Author(s): Douimi L*, Touaiher W, Oukessou Y, Rouadi S, Abada R, Roubal M and Mahtar M
Fungal rhinosinusitis is a rare entity, which can affect both healthy and immunocompromised individuals. It encompasses a wide spectrum of immune and pathological responses, including chronic, granulomatous, allergic and invasive forms. This last can extend to invasion of the orbit and the brain. We report the case of a young girl known to be asthmatic operated successfully in our department for an invasive fungal sinusitis
Fungal sinusitis is the mucosal inflammation of paranasal sinuses due to fungus etiology, with aspergillus being the commonest causative organism[1]. In fact, mycotic infection of paranasal sinuses by aspergillus was first described by mackenzie in 1893. Although its diagnosis has advanced markedly with the availability of computed tomography and sinus endoscopy, this entity remains underdiagnosed earlier because of the wide range of its clinical symptomatology [2,3,4].
We present the case of an 18 years old patient, asthmatic, operated in our department for fungal expansive pansinusitis and we also reviewed similar cases published in the literature to assist other healthcare professionals in recognizing and managing this condition.
This work has been reported in accordance with the scare criteria.
An 18 year old female patient presented to ent emergency department for a protrusion of the right eye evolving since 3 months, associated with a hypertelorism on a chronic sypmtomatology encompassing bilateral nasal obstruction, anosmia. No other sign was find in the interrogation, in particular, no epistaxis episod, nor visual disturbances. She denies sinus discharge and any prior episode of rhinosinusitis. Her past medical history found asthma poorly controlled. No history of diabetes, hypertension, or tuberculosis or anterior surgery was noted.
On clinical examination, vitals were within normal limits, and temperature was normal. Nasal examination on direct rhinoscopy, found an inflammatory and congested mucosa obstructing the nasal space totally. In the inspection, right proptosis was present, with no oculomotor dysfunction nor, loss of visual acuity. General examination and family history were non contributory. All the biochemical parameters were within normal limits.
The patient underwent a cerebral-orbital ct which shows an aggressive heterogeneous pansinus process occupying all the sinuses of the face, with bone destruction of the sinus walls and protrusion of the two globes more marked on the right. There is associated with an erosion of the posterior wall of the frontal sinus and the riddled blade of the ethmoid on the right with invasion of the dura mater in the right frontal. The rest of the cerebral parenchyma was homogeneous without abnormal hypo or hyperdensity.
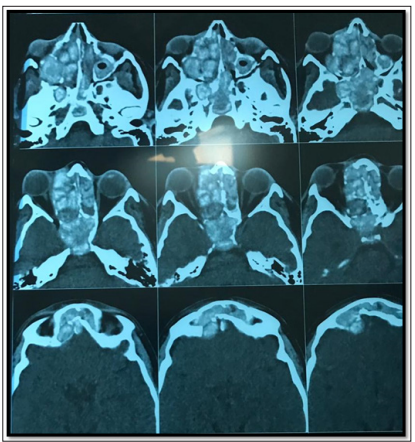
Figure 1: CT Scan Images: Axial Cut Showing the Erosion of the Posterior wall of the Frontal Sinus as well as an Enormous Process Invading the Medial Wall of the Right Orbit which is ProtrudeInvestigation was completed with a ct paranasal sinus objectifying total filling of sinus and nasal cavities with hyperdense material with right frontal parenchymal extension and rupture of the bone walls. In the right ethmoidal cells, this material pushes back the ipsilateral eyeball and the medial rectus muscle with grade ii exophtlamia. This aspect may be related to aspergillosis, however another origin cannot be ruled out.
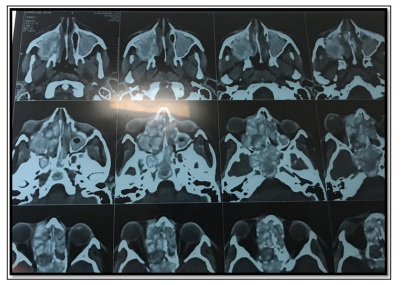
Figure 2: CT Paranasal Sinus Showing Total Filling Sinuses and its Extension
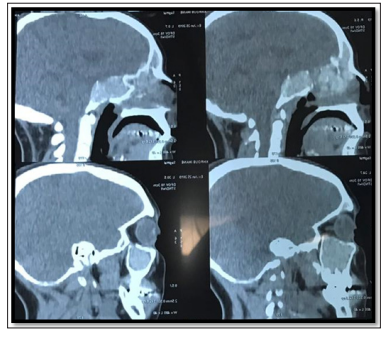
Figure 3: Sagittal CT Scan Cuts Showing the Filling of Sphenoid Sinus and the Thinning of Its Walls, as Well as The Erosion of the Posterior Wall of the Frontal Sinus
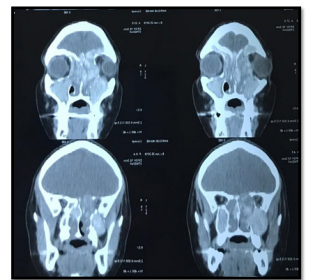
Figure 4: coronal cuts pointing the extension of the process Sinuses and cerebral mri was undergone showing the same thing above mentioned. It also showed a dural meningeal contrast enhancement opposite the right frontal hemi sinus, with no visible cerebral parenchymal extension sign.
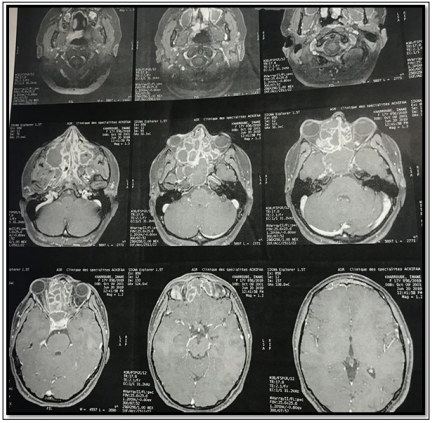
Figure 5: MRI Images Showing the Extension of the Disease
Under general anesthesia, and after a medical preparation based on general corticosteroid therapy, local nasal corticosteroid therapy, as well as nasal washing; the patient underwent an endoscopic surgery. The intervention consisted on a bilateral meatotomy, ethmoidectomy and sphenoidotomy procedures so as to remove the obstacle and restore the drainage of nasal cavity and paranasal sinuses. The surgery was completed by a medical prescription of amphotericin b. Histological examination confirmed the diagnosis of fungal sinusitis.No complications were recorded in the postoperative period. The patient was discharged 3 days after the surgery. 24 months follow up showed a complete remission and a satisfying clinical course.
Sinus fungal disease is becoming one of the most important diseases of the nasal cavity because of raising prevalence[5]. In fact, fungal sinusitis severity ranges from non-invasive (fungal ball, allergic fungal sinusitis) to invasive acute or chronic fungal infections[6]. This last classically affects healthy individuals, unlike acute invasive fungal sinusitis which arises in immunocompromised hosts[7].
Diagnosis is usually delayed, because of the absence of an apparent predisposing factor, a concealed symptomatology, as well as the lack of specific symptoms[8]. The prognosis of the invasive forms is poor due to its aggressiveness to invade the surrounding structures, particularly intracranial and orbital tissues, and in some cases dissemination to systemic organs[9]. If neglected and kept untreated, it may cause a proptosis, ocular disorders which can go to blindness, neurological complication as well as altered mental status. Aspergillus and mucor fungal are believed to be the common organisms causing fungal sinusitis [10].
Diagnosis of fungal sinusitis has advanced markedly with the availability of computed tomography scan (ct), magnetic resonanceimaging (mri) and sinus endoscopy. These imaging tools allow physicians to assess the extension of lesions, as well as to evaluate the patient’s response after treatment [6].
Ct scan evaluation is required before surgery, so as to study the anatomical and pathological extension of the disease. The anatomical assessment is necessary for an appropriate functional endoscopic surgery. Ct scan displays an excellent imaging tool. It commonly reveals sinus filling, mucosal thickening, and peri maxillary fat blurring due to a direct fungal tissue infiltration or vascular congestion[8]. Indeed, the evidence of bone destruction; which suggests a potentially invasive process; is a late finding and can be absent despite the extension of the lesion beyond the paranasal sinuses[11].
In this case, mri is a useful tool in evaluating the early changes in major vessels including the carotid artery and cavernous sinus as well as evaluating intracranial and orbital extension[12,13]. Differentiation between a malignant neoplasm and chronic invasive fungal rhinosinusitis by radiologic tools is difficult to impossible. The ultimate distinction between both of them is best made histologically. The latter allows a definitive diagnosis relying on positive fungal culture and histopathology, which is usually performed during nasal endoscopy or debridement surgery [14].
There is no general agreement about the treatment[15]. In fact, the revolution of functional endoscopic sinus surgery (fess) has totally changed the guidelines of surgical management. Therefore, the treatment of choice has become extensive surgical radical debridement of all necrotic tissues in which the fungi thrive, as early as possible combined with prompt intensive antifungal therapy [8]. Two commonly used drugs are itraconazole and amphotericin b [14].
The exact measure of debridement required depends on the extent of the disease spread and the condition of the patient. Thus, the ultimate aim of surgery is to restore normal nasal and paranasal drainage [16].
To sum up, the rising incidence of aspergillosis as a cause of fungal rhinosinusitis calls for a high degree of suspicion, especially in asthmatic hosts. Fungal sinusitis, particularly in its chronic invasive form, often progresses gradually over weeks or even months. In fact, diagnosis is usually delayed and made in advanced forms when complications are already set up.
Thus, early diagnosis and management improve clinical outcomes and are keys of a good prognosis. Surgery is considered to be the mainstream treatment based on complete excision of infected paranasal tissues. The treatment plan might differ and is tailored according to the severity, the extension and patient’s medical condition. Henceforward, an adequate attention must be paid to this entity of rhinosinusitis in order to avoid complications [17].
