Author(s): Ruchi Shrestha
Introduction: Intraocular foreign body is a kind of ocular emergency. Longer the foreign body stays in the eye, the greater damage they make. Here we report a case of intraocular foreign body which was treated as a case of intermediate uveitis for one and half years with oral and topical steroids.
Case Report: A 24 years-old patient came with complains of blurring of vison in left eye since one and half years associated with flashes and floaters since 1 week. There was no history of trauma. The patient was treated as a case of recurrent intermediate uveitis. The anterior chamber was quiet and there were 2+ vitreous cells. Diagnosis of intraocular foreign body was made after careful examination of fundus by indirect ophthalmoscopy. It was confirmed by Brightness scan and Computed Tomography. The case improved after removal of intraocular foreign body by pars plana vitrectomy.
Conclusion: This case report highlights that intraocular foreign body may masquerade silently as uveitis for years. The diagnosis may mislead in the absence of history of trauma and X-Ray orbit. Intraocular foreign body may remain silently inside the eye for years without causing serious complications. The most sensitive tool to diagnose intraocular foreign body is Computed Tomography scan.
Intraocular foreign body (IOFB), a kind of ophthalmic emergency, accounts for about 6 % of the ocular trauma and is commonly seen in young male [1]. The foreign bodies not only cause mechanical damage but also bring pathogenic microorganisms into the eyes, leading to endophthalmitis, which seriously affects the prognosis of visual acuity. Longer the foreign bodies stay in the eyes, the greater damage they make. Therefore early diagnosis and treatment of intraocular foreign body is important [2].
A 24 -years- old male came with complains of blurring of vison in left eye since one and half years associated with flashes and floaters since 1 week. The patient was mechanic by profession and had no history of trauma in eye. The patient was treated as a case of recurrent intermediate uveitis for one and half years with oral and topical steroids but the symptoms did not improve. The Best Corrected Visual Acuity at presentation was 6/6 in right eye and 6/24 in left eye. His Intraocular pressure was 20mmHg in right eye and 16 mmHg in left eye. On ocular examination there was linear corneal scar temporally and defect/hole was present in iris on the same side (Figure 1).
Figure 1: Arrows showing Corneal scar and iris hole
The anterior chamber was quiet. There were 2+ vitreous cells. On indirect ophthalmoscopy small metallic shiny foreign body was seen on the infero-temporal retina along with RPE changes near ora serrata in left eye (Figure 2). X-Ray orbit did not show the presence of foreign body in the eye.
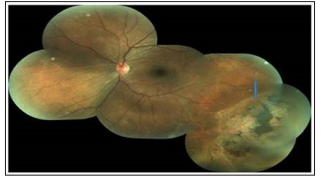
Figure 2: Poster segment photo showing site of intracular foreign body in the infero-temporal area as indicated by arrow
Brightness-scan (Figure 3) and computed Tomography- scan (Figure 4) confirmed the diagnosis of intraocular foreign body
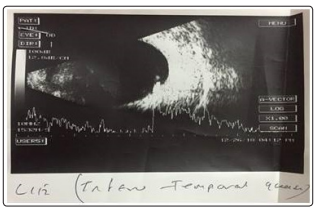
Figure 3: Brightness scan showing high spike at inferior and temporal indicating foreigh body

Figure 4: Computed Tomography scan of orbit showing the intraoclar foreign body as indicated arrow
The patient underwent pars plana vitrectomy, intraocular foreign body removal, endolaser and silicon oil insertion in left eye. (Figure 5) shows the intraocular foreign body which was removed after intraocular foreign body removal. The best corrected visual acuity in left eye after silicon oil removal was 6/12.
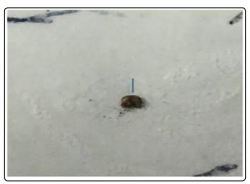
Figure 5: Intraocular foreign body removed by pars plana vitrectomy
Ocular injuries with retained IOFB possess serious threat to vision due to mechanical damage to intraocular structures, introduction of infection and chemical reaction of foreign body [3]. Plain films are frequently false negative or inaccurately localize the IOFBs in up to 30% of eyes. Computed Tomography and ultrasonography are now the primary methods to determine IOFB presence/localization and the nature of associated intraocular injuries. MRI is another powerful diagnostic tool but the method is controversial. The sensitivity of CT for IOFBs >0.06 mm is 100% [4]. The intraocular foreign body was missed in our case when X-ray orbit was done. Intraocular foreign body in our case was confirmed by computed tomography of head and orbit.
Intraocular foreign body should be removed urgently. Timing of surgery is determined primarily by the threat of endophthalmitis, which occurs in up to 48% of eyes with intraocular foreign body injury [4]. Pars plana vitrectomy is the preferred technique for removal of intraocular foreign body. Factors that determine the visual outcome include the nature and location of foreign body, the interval between the injury and surgery, initial visual acuity, entrance of wound location, preoperative retinal detachment, presence of intraocular hemorrhage, presence of endophthalmitis and the type of surgery [5].
Removing retained IOFBs within the first 24 hours after the injury may reduce the risks of infectious endophthalmitis, proliferative vitreoretinopathy and siderosis bulbi [6]. The process of siderosis bulbi may take few weeks to years before clinical signs are manifested depending on the site and nature of foreign body [7]. Our patient was lucky enough to have his intraocular foreign body removal without developing the complications for about one and half years.
This case report highlights that intraocular foreign body may masquerade silently as uveitis for years. The diagnosis may mislead in the absence of history of trauma and by X-ray orbit. Intraocular foreign body may remain silently inside the eye for years without causing serious complications. The most sensitive tool to diagnose intraocular foreign body is Computed Tomography scan.
Ethical approval was given by the local ethical committee board of Mechi Eye Hospital. Written informed consent was obtained from the patient.
Funding: None
Acknowledgements: Mechi Eye Hospital, Birtamod, Jhapa, Nepal
