Author(s): Yakob Gebregziabher Tsegay*, Molalegne Bitew, Assegdew Atlaw, Mintsnot Aragaw, Shambel Araya, Mesay Gemechu, Nega Brhane and Tigist workneh
Background: Current studies have presented and analyzed epidemiological, clinical and clinical laboratory features COVID-19 Patients. Studies suggests that patients with severe COVID-19 shows unregulated lipid metabolism and profile but adequate information is not available concerning the association of lipid parameter features with severity of disease its outcome in Ethiopia.
Objective: This study aims to determine the magnitude of lipid profile abnormalities and association of COVID-19 outcome among admitted patients at Millennium COVID-19 care center in Ethiopia.
Methods: A prospective observational cohort study was conducted among COVID-19 admitted patients to investigate lipid profile parameters from January 2021- June 2021. A total of 500 patients confirmed with COVID-19 infection by RT-PCR were included. Dynamic alteration in lipid profiles were recorded and tracked. Data were analyzed using SPSS version 25. P value <0.05 was considered significantly associated.
Result: The median age of the 500 study participants was 55.58+7.707 years, and from these 71.3% of patients were males. This study found that high-density Lipoprotein cholesterol (HDL-C) and Total Cholesterol levels were significantly higher in the severe and Critical disease category. The total cholesterol results showed that significantly higher 25 (5.38%) in severe infection cases than that, (17 (3.4%), 12(2.4%) and 5 (1%) in moderate, mild and critical cases consecutively (P<0.000). Whereas, patients with severe infection had slightly lower of HDL than Mild and moderate infection cases (P=0.000 and P=0.000) respectively. Moreover, a significant decrement in the level of TG was detected in severe infection cases compared to mild and moderate cases (P=0.0001). Hence, the higher TG/HDL-C ratio (3.754) was found in severe infection cases, compared with mild and moderate infection (P=0.001 and P=0.002) respectively.
Conclusion: Lipid function biomarkers like CHO, TG and LDL serum value was found elevated among severe than other patients. Lipid Metabolism biomarkers are a candidate for predicting COVID-19 disease severity in order to guide clinical care and general Public.
The coronavirus SARS_CoV-2 outbreak began in Wuhan, Hubei Province, China in late December 2019 and spread world worldwide with strangely high morbidity and mortality [1]. Coronavirus emerging at the year 2019 (COVID-19) belongs to the family coronaviridae with the genera Beta, Alpha, Delta and Gamma COVID-19e that causes different symptoms mainly fever, pneumonia, shortness of breath and lung infection [2]. COVID-19 is found in various animals and humans. Human COVID-19 (HCoV) includes. HCoV-229E and HCov-NL63 in the genus of alpha COVID-19e and HCov-OC43 and HCoV-HKU1 in the genus of beta COVID-19. HCoVs were first isolated in culture in 1960 from person with upper respiratory disease. In 2002 a betacoronavuruse lineage B (subgenuscovius) originating in bats then spread to humans causing severe respiratory disease named as Severe Acute Respirator Syndrome (SARS) related to COVID-19 (CoV). In 2012 betacoronavuruse in lineage C (subgenus merb-coviruse) transmitted from camel to humans in Saudi Arabia causing the same clinical manifestation as SARSCoV and named as Middle East Respiratory Syndrome related to COVID-19e (MERS_CoV) [3].
This deadly virus infected more than 63.7 million in the world, greater than 13.9 million Americans, more than 1.6 Million Spanish, nearly 115,911 thousand Egyptian and 110,74 Ethiopians. The death toll of COVID-19 more than 274 thousand Americans, near 56 thousand Italians, 6,650 Egyptian and 1,700 Ethiopian were killed. Increasing evidence suggests that immuno comprised patients and hyper inflammatory response are main features of COVID-19 severity and mortality. Sepsis and systematic inflammation are prevalent metabolic disorders associated with severe COVID-19. Moreover, proteome analysis suggests that patients with severe COVID-19 show unregulated lipid metabolism and profile [1-5].
Dyslipidemia is accompanying with respiratory failure, damage to immune system, cardiovascular system abnormality, along with high level of proinflammatory cytokines. In addition, endothelial dysfunction, higher platelet activities and thrombotic complication associated with causes dyslipidemia. The main contributor of high comorbidity and mortality of COVID-19 infection is dysregulation of lipid Metabolism. However, the predictor of value of lipid profile in disease severity and mortality, remains vague yet known [6].
Therefore, this current study was performed an observational cohort study to investigate the lipid profile features of patients with COVID-19 and illuminate the association between lipid features with severity and mortality.
Patients data were collected with structured questionnaire and laboratory samples were investigated at Millennium COVID-19 treatment center laboratory department of 500 laboratoryconfirmed cases with COVID-19 prospectively from January to June 2021. Requests to the laboratory are generated online, and the laboratory results are sent electronically from the laboratory information system (Polytech) to the patient’s electronic medical record.
Patients who had been tested for lipid function test, diabetic function test and cardiac marker tests were included in this laboratory based prospective cross sectional study. Eight milliliters of venous blood were collected in SSGT tube for clinical chemistry test parameters. The lipid function tests, diabetic function and cardiac markers were analyzed using Cobas 6000 automated clinical chemistry analyzer. In most COVID-19 infection, Realtime reverse transcription polymerase chain reaction (RT-PCR) test confirmed cases; routine clinical chemistry tests were performed to assess lipid, Cardiac function and diabetic functions. Among these lipid function tests, Total Cholesterol (CHO), Low density Lipoprotein (LDL-C), High Density Lipoprotein (HDL-C) and Triglyceride (TG) were performed; whereas creatine kinase muscle-brain isoenzymes (CK-MB), and troponin (TnT) were included under cardiac function tests. In addition, Glucose and Glyceride Hemoglobin (A1C) were mentioned as markers for diabetic function tests. All laboratory tests and interpretation were done following the manufacturers’ recommendation and standard operating procedure. Lipid function test abnormalities were defined as the elevation of the following metabolic parameter in serum: CHO >200 mg/dl, TG> 200mg/dl, HDL (35-65mg/dl) and LDL > 100 mg/dl. Cardiac biomarker abnormalities were defined as the elevation of troponin (0-14pg/ml) and CKMB (0-25 U/L). The diabetic profile abnormalities A1C (4.8-6%) and fasting blood glucose in serum dysfunction (75-115 mg/dl).
SARS-CoV-2 was confirmed using RT-PCR-. Two pairs of primers targeting nucleo-capsid protein (N) and open reading frame 1ab (ORF1ab) were amplified and examined. The corresponding sequences for N were 5’-GGGGAACTTCTCCTGCTAGAAT-3’ (F),5’-CAGACATTTTGCTCTCAAGCTG-3’(R),and5’-FAMTTGCTGCTGCTTGACAGATT- AMRA-3’ (probe) and for ORF1ab were 5’ CCCTGTGGGTTTTACACTTAA-3’ (F), 5’ ACGATTGTGCATCAGCTGA-3’(R),and5’-CY3 CGTCTGCGGTATGTGGAAAGGTTATGG-BHQ1-3’ (probe). These diagnostic criteria were based on the recommendations by the WHO.
The study was approved by Institute of biotechnology, University of Gondar ethics and research committee; protocol number IOB/291/04/2021. Data was collected after permission was obtained. All the information obtained from the study participants were kept confidential.
SPSS statistical software package version 25.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Categorical data were expressed as absolute values and percentage and compared using Chi-square test to determine association among categorical variables. The quantitative data were expressed as Mean ±SD and Median values. P value < 0.05 was considered as statistically significant.
COVID-19 patient: any patient who has tested positive for COVID-19 gene as reported by a laboratory given mandate to test such patients by the Ministry of Health [7].
Asymptomatic patient: any patient who has confirmed as positive for COVID-19 but does not have any symptoms. These patients are detected after isolation and contact tracing as done by EPHI [7].
Mild Cases: patients who present with non-specific complaints such as myalgia, conjunctivitis, fatigue and sometimes by upper respiratory tract infection symptoms such as sore throat and runny nose [7].
Moderate: Symptomatic patient meeting case definition for COVID without evidence of viral pneumonia or hypoxia and/or 140 adolescent or adult with clinical sign of pneumonia (fever, cough, dyspnea, fast breathing) but no severe pneumonia including SPo2≥90% on room air [7]
Severe: Adolescent or adult with clinical sign of pneumonia (fever, 145 cough, dyspnea, fast breathing) plus one of the following: respiratory rate >30 breath/min, severe respiratory distress; or SPo2<90% on room air [7]
Critical: Acute respiratory distress syndrome (ARDS) within one 150 week of known clinical insult or new or worsening respiratory symptoms, chest imaging indicating bilateral opacities not fully explained by volume overload, labor or lung collapse, respiratory failure not fully explained by cardiac failure or fluid overload, acute life threatening organ dysfunction, evidence of septic shock with characteristics of persistent hypotension despite volume resuscitation in adults and children [7].
Result Patient Demographics and Clinical Features A total of 500 patients with real time-PCR confirmed COVID-19 disease were included in this study: 298 with Sever disease and 60 with critical disease. Most of the study participants were older than 66 years. The median age of the study participants was 55.58+7.707 years, from these 338(67.5%) of patients were males. The median age was significantly higher in critical (ICU patients) group compared to moderate and severe groups. The duration of symptoms before admission was also higher in severe patients (Table 1).
Table 1: Socio-demographic characteristics and clinical features of study participants at MCCC, Ethiopia, 2021
| Variables | Frequency | Percent |
|---|---|---|
| Age | Mean 55.58+7.707 | |
| Gender | ||
| Male | 338 | 67.6 |
| Female | 162 | 32.4 |
| Disease Severity | ||
| Mild | 58 | 11.6 |
| Moderate | 84 | 16.8 |
| Severe | 298 | 59.6 |
| Critical | 60 | 12 |
| Comorbid | ||
| No comorbidity | 269 | 53.8 |
| Diabetics (DM) | 61 | 12.2 |
| Hypertension (HTN) | 58 | 11.6 |
| Asthma | 10 | 2 |
| Cardiac | 8 | 1.6 |
| HTN+DM | 55 | 11 |
| HTN + Asthma | 3 | 0.6 |
| HTN +DM +Cardiac | 14 | 2.8 |
| ARVI | 10 | 2 |
| COPD | 4 | 0.8 |
| CLD +DM +CHF | 8 | 1.6 |
| Patient outcome | ||
| Death | 74 | 85.2 |
| Improved | 426 | 14.8 |
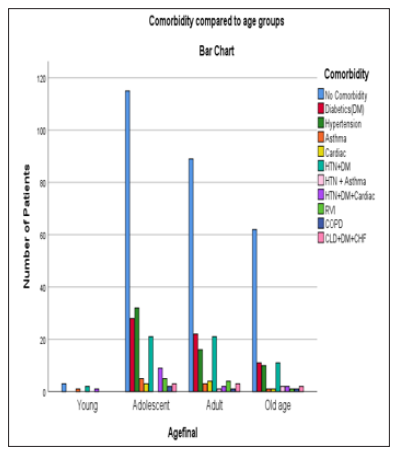
The study participants were classified into four groups mild, moderate, severe and critical; the mild case 58 (11.6%), Moderate 84 (16.8%), Severe 298 (59.6%) and Critical case at intensive care unit 60 (12%) (fig1).
The total cholesterol results showed that significantly higher 25 (5.38%) in severe infection cases than that, (17 (3.4%), 12(2.4%) and 5 (1%) in moderate, mild and critical cases consecutively (P<0.000). Whereas, patients with severe infection had slightly lower of HDL than Mild and moderate infection cases (P=0.000 and P=0.000) respectively. Moreover, a significant decrement in the level of TG was detected in severe infection cases compared to mild and moderate cases (P=0.0001). Hence, the higher TG/HDL-C ratio (3.754) was found in severe infection cases, compared with mild and moderate infection (P=0.001 and P=0.002) respectively (Table2).
Total cholesterol (CHOL) and high density lipoprotein (HDL-C) in male study subjects were significantly higher than female study participants (142.310 (75.54),36.38 (14.79) and (142.054 (42.97),38.81 (11.96) respectively .
Table 2: Lipid biomarker profile level among Mild, Moderate, Severe and Critical cases of COVID-19 Patients at Millennium COVID-19 Care Center, 2021
| Lipid Biomarkers | Mild cases (11.6%) | Moderate cases | Severe cases | Critical cases | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | P.Value | Mean (SD) | P.Value | Mean (SD) | P.Value | Mean (SD) | P.Value | |
| CHOL | 165.4 (39.6) | 0.0012 | 147.9(46.7) | 0.0021 | 135.4(43.4) | 0.001 | 145.9(150.1) | 0.0011 |
| TG | 159.2(105.8) | 0.887 | 165.9(132.9) | 0.541 | 210.2(143.5) | 0.754 | 144.3(75.4) | 0.587 |
| HDL | 44.3(12.7) | 0.000 | 36.5(15.6) | 0.001 | 34.1(11.3) | 0.0013 | 35.3(20.5) | 0.000 |
| LDL | 108.5(33.4) | 0.002 | 92.3(37.5) | 0.001 | 88.8(39.2) | 0.0012 | 84.3(33.6) | 0.000 |
Table 3: The mean (SD) for lipid profile in COVID-19 Patients based on gender at Millennium COVID-19 Care Center, 2021
| Lipid Biomarkers | Male (n=338) | Female (n=162) | P-Value |
|---|---|---|---|
| CHOL | 142.310(75.54) | 142.054(42.97) | 0.000 |
| TG | 381.86(103.96) | 154.25(97.02) | 0.043 |
| HDL | 36.32(14.79) | 34.81(11.96) | 0.000 |
| LDL | 91.29(38.99) | 90.74(36.38) | 0.000 |
The current viral pandemic started in Wuhan city, China is today distributed every corner of the world. This novel viral outbreak has been known as Coronavirus Disease 2019, (COVID-19), and is sustained by Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-COV-2). However, immense information about this virus is not known and the whole world is working on this COVID-19 infection and complication. Studies investigated that there is a pathological modification of total cholesterol (CHOL), Low Density Lipoprotein (LDL), High Density Lipoprotein (HDL) and Triglyceride (TG) their association with COVID-19 Severity and Mortality [8-11].
Lipid metabolism has paramount role in COVID-19 Viral infection cycle. Secondary factors such as genetic alteration may influence on hyperlipidemia or dyslipidemia [11]. This study shows the possible association abnormal lipid profile with patients suffering from COVID-19 Infection. In the recent study increased serum level of CHOL, TG, HDL and LDL correlated to severe COVID-19 patients. Based on the current finding it may be concluded that the alteration on lipid levels frequently changes during COVID-19 infection and is associated with disease severity. this is in line with a studies showed that hypercholesterolemia was indicated in 18% of COVID-19 patients with developing chroming disease Cardiovascular Disease (CVD) and Hypertension and further more hyperlipidemia was occurred in 25% of hospitalized patients [12, 13]. In addition, observational database from 169 hospitals in Asia, North America and Europe, revealing that the prevalence of hyperlipidemia was indicated in 30.2% of survivors from COVID-19 infection and 35% non Survivors [14]. Importantly, the recent study, it was illustrated that serum levels of HDL-C were lower in patients with severe as compared to with mild patients. These results may assist that the idea that HDL-C particles may have some protection against SARS-COV-2 virus as a result their anti-inflammatory and anti-microbial actions [15].
The current study revealed and speculated that hyperlipidemia or increasing levels of CHOL, TG and LDL are most likely due to risk of increasing cardiac complication, acute coronary syndrome, acute myocardial injury, acute cardiac injury, Venous thrombo embolism, lung injury that are most common in patients with preexisting cardiovascular disease with high mortality rate.
The finding of this study may also to reflect the abnormal lipid profile in COVID-19 patients having mild to Critical or patients admitted at Intensive Care Unit (ICU). This may also provide paramount information’s for future researchers about COVID-19 infection and its association with COVID-19 severity
Ethical clearance was obtained from Ethiopia Biotechnology, Institutional Board Research ethics review committee and it was in accordance with the principles of the Helsinki II declaration. Availability of Data and Material
All the available data were included in the manuscript.
Funding: None
Conflict of interest: The authors declare that they have no conflict of interest.
