Author(s): Pablo Santillán Roldan*,Mauricio Gómez Bossa,Andrés Cepeda Mora, Pablo Armas Cruz, Lorena Guacales Zambrano, Alejandra Castillo Mantilla ,Geraldine Paredes Guerrero,Thalía Cazar Gallegos, Felipe Loza Hernández and karla Andrade Ruiz
Maternal Sepsis remains as one of the most common causes of morbidity and mortality between obstetric patients with the 11% of maternal deaths worldwide. It also contributes, to the increased risk of other common causes of maternal death such as hypertensive disorders, hemorrhage, and thromboembolism. Despite of the recent advances in preventative strategies, diagnostic tools, antimicrobial therapy and laboratory tests, morbidity and mortality in pregnant population continued to increase over the years .
Maternal Sepsis remains as one of the most common causes of morbidity and mortality between obstetric patients with the 11% of maternal deaths worldwide. It also contributes, to the increased risk of other common causes of maternal death such as hypertensive disorders, hemorrhage, and thromboembolism. Despite of the recent advances in preventative strategies, diagnostic tools, antimicrobial therapy and laboratory tests, morbidity and mortality in pregnant population continued to increase over the years [1]. Due to these worrying facts, effective prevention, early recognition and appropriate management has become so important nowadays. The international definition of sepsis was changed in 2016 by the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) Committee defined sepsis as a life-threatening organ dysfunction caused by a deregulated host response to infection secondary to inadequate perfusion [2]. Attending the physiopathology of sepsis we propose the mnemonics LAVOE initial management with Liquids (fluids therapy), Antibiotics, Vasopressors, Oxygen and Enoxaparin (thromboprophylaxis) as an easy form to remember what to do with a patient on suspect of sepsis.
To understand the mechanics of fluid resuscitation, we must understand that venous volume can be divided into unstressed and stressed volume. The unstressed volume is the basal amount of blood, this volume does not affect intravascular pressure. Stressed volume is then referring to the volume that actively affects the venous pressure and the vascular wall stress and, consequently, the venous return. Therefore, early resuscitation in sepsis is recovering the unstressed volume lost by vasodilation and loss of the endothelial glycocalyx[3]. The following step in resuscitation consists of filling up the stressed volume affecting cardiac output. Filling the stressed volume is the key moment in resuscitation because an under-load would affect tissue perfusion by an insufficient cardiac output and an overload would cause a fluid leak and general edema [3-5].
The Surviving Sepsis Campaign (SSC) and The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock agree on the administration of 30ml/kg as an initial measure on any patient diagnosed of sepsis [4,6]. However the SSC recommends that the 30ml/kg should be administered within a “1 hour bundle” but the Japanese Guide keeps recommending an administration on a 3 hour range. This disagreement has become relevant over the last few years because of the surging literature criticizing the fluid overload that can be induced if the fluid therapy is too aggressive and the “one-size-fits-all” measure that contradicts the current biomedical practices that suggest a more personalized practice [7]. In fact, it has been demonstrated in a retrospective study involving 185 hospitals in the New York State Department of Health that the time to completion of the fluid bolus was not associated with in-hospital mortality [8].
Fluid overload has become very important because it has been demonstrated that it can be even more harmful than under-load [5,7,9]. Indeed, the iatrogenic edema causes organ dysfunction in various systems such as the cardiac, vascular, renal, Central Nervous System, Respiratory, Gastrointestinal and hepatic system (FIGURE 1) [7].
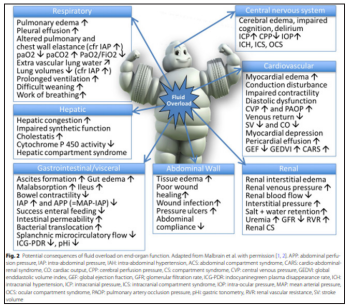
Figure 1: (9) Describe how the various systems are affected with edema caused by the use in excess of liquids.
Hopefully, several studies found that a fluid-restrictive therapy is possible and won’t affect the patient outcome [5,10]. In 2018 the REFRESH clinical trial compared a fluid-restrictive therapy where they only administered a single 1000mL bolus and vasopressors to the trial group and a liberal group where they could continue administering as much liquids as the attending clinician would consider plus the vasopressor therapy. As proposed, the restricted group had no damage and allowed a 30% reduction in total fluid administration in 24h [10]. Yet, the mechanism is not clear. It is suspected to be because restrictive fluid resuscitation keeps the tissue in a low-pressure condition, therefore avoiding the harmful edema [5].
In addition, current guidelines recommend the use of balanced crystalloids against the use of normal saline (un-buffered crystalloid solution) or colloids [4,6]. Buffered solutions slightly vary in their composition but typically have a pH, chloride concentration, and overall osmolality closer to human plasma than that of saline solutions [3]. The recommendation against the use of saline for resuscitation in sepsis is a discussed issue that seems to have finally come to a conclusion. In 2015, the SPLIT trial compared 0.9% Saline versus Plasma-Lyte 148 (PL-148) (a buffered crystalloid) on a heterogeneous population of ICU patients. Even though saline was associated with hyperchloremia and metabolic acidosis, there was no difference in the outcome. In 2017, the SALT pilot trial compared between 0.9 Saline and balanced crystalloids (Lactated Ringer’s solution or Plasma Lyte A) and, again, found no difference in the outcomes. They only acknowledged that patients exposed to larger volumes of saline appeared to experience more major adverse kidney events [11]. The main issue with both of these studies is that they included a heterogeneous population and not only sepsis patients. Finally, the SMART trial published in 2019 compared the two solutions on 1641 patients admitted to the ICU diagnosed with sepsis. This trial demonstrated that balanced solutions were associated with reduced 30-day hospital mortality, major kidney events, and increased ventilation, vasopressor and RRT-free days [12]. The proposed mechanism by which balanced crystalloids may result in better outcomes than saline is not completely understood but it is suspected to be because of the hyperchloremia and acidosis caused by Saline, causing vasoconstriction and inflammation of renal vasculature [11].
There are three important categories of colloids available: albumin, hydroxyethyl starch (HES), and gelatin. These substances should act as oncotically active fluids that should counter the capillary leak and increase the inward flux of fluids towards the vasculature. Still, in sepsis conditions, the loss of the endothelial glycocalyx layer should allow molecules that are oncotically active to equilibrate themselves between physiological spaces [3]. Nonetheless, we should not generalize between colloids. Also, Albumin is recommended only in patients that have already received an important volume of crystalloids and it is not recommended to use it as a standard initial treatment[4,6]. Accordingly, ALBIOS, the largest trial to the date studying the use of albumin in septic patients, reported a decreased mortality only in the subgroup of septic shock patients with hypoalbuminemia [13]. Contrarily, the use of HES is strongly contraindicated [4,6].
Finally, to avoid under or over-resuscitation, major guidelines recommend close motorization of the patient. Rivers et al. suggested in 2001 that monitoring macro vascular and static measures as insufficient to predict if a patient is still fluid responsive (under-resuscitated, balanced or over-resuscitated) and suggested motorization with dynamic measures to guide resuscitation In fact, now a days, the current guidelines recommend measuring central venous pressure, mean arterial pressure, and oxygen delivery (that could be defined by central venous oxygen saturation, hemoglobin, cardiac output, and oxygen consumption) significantly reduces mortality associated with sepsis [2,4]. Finally a dynamic test that can be easily done is the passive leg raising test which consists on lifting the patient’s legs to 45° while the rest of the body is horizontal to evaluate if the increased venous return towards the right heart affects cardiac output: if it is responsive, then the patient is still fluid responsive [4,6,9].
The Society for Maternal-Fetal Medicine gave an approach on the management of sepsis in pregnant or puerperal patients [14]. The recommendations from the SCC are preserved but they comment that passive leg raising may not be useful in patients carrying a third trimester pregnancy because the uterus may compress the inferior vena cava and venous blood from the lower limb would not actually return to the cardiac cavities. In these cases, it is recommended to administer a small bolus of fluid (250-500mL) to evaluate any changes in cardiac output [14].
Pregnant women by themselves have greater susceptibility to develop serious infections, this fragility is based on a multifactorial origin, both by the physiological and anatomical changes proper of pregnancy and by chronic diseases that the patients may carry, invasive procedures to which the pregnant woman may be subjected and some other risks related to the healthcare system [12,15].
Risk factors that can trigger sepsis during pregnancy include: social-economical, medical, as well as the changes inherent in pregnancy
Poverty, difficult access to health homes or poor infrastructure, scarcity of medicines, limited personnel for care, lack of basic services such as water, electricity and telephone in homes [12,15].
Age over 40 years, anemia, diabetes, chronic hypertension, obesity, diseases with HIV (human immunodeficiency virus), untreated tuberculosis, inflammatory pelvic disease, in vitro fertilization, amniocentesis [12,15].
Prolonged labor, more than 5 vaginal touches during labor, vaginal delivery instrumented, not using antibiotics during cesarean section [12,15].
The administration of antibiotics is decisive in the management of sepsis in the obstetric patient, the late onset increases the risk of mortality by 7.6% with each hour of delay [16].
The study conducted by Ferrer and Liu indicate a proportional increase in mortality due to the delay of each hour from the onset of antibiotic- therapy and that it should begin as soon as possible after microbiology samples [17,18].
The study was developed by Peltan. Included 10811 patients in which the mean time from patient arrival to administration of antimicrobial therapy was 116 minutes. Thus mortality per year was higher when the time door-antibiotic were > 3 h vs ≤ 3 h (OR 1.27; 95% CI, 1.13-1.43) but was not found in those whose interval was > 1 h vs ≤ 1 h (adjusted OR, 1.26; 95% CI, 0.98-1.62).
The pathogens can be gram positive, gram negative and fungal, the agents that stand out are Escherichia coli, Streptococcus, Staphylococcus, streptococcus type A, although its frequency is low; can trigger shock by the production of toxins and necrosis having mortality from 30 to 60%. (19)(4,20,21)(Fan S-R et al.,2020; Suleiman et al., 2016; Evans et al., 2021)
Pathogens such as candida can develop chorioamnionitis, miscarriage, premature birth, and stillbirth. Rare microorganisms reported in maternal sepsis include Clostridium innocuum, Clostridium novyi, Plasmodium vivax, and Chlamydia psittacosis. Table 1 shows microorganisms isolated from maternal microbiology in sepsis during pregnancy and puerperium.
| Gram positive | Gram negative |
|---|---|
| Streptococcus grupo A, B. 24.0% Staphylococcus aureus. 14.3% Enterococcus 3.1% Listeria monocytógenes 2.9% Otros grampositivos: 3.2% |
Escherichia coli 31.4% Clostridium 3.3% Klebsiella 2.7% Acinetobacter 2.0% Enterobacter 1.6% Bacteroides 1.6% Proteus mirabilis 1.5% Pseudomonas 1.0% Otros gramnegativos: 3.8% |
| Anaerobics : 1.9% Non bacterias: 1.8% |
Take from New Concept and Management for Sepsis in Pregnancy and the Puerperium Modified by: the authors.
Diagnoses associated with sepsis may be associated with pregnancy or during pregnancy-related surgical procedures or those not related to pregnancy, but if they are more often in the obstetric population, incidental infections during pregnancy, or those acquired in the intensive care unit It is recommended to use antimicrobial combination therapy, and not mono therapy considering the clinical characteristics of the patient, place of infection and microbial prevalence [4,12,19]. During pregnancy the infections are usually poly microbial, under this concept they are administered: penicillin, an aminoglycoside and clindamycin, vancomycin or piperacillin-tazobactam. Considering the risk some may have to the fetus. as well as antibiotic withdrawal depending on the germ identified and considering procalcitonin values [4,20,22,23].
| Patogen | Agent | Tratamiento | Alternatives |
|---|---|---|---|
| Corioamnionitis | Cándida Clostridium innocuum, Clostridium novyi, Plasmodium vivax y Chlamydia psittacosis | Ampicilina más gentamicina más cobertura anaeróbica con clindamicina o metronidazol en caso de parto por cesárea | |
| Endomiometritis | Gram-negative anaerobes Streptococci | Ampicilina, gentamicina y metronidazol o clindamicina | cefotaxima o ceftriaxona más metronidazol |
| Infecciones del tracto urinario | Gramnegatives Occasionally caused by staphylococci and streptococci | Gentamicina con ampicilina | carbapenem o piperacilinatazobactam |
| Cesárea | MSSA MRSA Streptococci | Flucloxacillin* + clindamycin *If MRSA use vancomycin instead of flucloxacillin | Vancomycin + clindamycin Clindamycin/ teicoplanin are alternatives in MRSA |
| Shock tóxico | Staphylococci Streptococci | Flucloxacillin* + clindamycin + gentamicin (gentamicin once only) *For MRSA use vancomycin instead of flucloxacillin | Vancomycin + clindamycin + gentamicin (gentamicin immediately and once only) OR Linezolid + gentamicin (gentamicin once only) |
| Abdominal infections | MRSA Streptococci Gramnegatives Anaerobes | Ceftriaxone, cefotaxime, ceftazidime, or cefepime plus metronidazole; | Complicated cases may require monotherapy with a carbapenem or piperacillintazobactam |
Modified: by authors.
The optimal duration of antibiotics remains controversial and few prospective randomized controlled trials have been interpreted. The survival campaign against sepsis guidelines suggests 7 to 10 days. (4,22,24) (Evans et al., 2021; Cordioli et al., 2013;Greer et al.,2020)
Among the biomarkers that we can use to monitor the response to sepsis treatment are those that are not specific such as white blood cells, reactive protein C, whose sensitivity and specificity are low. Procalcitonin currently plays a leading and promising role in patients with sepsis, as well as serum lactate which > 4 mmol/L is associated in approximately 46% with mortality. (Evans et al., 2021; Bartoletti et al., 2018; Iankova et al., 2018; Schuetz et al., 2017).
The pregnant woman experiences hemodynamic changes in order to adapt to the increased metabolic needs for the correct development of the fetus [25,26]. The increase in cardiac output and peripheral vasodilation determine a physiologic hyperdynamic state along with loss of afterload. In addition, there is also hypoalbuminemia and loss of intravascular oncotic pressure[27].
Sepsis increases cardiac output and decreases systemic vascular resistances by the release of pro-inflammatory cytokines and also generates extravasation of albumin and fluid Thus, sepsis in obstetrics led to a state of relative hypovolemia resulting from pathological redistribution of the absolute intravascular volume that leads to hypotension because of vasodilation and third spacing and myocardial dysfunction [27,28,29]. Approximately, 60% of septic patients develop systolic dysfunction with an ejection fraction below 45% [14].
For those obstetric patients who are not fluid responsive or who are not candidates for further fluid resuscitation, vasopressors should be started to improve blood pressure [14,27].
Septic shock was described as sepsis with persistent hypotension needing vasopressors to maintain a mean arterial pressure (MAP) ≥ 65 mmHg, and a serum lactate level >2 mmol/L (18 mg/dL)”. Simonetto. C, et al., 2020. This means a severe hemodynamic failure which remains a major challenge associated with high rates of hospital mortality [9].
The main objective in the management of patients with septic shock is to increase macro and microcirculatory flow. (Scheeren, Et al., 2019) As hypotension is also induced by systemic vasodilation, vasopressor therapy is fundamental in septic shock, aiming at correcting the vascular tone depression and then at improving organ perfusion pressure [30].
The Sepsis Surviving Campaign (SSC) recommends applying vasopressors within the first hour when fluid administration is not sufficient to achieve the hemodynamic resuscitation goals: a target Mean Arterial Pressure (MAP) of 65 mmHg (strong recommendation, moderate-quality evidence). Or to normalize lactate in patients with high lactate concentrations as a marker for tissue hypoperfusion (weak recommendation, low-quality evidence) [4,9].
SOMANZ guidelines suggest despite fluid resuscitation (1-2 L), the mean arterial pressure and other indices do not improve, vasopressors may be required [31].
All vasoactive drugs will affect placental blood flow and therefore should be used when the benefits to the mother outweigh any risks to the fetus.
Vasopressors in maternal sepsis are aligned with SSC recommendations. The SSC and SOMANZ guidelines recommend Norepinephrine as the initial vasopressor of choice [4,14,30,31].
As a strong α-adrenergic agonist, it increases blood pressure primarily through being able to increase vascular tone with a little effect on heart rate. Thus, an early administration can increase cardiac output through an increase in cardiac preload, but also by increasing contractility [32]. If hypotension persists despite hydric resuscitation and norepinephrine administration, vasopressin or epinephrine may be used as second line agents [33].
Vasopressin should be used with caution in pregnant women. Theoretically, the drug may stimulate oxytocin receptors in the uterus, resulting in contractions and possibly preterm birth [14,33].
Instead of that SSC suggests adding vasopressin instead of escalating the dose of norepinephrine for adults with septic shock on norepinephrine with inadequate MAP levels [4].
For adults with septic shock and inadequate MAP levels despite norepinephrine and vasopressin, SSC suggests adding epinephrine [4].
| Agents | Receptors | Major effects | Major side-effects | SSC | Safety |
|---|---|---|---|---|---|
| Norepinephrine | α1, β1 | - venous and arterial tone | Cardiac arrhythmia Peripheral ischemia | First line agent | Safe for the fetus, especially at low doses. |
| - preload, - contractility | Inadvertent immunomodulation | ||||
| Epinephrine | α1, β1, β2 | - contractility, - preload | Tachycardia, tachyarrhythmia Peripheral ischemia Splanchnic ischemia | Second line agent | when initial norepinephrine administration fails to maintain an adequate MAP |
| - venous and arterial tone | Increased myocardial oxygen consumption lactic acidosis, hyperglycemia | ||||
| - heart rate | |||||
| Dopamine | α1, β1 | - contractility, - heart rate | Tachycardia, tachyarrhythmia | Only in the setting of myocardial dysfunction or continued hypoperfusion despite fluid and vasopressor therapy | Not recommended for renal protection |
| D1, D2 | - venous and arterial tone | ||||
| - renal and mesenteric vasodilation | |||||
| Vasopressin | V1a V2 | - venous and arterial tone, platelet aggregation | Peripheral ischemia Mesenteric ischemia Cardiac arrhythmia | Second line agent | theoretical interaction of vasopressin with oxytocin receptors |
| V1b | - water retention, release of coagulation factors | when initial norepinephrine administration fails to maintain an adequate MAP | |||
| - corticotropic axis stimulation, insulin secretion | |||||
| Terlipressin | V1a,b > V2 | - venous and arterial tone, platelet aggregation | Peripheral ischemia Mesenteric ischemia Cardiac arrhythmia | Against using in septic shock | |
| - water retention, release of coagulation factors | |||||
| Modified from: Shi R, Hamzaoui O, De Vita N, Monnet X, Teboul J-L. Vasopressors in septic shock: which, when, and how much? Ann Transl Med. 2020;8(12):794-794 | |||||
There is a direct relationship between the development of multiorgan dysfunction syndrome (MOMS) and mortality. Sepsis is characterized by a marked hypovolemia due to an increase in capillary permeability, thus, a redistribution of blood flow is generated with the following disturbance in the relationship between disponibility and demand of oxygen. That is the reason to supply oxygen to guarantee maternal arterial PaO2 at more than 70 mm Hg and partial pressure of carbon dioxide (PaCO2) at less than 60 to 70 mm Hg to ensure fetal oxygenation and placental perfusion [1].
Sepsis includes deregulation triggered by excessive stimulation of the clotting cascade. The cellular surfaces already turned into pro coagulants are responsible for complex formation, resulting in disseminated intravascular coagulation and vascular microthrombosis [19,27,34].
Pregnancy and sepsis are associated with hypercoagulability state therefore prevention of deep vein thrombosis is essential, therefore measures are focused towards the use of intermittent pneumatic compression stockings and low molecular weight heparin, which by its mechanism of action displaces the antithrombin III of the cellular surfaces, where the signals of the clotting phase begin to be elaborated in order to avoid the formation of the complexes [3].
The use of unfractionated heparin and low molecular weight heparin is recommended [22].
Among the mechanisms in which heparin modulates the response to sepsis are:
Interferes with leukocyte adhesion to endothelium, a key in the development of sepsis.
showed a 40% reduction in mortality with the use of prophylactic heparin[35,36]. However, reported a 12% relative risk reduction in mortality in patients receiving intravenous heparin within 28 days of sepsis treatment[37].
Septic pregnant woman should have thromboprophylactic treatment based on unfractionated heparin(NFH) or low molecular weight heparin (LWH), if the delivery occurs before the first 12 hours it will be done with HNF and in those where it is foreseen after 12 hours with LWH, the dose of heparin will depend on the weight of the patient and the conditions in which it is found as well as its renal function. Table 4 indicates weight-adjusted doses for multidisciplinary treatment of sepsis [4,37,38].
| Weight | Enoxaparin | Dalteparina | Tinzaparina |
| <50 kg | 20 mg | 2500 U/dia | 3500 U/dia |
| 50 a 90 kg | 40 mg | 5000 U/dia | 4500 u/dia |
| 91 a 130 kg | 60 mg | 7500 U/dia | 7000 U/dia |
| 131- 170 kg | 80 mg | 10000 U/dia | 9000 U/dia |
| >170 kg | 0.6 mg/kg/day | 75 U/dia | 75 U/dia |
Taken from Taken from Venous thromboembolism in pregnancydiagnosis, management, and treatment Modified by the authors
| Therapeutic | |||
|---|---|---|---|
| Weight | Enoxaparin | Dalteparin | Tinzaparin |
| <50 kg | 60 mg QD O 40 mg twiceday | 5000 IU twice a day or 10000 IU daily. | 175 UI/kg |
| 50 a 69 kg | 90 mg QD 60 mg twice day | 6000 IU twice a day or 12000 IU daily. | 175 UI/kgonce daily |
| 70- 89kg | 80 mg twice a day or 120 mg daily. | 8000 IU twice a day or 16000 IU daily. | 175 UI/kg once daily |
| 90- 109kg | 150 mg QD O 100 mg twice day | 10000 IUtwice a day or 20000 IUdaily. | 175 UI/kg |
| 110 a 125 kg | 120mg twice day or 180 mg daily | 12000 IUtwice day or 24000 IU daily | 175 UI/kg |
| >125 kg | Consult with a Specialist. |
Taken from Venous thromboembolism in pregnancy-diagnosis, management, and treatment Modified by the authors
