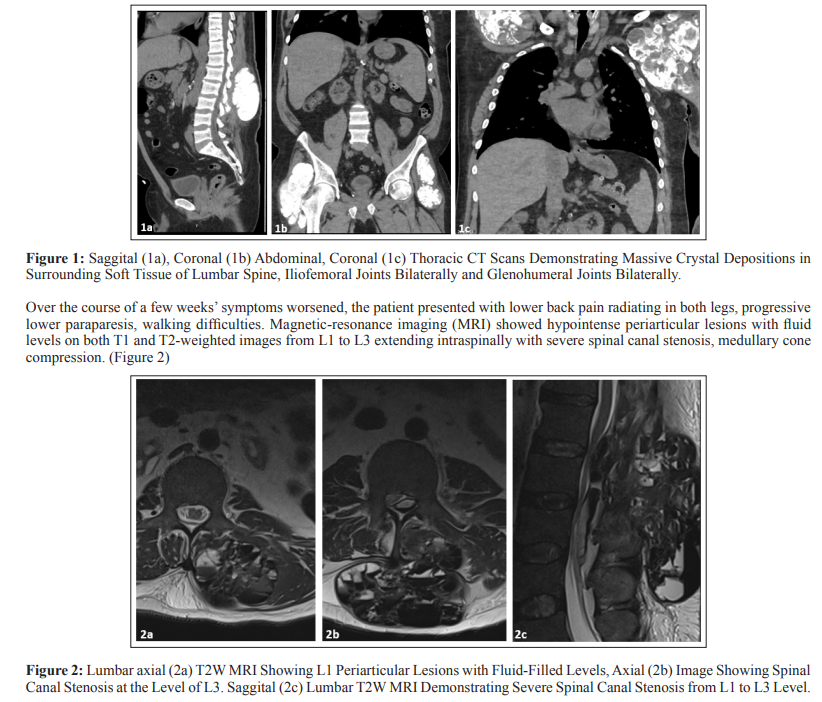
We report a case of 34-year-old male who was admitted to the hospital with recurrent fever and elevated inflammatory markers for the past few months. Patient had a history of stage 5 chronic kidney disease treated with hemodialysis, anabolic-androgenic steroid use, arterial hypertension, tertiary hyperparathyroidism and multiple calcium deposits along glenohumeral, iliofemoral joints bilaterally, left foot and lumbar spine. Computed-tomography (CT) showed hyperdense calcifications in soft tissue along lumbar spine with minimal intraspinal involvement. (Figure 1)
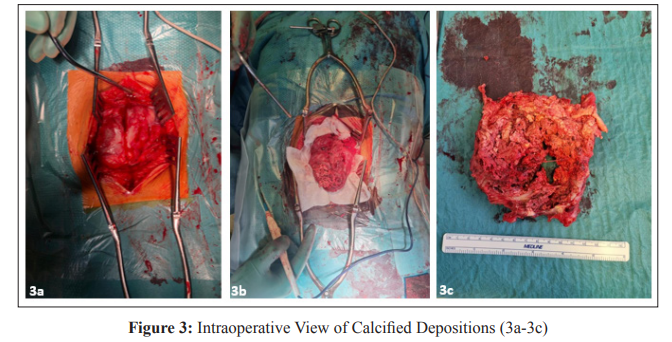
Surgical resection of the pathological tissue was indicated. The patient underwent L1-L3 laminectomy and resection of the lumbar soft tissue and intraspinal extradural calcified depositions. (Figure 3)
Histopathological Examination Confirmed Diagnosis of HADD Associated Spinal Canal Stenosis. Physical Rehabilitation Followed, Progressive Recovery was Seen, With Almost Complete Resolution of Motor Deficits 6 Months Post Surgery.
The presented case highlights a rare complication of HADD - spinal canal stenosis. This condition predominantly affects the glenohumeral joint, and less commonly the elbow, wrist, hand, hip, knee, ankle, foot, and spine - in rare instances leading to spinal canal stenosis, as observed in our case [1]. Patient’s presentation with recurrent fever, elevated inflammatory markers points out the systemic impact of HADD. HADD’s association with conditions such as chronic kidney disease and anabolic-androgenic steroid use suggests potential predisposing factors in this case [2-5].
Imaging played a crucial role in diagnostics, assesing the severity of the spinal involvement. CT revelaed hyperdense calcifications along the lumbar spine, wile magnetic resonance imaging provided detailed insights into the extent of the pathology. The identification of hypointense periarticular lesions with fluid levels on both T1 and T2-weighted images, along with severe spinal canal stenosis and medullary cone compression, guided the decision for the intervention [6-8].
The surgical approach involved L1-L3 laminectomy and resection of the lumbar soft tissue and intraspinal extradural calcified depositions. Histopathological examination confirmed the diagnosis of HADD-associated spinal canal stenosis. The postoperative course demonstrated progressive recovery, with almost complete resolution of motor deficits six months postsurgery. This positive outcome emphasizes the importance of timely surgical management in cases of HADD-related spinal canal stenosis to prevent irreversible neurological damage.
In conclusion, this case report sheds light on the rare but serious complication of spinal canal stenosis associated with HADD. Clinicians should be vigilant in patients with HADD, particularly those with predisposing factors, to identify and manage potential complications promptly. The successful surgical intervention in this case underscores the therapeutic potential of timely and targeted approaches in mitigating the impact of HADD on spinal structures.
