Author(s): John Raper*, Cody Cissom, Gabe Autry, Waqaar Arshad, Rami Sakaan and Chris Tucker
Left ventricular diverticulum was first described in 1838 and is thought to occur in 0.4% of the population [1,2]. Left ventricular diverticulum is challenging to diagnose due to the asymptomatic nature and lack of consistent ways to describe the outpouching, however it is known that it contains all layers of the heart [3-5]. Previous authors have tried to classify based on using the size of diverticulum compared to the size of the left ventricle [4]. Diverticulum can be classified as either muscular or fibrous and they display contractile features consistent with the remaining heart [3,4]. As much as 30% of left diverticulum cases are not associated with congenital abnormalities and can present with chest pain [3]. Echocardiography and angiography can be used for diagnosis and surgical resection are typically the treatment of choice before complications such as endocarditis, arrhythmia, heart failure, and tamponade occur [1,6].
Takotsubo Cardiomyopathy was first described in 1991 and most often occurs in females due to perceived physical or emotional stress. Takotsubo Cardiomyopathy has an estimated incidence of 100 new cases per million each year and accounts for 2% of all suspected acute coronary syndrome [7]. Diagnosis criteria for takotsubo cardiomyopathy include: no significant history of coronary artery disease, ST elevation and or T wave EKG changes, and absence of pheochromocytoma or myocarditis, and temporary dyskinesis/hypokinesis/akinesis in left ventricle with/without associated apical involvement [8]. Current evidence suggests that post-menopausal women (> 50 years old) are more at risk for takotsubo due to the estrogen deficiency and the noted role of estrogen in reducing the stress-induced damage to the heart. The prevalence of Left Ventricular Diverticulum with Takotsubo Cardiomyopathy is unknown, and the pathogenesis is incompletely understood [7]. Here we present a case of Takotsubo Cardiomyopathy a newly diagnosed Left Ventricular Diverticulum. To our knowledge, there is only one other reported case in 2008 [9].
74-year-old female with past medical history of CAD s/p CABG, A. fib on warfarin s/p 2 cryoablations, obesity, and hypothyroidism presented for chest pain.
Initially admitted for chest pain and elevated troponin of 0.116 (reference range 0-0.034) before trending to a peak of 2.67. Shortly after her admission she developed acute worsening of substernal chest pain 10/10 radiating to left arm. EKG was obtained and appeared Anterior lateral ST elevation suggestive of anterior lateral STEMI. Of note, patient had severely elevated INR but due to patient's dynamic EKG changes suggestive of anterior lateral STEMI, patient was emergently brought to cardiac Cath Lab. Heart rate in the 80s and respiratory see mildly labored but O2 saturation was maintained between 90 to 98%. STEMI team was subsequently activated, and patient was taken to Cath Lab. Findings in the Cath lab: CTO of proximal LAD, patent LIMA to LAD which has a patent stent distal to the anastomosis. Left ventricular diverticula, EF estimated at 15% with signs suggestive of Takotsubo cardiomyopathy. Patient was started on Coreg, Entresto, Spironolactone, and Farxiga. Plans for subsequent follow up for TTE for heart failure with reduced ejection fraction. Also plans for follow up with cardiothoracic surgery to discuss possible resection of diverticulum.
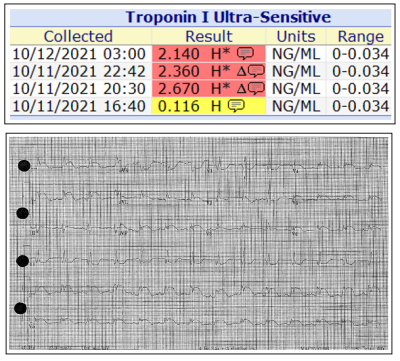
Figure 1: Shows initial troponin trending upwards with a max of 2.67 and a ST elevation in the anterior lateral distribution.
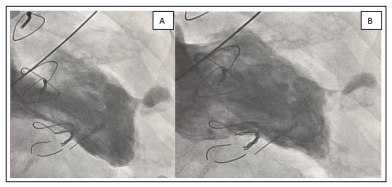
Figure 2: Reveals a dilated left ventricle consistent with takosubo cardiomyopathy in addition to left ventricle diverticula measuring approximately 18 mm x 26 mm. Evidence of diverticulum contraction can be seen when comparing Fig. 2A (diastole) vs Fig. 2B (systole)
This case report is the second report of takosubo cardiomyopathy with left ventricular diverticulum. We are unsure the mechanism or the prevalence of these two conditions occurring together. This patient presented with classic STEMI features and an abnormal EKG of what looked to be anterior-lateral STEMI, but ischemia was ruled out during CATH lab procedures. The patient was also a post-menopausal female which is consistent with current evidence suggesting this is an affected population for takosubo’s cardiomyopathy. We are unsure at the present time if the left ventricular diverticulum contributed to the acute ischemic presentation as this has been reported in the past [3].
