Author(s): Maikal Kujur
Hernia repair has been one of the most common and an ever-evolving field of surgery. With experienced surgeons, laparoscopic hernia repair techniques are associated with significantly less postoperative pain and an earlier return to normal work compared with open hernia repair. The use of a mesh in primary inguinal hernia repair is a standard treatment now and has been proven to be far superior to a basic anatomical repair.
Hernia repair has been one of the most common and an everevolving field of surgery. With experienced surgeons, laparoscopic hernia repair techniques are associated with significantly less postoperative pain and an earlier return to normal work compared with open hernia repair [1-4]. The use of a mesh in primary inguinal hernia repair is a standard treatment now and has been proven to be far superior to a basic anatomical repair [5].
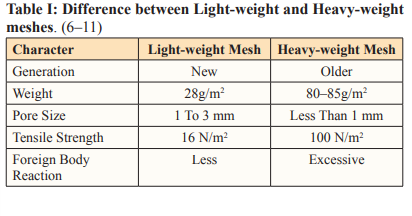
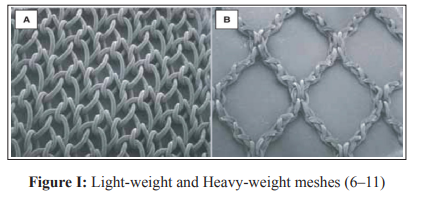
As mesh-related complications have increased in the last decade, there has been an evolution in the type of meshes being used. As a consequence, today two major mesh concepts are distinguished, the classical concept including so-called heavyweight meshes with small pores and the new concept including lightweight meshes with large pores. Typically, the new generation mesh is characterised by a reduced weight (depending on the specific weight of the basic polymer), a pore size of more than 1 mm, an elasticity of 20-35% (at 16 N/cm) and a physiologic tensile strength of 16 N/cm at minimum. Heavy-weight meshes contain high concentrations of foreign material and cause excessive inflammatory responses. Light-weight meshes have larger pores and they encourage collagen production with the integration of the mesh into the abdominal wall with an adequate inflammatory response [6-10]
Several studies have been conducted to compare the use of Light-weight meshes and Heavy-weight meshes in both open and laparoscopic inguinal hernia repair [1-13].
To compare the heavy-weight vs light-weight meshes in laparoscopic inguinal hernia repair by assessing the postoperative outcomes and patient satisfaction by analysing: Infection, Seroma formation, Ileus, Foreign Body Sensation, Groin Stiffness, Delayed Urinary Retention, Testicular Atrophy among male patients, Early postoperative pain on Day 1, 2 & 7, Chronic pain on follow-up 3rd and 6th month, Duration of hospital stay, Duration to start work, Quality of life after surgery (7 points Likert scale) and Recurrence.
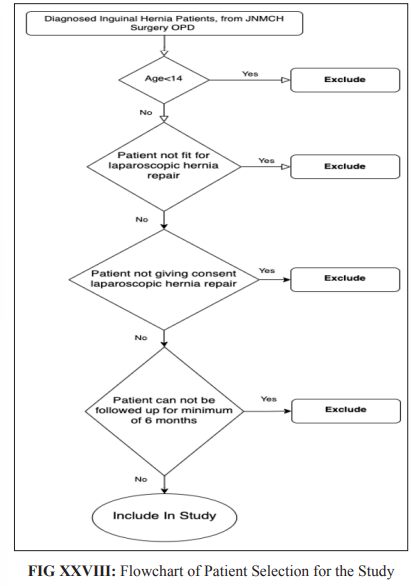
This was a hospital-based, unicentric, prospective study. A total of 91 patients with inguinal hernia enrolled prospectively between November 2019 to June 2021, aged more than 13 years, admitted in JNMCH Hospital were included in this study. All patients were divided into the two group by manual random selection technique. 54 patients were included in the heavy-weight mesh group while 37 patients were allocated to the light-weight mesh group.
• Patients giving consent to be included in the study
• Inguinal Hernia patients of >13 years of age
• Patients of direct or indirect, unilateral or bilateral inguinal
hernia
• Patients not giving consent for study
• Patients who are not fit for general anaesthesia
• Patients with comorbidity that contraindicates laparoscopic
surgery
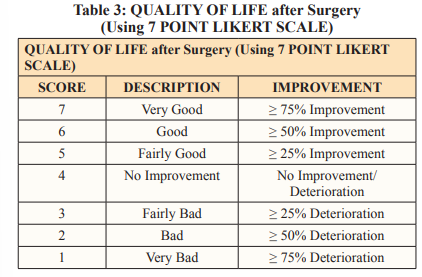
• Patients having bleeding disorders
Detailed history and clinical examination were done in every case before surgery. Informed consent was taken from the patient after they were explained the risks, benefits and complications of the implants and assured that confidentiality would be maintained of their identity and personal details. Post-operatively all patients were evaluated for Infection, Seroma formation, Ileus, Foreign Body Sensation, Groin Stiffness, Delayed Urinary Retention, Testicular Atrophy among male patients, Early postoperative pain on Day 1, 2 & 7, Chronic pain on follow-up 3rd and 6th month, Duration of hospital stay, Duration to start work, Quality of life after surgery (7 points Likert scale) and Recurrence.
Prolene is a heavy-weight non-absorbable mesh. It is made of polypropylene monofilaments with small pores. Its weight is 80 to 85g/m2 with dimensions 10x15cm. Pore size is less than 1 mm.
Ultrapro is a light-weight partially absorbable mesh, made of polypropylene and poliglecaprone monofilaments with large pores (3 to 4 mm). The poliglecaprone monofilaments are absorbed within 90 to 120 days due to hydrolysis. Its weight is 28g/m2 (part of polypropylene that is not absorbed) with dimensions 10x15cm. Pore size is usually 1 to 3 mm.
Pre-Operative Variables: Demographic characteristics - Age
and Gender
Clinical characteristics - location of the hernia, type of hernia
Intra-Operative Variables: Method of repair - TEP/TAPP, Type of Mesh used (Light-Weight or Heavy-Weight mesh).
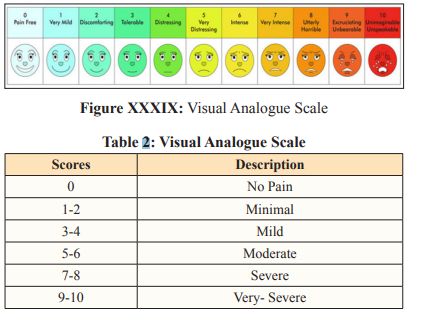
The patients were followed up during the postoperative period for post-operative events, such as postoperative complications (Infection, Seroma, Ileus, Foreign Body Sensation, delayed urinary obstruction, testicular atrophy and Groin Stiffness), Recurrence and Pain-score based on VAS (recorded on a scale of 0 to 10) on Postop days 1-2-7, 3 months and 6 months follow-up respectively}.
Patient data on Duration of hospital stay and Duration to start physical activity was noted. Patients were Questioned on Quality of life after surgery based on 7 points Likert scale at the followup 6 months.
Postoperative management is done as per the protocol attached.
Follow up done for a period of six months following surgery as
follows.
• 7th Postoperative day
• 3rd months
• 6th months
Chronic pain (defined as pain that persisted beyond 3 months of surgery and necessitated prescription of analgesics or any other remedy and recorded as present or absent). Recurrence (defined by any bulge which appeared after surgery at any time during the time period of study and treated by re-surgery or truss this was recorded as present or absent).
Data were collected and entered into a Microsoft Excel sheet. Continuous data were compared in the form of Mean and Standard Deviation using a Unpaired ‘t’ test; while categorical data were compared in the form of percentage and frequency using a Pearson’s chi (x2) square test.
Statistical analysis was done using the International Business Machines Corporation - Statistical Package for the Social Science (IBM-SPSS) software (Norman H. Nie, Dale H. Bent, C. Hadlai Hull) Windows, Version 24, Head-quarter: Armonk, New York. The results were considered significant if the p-value is < 0.05.
This prospective, randomized and comparative study was carried out from October 2019 to January 2022 (enrolled till June 2021) in the Department Of General Surgery, Jawaharlal Nehru Medical College and Hospital, Aligarh Muslim University, Aligarh. A total of 91 patients meeting inclusion criteria with inguinal hernia were included in the study and randomly divided into two groups. 54 patients were placed in Group A (light-weight mesh used) and 37 in Group B (heavy-weight mesh used).
The light-weight mesh repair was found to have better than heavyweight mesh repair in terms of duration of hospital stay and quality of life score with a p-value of 0.0054 and 0.0372 respectively.
While there was no statistical difference between the lightweight mesh repair and heavy-weight mesh repair in terms of postoperative complications (infection, seroma, recurrence, foreign body sensation, groin stiffness, delayed urinary obstruction & testicular atrophy among male patients), postoperative pain (Day1, Day2, Day7, 3rd month & 6th month) and duration of return to work with a p-value of 0.15271, 0.770335, 0.15271, 0.629837, 0.629837, 0, 0, 0, 0.626, 0.7704 , 0, 0, 0 and 0.1888 respectively.
Our showed no statistical difference between the light-weight mesh repair and heavy-weight mesh repair in terms of postoperative complications (infection, seroma, recurrence, foreign body sensation, groin stiffness, delayed urinary obstruction & testicular atrophy among male patients), postoperative pain (early & chronic) and duration of return to work.
In general surgical practice, inguinal hernia repair is one of the commonly performed procedures. Over a hundred years the methods for inguinal hernia repair had very few changes till different laparoscopic inguinal hernia techniques and the synthetic mesh was introduced.
The aims of successful hernia repair include achieving an effective repair with the lowest possible postoperative complications and better outcomes.
This study was mainly undertaken with the aim of comparing the two widely used meshes in laparoscopic techniques, the lightweight mesh and the heavy-weight mesh.
We conducted a unicentric, prospective, randomized and comparative study on 91 patients with Inguinal Hernia diagnosis in the Department of Surgery, Jawaharlal Nehru medical college and hospital, Aligarh Muslim University, Aligarh from October 2019 to January 2022.
In our study groups, 91 Patients were randomly assigned into two groups, 54 patients were placed in Group A (Light-Weight Mesh used) and 37 in Group B (Heavy-Weight Mesh used).
Moheb S Eskandaros et al (12), 2016 did a similar study with a similar study design. They did a unicentric, prospective, computerized randomized and comparative study in 60 diagnosed inguinal hernia patients to compare the 30 cases each of heavy-weight (prolene) mesh & the light-weight (ultrapro) mesh in transabdominal preperitoneal (TAPP) inguinal hernia repair technique.
C Nikkolo et al (13), 2012 also did a similar study with a similar study design, but using an open tension-free Lichtenstein surgical technique on a total of 114 inguinal hernia patients, which were randomized into 57 cases each of the heavyweight mesh (HW) group and lightweight mesh (LW) group.
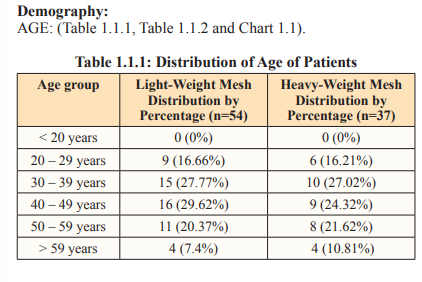
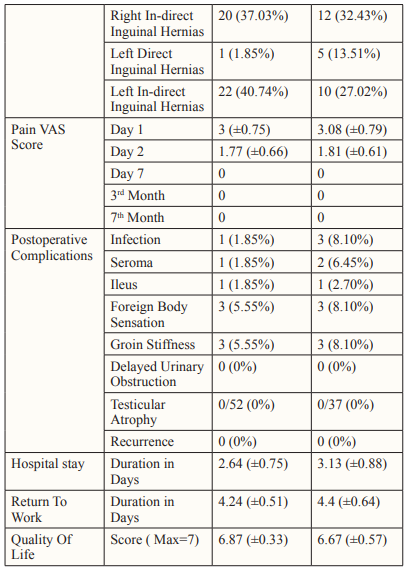
The mean ± SD age of the light-weight mesh group was 41.42 ± 9.63 years, while it was 42.91 ± 14.06 years in heavy-weight mesh group. Though our study inclusion criteria were to include Inguinal Hernia patients of ≥14 years of age, we had the youngest patient of 22 years.
Stefano Bona et al (14), 2017 in her Supermesh Study using 808 primary inguinal hernia found similar age groups, she included all patients of >18 years of age, of both genders; the mean (min-max) age of the light-weight mesh group was 59 years (47-69) years, of the heavy-weight mesh group was 61 (50-70) years respectively. These results were similar and comparable to our results.
Moheb S Eskandaros et al (12), 2016 in their published study compared the outcomes of inguinal hernia repair using (45) heavyweight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) transabdominal preperitoneal (TAPP) patients. In his study, all the patients were men with a mean age (mean ± SD) of 39.8 ± 8.825 years in the light-weight mesh group (group A) ranging from 27 to 55 years. In the heavy-weight mesh group (group B), patients had a mean age of 38.667 ± 9.777 years, ranging from 22 to 55 years. The p-value was 0.692, which was statistically nonsignificant. These results are similar and comparable to our results.
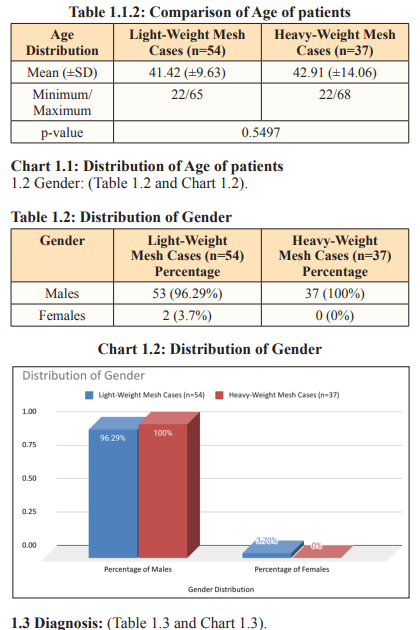
In our study groups, 96.29% (52/54) of all the light-weight mesh and all 100% (37/37) of the heavy-weight mesh group cases were males, while 3.7% (2/54) of the light-weight mesh and none (0/37) of the heavy-weight mesh group cases were females.
Stefano Bona et al (14), 2017 in her Supermesh Study using 808 primary inguinal hernia found similar age groups, she included all patients of >18 years of age, of both genders; Male % (n=768) Female % (n=39) LW male=95% (392), HW male=95% (392); LW female=5% (19), HW female=5% (19) respectively. These results are similar and comparable to our results.
Moheb S Eskandaros et al (12), 2016 in their published study compared the outcomes of inguinal hernia repair using (45) heavyweight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) transabdominal preperitoneal (TAPP) patients. In his study all the patients were men. These results are similar and comparable to our result, but the inclusion criteria were different.
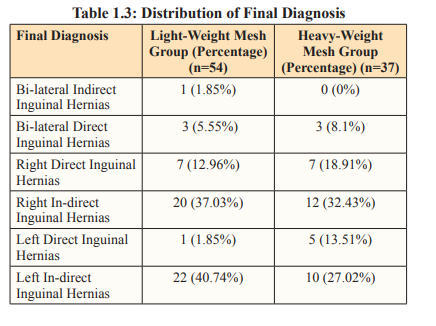
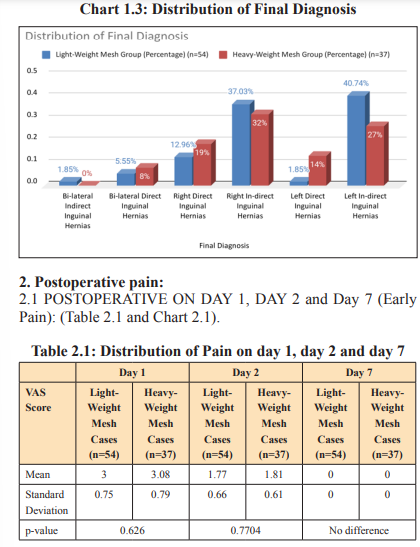
Bilateral indirect inguinal hernias, bilateral direct inguinal hernias, right direct inguinal hernias, right indirect inguinal hernias, left direct inguinal hernias and left indirect inguinal hernias in lightweight mesh group were- 1.85% (1/54), 5.55% (3/54), 12.96% (7/54), 37.03% (20/54), 1.85% (1/54) and 40.74% (22/54); while in the heavy-weight mesh group they were - none 0%, 8.1% (3/37), 18.91% (7/37), 32.43% (12/37), 13.51% (5/37) and 27.02% (10/37) respectively.
Moheb S Eskandaros et al (12), 2016 in their published study compared the outcomes of inguinal hernia repair using (45) heavyweight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) transabdominal preperitoneal (TAPP) patients. In group A (15 patients, light-weight), three patients (20%) had a direct hernia, whereas 12 patients (80%) had an indirect hernia. In group B (45 patients, heavy-weight), nine patients (20%) had direct hernias, whereas 36 patients (80%) had indirect hernias. These results were similar and comparable to our results.
Stefano Bona et al (14), 2017 in her Supermesh Study using 808 primary inguinal hernia found Left side Hernia [% (n)]: LW=46% (181), HW=44% (166); Right side Hernia [% (n)]: LW=54% (216), HW=56% (214); Bilateral : LW=45% (14), HW=55% (39). These results are similar and comparable to our results.
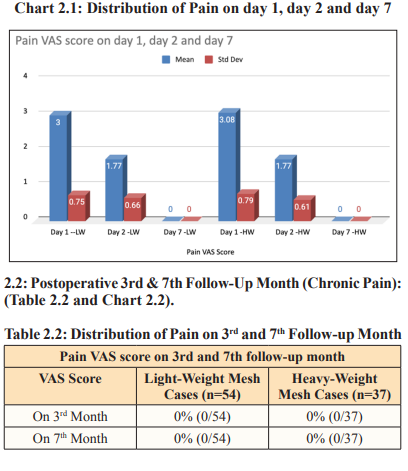
The mean and standard deviation, pain VAS-score on Day 1 and Day 2 of patients in of light-weight mesh group was 3 (± 0.75) and 1.77 (± 0.66); while of the heavy-weight mesh group was 3.08 (± 0.79) and 1.81 (± 0.61) respectively. There was no statistically significant difference in VAS pain score on day 1 with a p-value was 0.626, while on day 2 it was 0.7704.
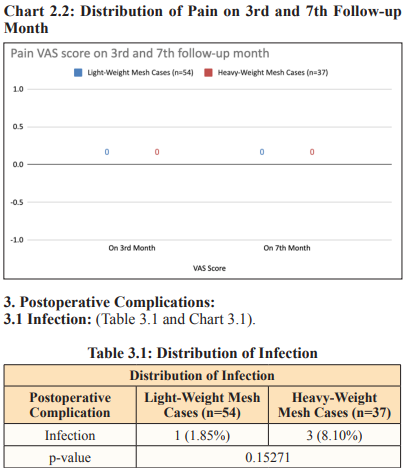
No patient, in any group had any pain on Day 7, none of the patients in our study reported having pain beyond the 5th Day of Surgery. There was no statistical difference between the two groups after the 3rd and 7th-month follow-up.
Michael Kraub et al (15), 2020 published a retrospective questionary based comparative study on elective groin hernia patients using propensity score matching and concluded that light-weight mesh does not have less chronic pain when compared with heavy-weight mesh in repairing elective unilateral primary hernias by the mesh plug technique. These results were similar and comparable to our results.
Moheb S Eskandaros et al (12), 2016 published a study to compare the outcomes of transabdominal preperitoneal inguinal hernia repair using (45) heavy-weight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) patients and concluded that light-weight meshes are superior to the heavyweight meshes in respect to the occurrence of pain. In group A, the first 24h pain had a mean of 2±0.926 and ranged from 1 to 3 on the Numeric Rating Scale (NRS), whereas in group B, the immediate postoperative pain had a mean of 4.2 ±0.944 andranged from 3 to 6 on the NRS. With respect to the follow-up, the pain in group A after 1 week was 1.133 ± 0.990 (ranging from 0 to 3), after 1 month was 0.6 ± 0.910 (ranging from 0 to 3), after 6 months was 0.267 ± 0.594 (ranging from 0 to 2), and after 12 months, none of the patients suffered from any pain. The pain in group B after 1 week was 3.489 ± 1.079 (ranging from 2 to 6), after 1 month was 2.667 ± 1.187 (ranging from 2 to 5) and after 6 months was 2.156 ± 1.205 (ranging from 2 to 5). These results were similar and comparable to our results.
In our study groups, 1.85% (1/54) of the light-weight mesh and 8.10% (3/37) of the heavy-weight mesh group cases had Infection. This difference in Infection was not statistically significant between the study groups with a p-value of 0.15271. Postoperative Infections were superficial and were managed conservatively.
In our study groups, 1.85% (1/54) of the light-weight mesh and 6.45% (2/37) of the heavy-weight mesh group cases had Seroma. This difference in Seroma was not statistically significant between the study groups with a p-value of 0.770335. Postoperative Seromas were minimal and were managed conservatively.
In our study groups, 1.85% (1/54) of the light-weight mesh and 2.70% (1/37) of the heavy-weight mesh group cases had Ileus. This difference in Ileus was not statistically significant between the study groups with a p-value of 0.15271. Postoperative Ileus were rare, of short duration and was managed conservatively.
In our study, 5.55% (3/54) patients in the light-weight mesh group and 8.1% (3/37) patients in the heavy-weight mesh group expressed foreign body sensation to the applied mesh. There was no statistically significant difference in foreign body sensation to mesh between our study groups with a p-value of 0.629837. Complaints of postoperative foreign body sensation to the mesh were minimal and were managed conservatively
In our study, 5.55% (3/54) patients in the light-weight mesh group and 8.1% (3/37) patients in the heavy-weight mesh group expressed groin stiffness (change in abdominal wall motility) at the mesh application site. There was no statistically significant difference in groin stiffness in our study groups with a p-value of 0.629837. Complaints of postoperative groin stiffness were minimal and were managed conservatively.
None of the patients 0% (0/91) in our study reported having delayed urinary obstruction in any type of mesh used (in both groups). There was no statistical difference between the two groups.
None of the male patients 0% (0/89) in our study reported having testicular atrophy in any type of mesh used (in both groups). There was no statistical difference between the two groups.
None of the patients 0% (0/91) in our study reported having recurrence in any type of mesh used (in both groups). There was no statistical difference between the two groups.
Chunlin Zhong et al (1), 2013 published a meta-analysis on a total of 2231 hernias from 11 RCTs and concluded that there was no significant difference in postoperative wound infection (p=0.87), seroma (p=0.89), hematoma (p=0.16), urine retention (p=1.74), testicular atrophy (p=0.71), foreign body sensation (p=0.21) and recurrence (p=0.39). These results were similar and comparable to our results.
J. Li et al (17), 2012, in his published a meta-analysis on “Lightweight versus heavyweight in inguinal hernia repair, a comprehensive literature search” showed no significant difference in postoperative wound infection (p=0.82), seroma (p=0.03; OR=0.80, 95%CI=0.52) testicular atrophy (p=0.81), foreign body sensation (p=0.55) and recurrence (p=0.52). There was no significant difference in postoperative recurrence, seroma, wound infection and testicular atrophy between lightweight mesh versus heavyweight mesh for inguinal hernia. These results were similar and comparable to our results.
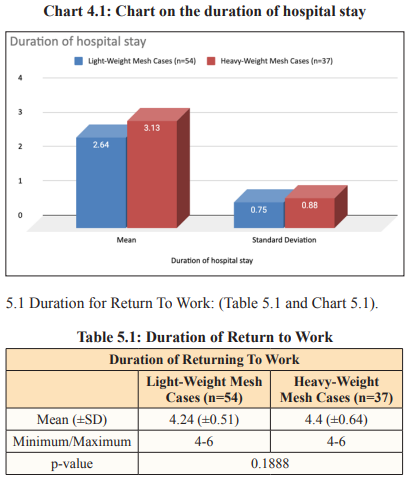
The mean ± SD duration of hospital stay in the light-weight mesh group was 2.64 ±0.75 days and it was 3.13 ±0.88 days in the heavy-weight mesh group. There was a statistically significant difference in the mean duration of hospital stay in our study groups with a p-value of 0.0054.
Moheb S Eskandaros et al (12), 2016 published a study to compare the outcomes of Trans-Abdominal Pre-Peritoneal (TAPP) inguinal hernia repair using (45) heavy-weight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) patients and concluded that light-weight meshes were superior to the heavyweight meshes. Results showed the mean hospital stay for group A (Light-Weight) was 1.4±0.632 days (ranging from 1 to 3 days), whereas in group B (Heavy-Weight) was 1.844±1.882 days. Though the p-value was 0.375, which was statistically nonsignificant, which is different to our result.
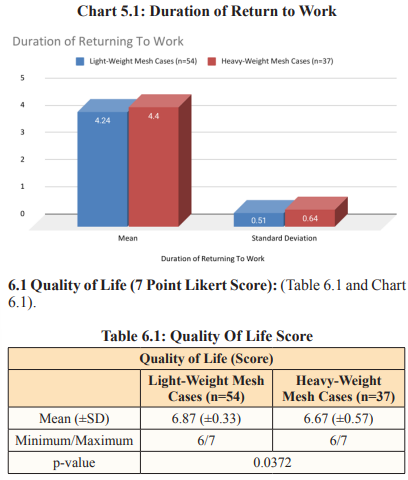
The mean ± SD duration for return to work in the light-weight mesh group was 4.24 ± 0.51 days and was 4.4 ± 0.64 days in the heavy-weight mesh group. There was no statistically significant difference in mean duration for return to work in our study groups with a p-value of 0.1888.
Moheb S Eskandaros et al (12), 2016 published a study to compare the outcomes of TAPP (trans-abdominal pre-peritoneal) inguinal hernia repair using (45) heavy-weight (prolene) mesh versus the (15) light-weight (ultrapro) mesh in sixty (60) patients and concluded that light-weight meshes are superior to the heavyweight meshes. Results showed the patients in group A started to return to work after 5.033±1.189 days, whereas in group B it was 7.867± 2.662 days. He concluded that lightweight meshes were superior to heavy-weight meshes in respect to early return to work. Though the p-value of our study was 0.1888, which was statistically nonsignificant, which is different in this published study
M. Smietañski et al (11), 2012 published a study titled“Systematic review and meta-analysis on heavy and lightweight polypropylene mesh in Lichtenstein inguinal hernioplasty” using 2115 patients of 8 RCTs. The analysis demonstrated that though the number of patients not working after 1 month was almost 4 times higher in the heavyweight mesh group (2.5 vs. 9.5 %); this difference was not significant, similar to our study
Muhammad S. Sajid et al (18), 2013 published a systematic review and meta-analysis using 11 RCTs encompassing 2,189 patients and concluded that the use of light-weight mesh for laparoscopic inguinal hernia repair is not associated with an increased risk forhernia recurrence. The analysis demonstrated that in the fixedeffects model (MD, 2.92; 95% CI, 21.59 to 2.25; z 5 2.70; p-value= 0.007), the time taken to return to work by the patients in the LWM group was statistically shorter than the time taken by the patients in HWM group; this difference was significant, different than our study
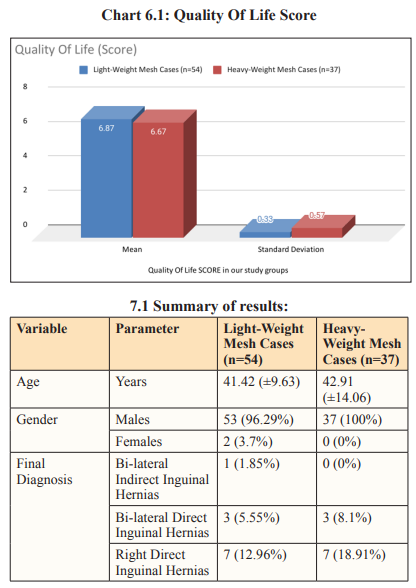
The mean ± SD Quality Of Life Score in the light-weight mesh group was 6.87 ± 0.33 and was 6.67 ± 0.57 in the heavy-weight mesh group. There was a statistically significant difference in the quality of life in our study groups with a p-value of 0.0372.
Chunlin Zhong et al (16), 2013 published a meta-analysis, titled“A Meta-analysis Comparing Lightweight Meshes With Heavyweight Meshes in Lichtenstein Inguinal Hernia Repair” on a total of 2231 hernias from 11 RCTs. The analysis demonstrated that 3 studies evaluated the quality of life (SF-36) after surgery. In the Bringmam (19) and Nikkolo (13) studies, there were no differences in quality of life between the 2 groups, but Smietañski (11) and others found that the lightweight group received a high score in physical function and pain measured after surgery. Thus, the results of the third study are similar to our result in terms of quality of life.
Our study has certain limitations:
The use of mesh in laparoscopic approach for inguinal hernia repair is widely adopted now. In our study the use of light-weight meshes is associated with less duration of hospital stay and better Quality Of Life score with a p-value of 0.0054 and 0.0372 respectively with no increased incidence of postoperative complications in comparison with the heavy-weight meshes. We recommend use of light-weight meshes over heavy-weight meshes to be used in laparoscopic inguinal hernia repair for a relatively better outcome.
