Author(s): Maryam Hammad*, Rabab Alkhayat and Fayza Haidar
Mesenteric cysts are rare, variably-sized intra-abdominal lesions developing during childhood. Their symptoms vary from being asymptomatic and incidentally found to non-specific, presenting as lower abdominal pain, nausea and vomiting, constipation and diarrhea. Clinically, these abdominal masses may be palpable in more than 50% of patients. The diagnosis of these lesions can be made accurately radiologically through abdominal ultrasound and CT. The treatment of choice is complete surgical resection. Hereby we report the clinical course of a 5 year old child with a mesenteric cyst who complained of acute abdominal pain, constipation and vomiting and were surgically treated after being diagnosed with a mesenteric cyst based on radiological examination.
Mesenteric cysts are benign, rare, variably-sized intra-abdominal lesions developing during childhood. They occur anywhere near the omentum or mesentery of the gastrointestinal tract with probable extension to the retroperitoneal region [1]. The incidence of mesenteric and omental cysts has been reported in about 1 case per 20,000 in children, and 1 in 105,000 cases in adult. About onethird of the cases occur in children younger than 15 years old, and the mean age-of-onset is 4.9 years [2]. Presenting symptoms are variable and non-specific in most of the cases. These symptoms include variable intensity of abdominal pain, vomiting, constipation or diarrhea and abdominal distension. The diagnosis of these intraabdominal lesions can be accurately suggested and made through radiological examination like abdominal ultrasound and computed tomography studies. Treatment is surgical, with complete resection of the cyst through laparotomy or laparoscopy [3].
On 26th May 2021, 5 year old male (17.5 kg of actual body weight) a known case of Alpha Thalassemia, G6PD reduced activity, chronic constipation and anal fissures, presented to our tertiary care hospital (Salmaniya Medical complex) accident and emergency department with one day history of acute lower abdominal pain, radiating to right upper quadrant and pelvic area, nausea and non-bilious vomiting. On physical examination, patient is afebrile complaining of colic’s and rolling in bed. He has no abdominal distension, with soft abdomen and voluntary guarding and lower abdomen mild tenderness. Patient’s genitalia are normal and both testis are descended. He was admitted to the pediatric surgical unit for a suspected partial abdominal obstruction for further investigation. Patient initial labs were as the following: WBC count (12.45x10^9/L), RBC count (5.04x10^12/L), Hemoglobin (10.1g/dL), Neutrophils (83.5%), and Neutrophils Absolute Count (10 x10^9/L), Glucose (Random) 5.9mmol/L, UREA 5 mmol/L, Creatinine 27.00 μmol/L, his electrolytes were within normal limits and his urine test was normal as well. Patient was taken for an abdominal and a pelvic ultrasound scan (Figure-1) and computed tomography studies (Figure-2) and the tests concluded that the patient has a large retroperitoneal multi-cystic mass like lesion with multiple internal septation measuring 15 X 12 CM in size encasing the small bowel (mainly jejunum bowel loop) with no intestinal obstruction. The radiological features are most consistent with a congenital mesenteric cyst.
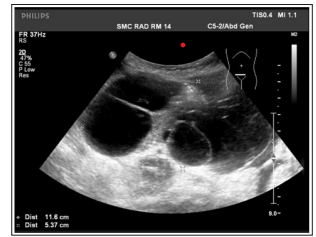
Figure 1: Ultrasonography scans showing a large multiloculated mass with a well-defined wall and multiple internal septation
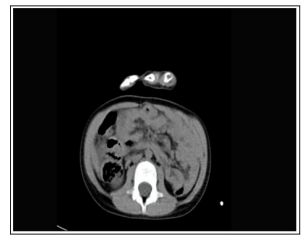
Figure 2: Abdominal computed tomography (CT) scan showing a large multiloculated cystic mass with fine septations (about 11 cmx8 cm).
After that, patient was admitted to the pediatric surgical ward, kept on IV hydration and antibiotics and a scheduled laparotomy was performed the next day and intraoperative findings were a large mesenteric cyst measuring around 15 X 12 CM in size nearly 20 CM from duodenojejunal junction. The cyst was compressing and flattening out the proximal jejunum.
Nearly 15 CM of bowel was excised which was adhered to the cyst. The remaining 200 cm of small bowel till ileocecal valve was normal looking with no gangrene or perforation. The excised cyst along with the adherent bowel loop were sent for the histopathology examination.
The histological diagnosis was made on hematoxylineosinstained slides along with The histological diagnosis was made on hematoxylineosin- stained slides along with immunohistochemistery studies on the slides. Sections of the sampled tissue were evaluated through light microscopy (Olympus, CX41).
As shown in (Figure-3 A and B), Gross examination of the specimen reveals segment of bowel with an attached cystic mass. The bowel measures 9 cm in length and 2.5 cm in diameter. The outer surface looks unremarkable. Attached to its mesenteric side, a multilobulated cystic mass weighing 180 g and measuring 11x8x4 cm. The mass is away by 4 cm from one surgical longitudinal resection margin of the bowel and 2 cm from the other resection margin. It is 0.5 cm away from the bowel wall (mesenteric side). On opening the mass, it is a multiloculated mass filled with clear seromucinous fluid. Its inner surface is smooth without any mural nodules. On opening the bowel, mucosa looks unremarkable. No polyps or growth noted. Representative sections are submitted. Microscopic examination of the submitted tissue sections which are hematoxylin-eosin-stained slides (Figure-4.A) display small bowel mucosa with preserved villous architecture and mild chronic inflammation in the lamina propria extending focally to the muscular layers. A multiloculated cystic mass (Figure-4.B & C) was noted in the mesentery, lined by a single layer of endothelial cells. The underlying fibrous stroma contains multifocal lymphocyte collection. Cyst lumen is filled with pale eosinophilic lymphatic material. No cytological atypia or architectural complexity noted. No ulceration, features of chronicity, granulomas, viral inclusion, dysplasia or malignancy noted. Both resection margins are viable.
D2-40 stain (Sensitive and specific stain for endothelial cells lining the lymphatic channels) highlights the endothelial cyst lining (Figure -4.F).
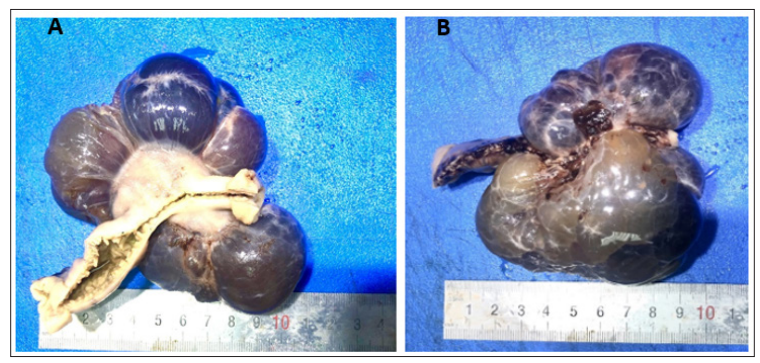
Figure 3: A and B. Photograph showing gross morphology of a giant mesenteric cyst. A multiloculated cystic mass attached to the bowl loop with intact intestinal serosa measuring
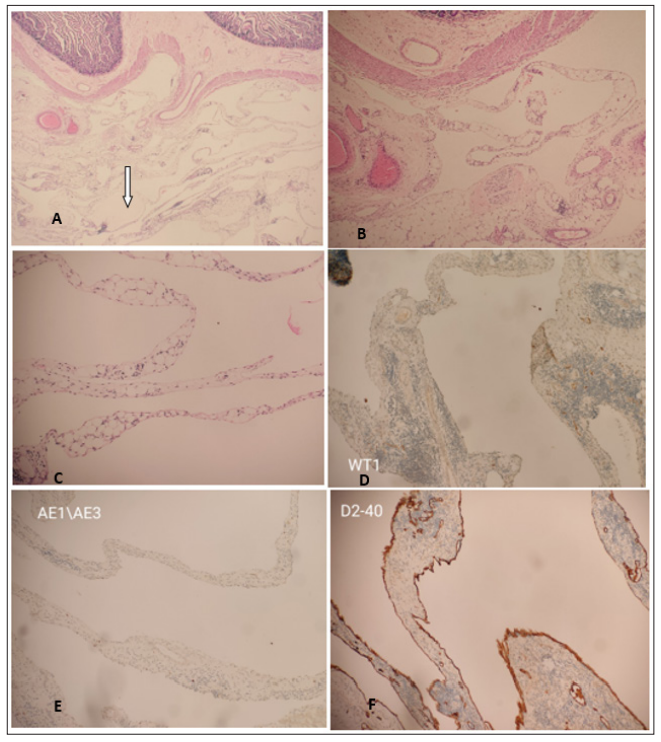
Figure 4: A. Hematoxylin-eosin-stained sections and immunihistochemical stained sections of the cyst. A.Cyst in the mesentery of small bowel filed with pale eosinophilic material (arrow). (Magnification x 20/0.08 NA). B Cyst in the mesentery with a further magnification of the tissue (Magnification x 40/0.40 NA). C The cyst lined by a single layer of endothelial cells. The underlying fibrous stroma contains multifocal lymphocyte collection (magnification x 40/0.08 NA). D. Cyst lining focally positive for WT1. E.Cyst lining negative for Pancytokeratine. F. Cyst lining is diffusely and strongly positive for D2-40 tissue (Magnification x 40/0.40 NA).
Mesenteric cysts are very rare intra-abdominal cystic tumors with a prevalence from 1:100,000 to 1:250,000 of hospitalizations in adults and 1:20,000 in the pediatric population [4,3]. They were first described by the Italian pathologist Antonio Benivieni during the autopsy of an 8-year-old child in 1507 [1,2].
The origin of mesenteric cysts are not fully understood due to the paucity of the reported cases. However, In the literatures, most of these cysts were considered to develop from lymphatic duct obstruction, lymphatic duct injury, lymph node degeneration, ectopic lymphatic tissue proliferation, and failure of the mesenteric sheets to fuse together [3,5]. Other considerable etiologies were congenital diseases, diverticula, pelvic cavity surgery, and inflammatory pelvic disease.
The presentation of mesenteric cysts vary from being asymptomatic and incidentally discovered to presenting as acute abdomen with nausea, vomiting, abdominal pain and bowel obstruction. These symptoms are dependent on the location of the cyst, its size and number. Usually, these cysts are found in the retro-peritoneum area, along the mesentery of the bowel. In a review series of 162 patients, 60% of mesenteric cysts occurred in the small-bowel Mesentery, 24% in the large-bowel mesentery, and 14.5% in the retro-peritoneum [1]. These cysts are generally slow-growing, and benign. Their size varies, with a mean up to 10 cm in diameter (12.7 cm in maximum diameter in our case). Sometimes, these cysts can be complicated by perforation, hemorrhage, infection, volvulus or torsion causing acute intestinal obstruction [6].
Several classification systems of mesenteric cysts exist. However, the most comprehensive and widely used, is that proposed by de Perrot et al. Based on the histological features of the cyst, six different types are present: “(1) cysts of lymphatic origin (simple lymphatic cyst and lymphangioma); (2) cysts of mesothelial origin (simple mesothelial cyst, benign cystic mesothelioma, and malignant cystic mesothelioma); (3) cysts of enteric origin (enteric cyst and enteric duplication cyst); (4) cysts of urogenital origin; (5) mature cystic teratoma (dermoid cysts), and (6) pseudocysts (infectious and traumatic cysts) [7,8].
Moreover, some other rare types of mesenteric cysts do exist, such as mucinous mesenteric cyst of the sigmoid mesocolon and mesenteric cysts caused by endometriosis [7,8].
Diagnosis modalities for mesenteric cysts are the same as the intraabdomenal tumors which are the radiological examination in particularly the ultrasound, CT and MRI. In most cases, the diagnosis can be accurately made by these modalities. Although the ultrasound examination can be more sensitive for the septation and the multiloculatity of the cyst than the CT [7]. Depending on the content of the cyst (clear fluid, chyle or, rarely, hemorrhagic fluid), the density of the cyst can vary in the CT and MRI. Presence of fine calcifications are found usually [8]. In some cases, accurate diagnosis by radiological modalities alone can be challenging due to the the existence of mimickers including loculated ascites, gastrointestinal duplication cysts, pancreatic pseudocyst, cystic pancreatic tumor, and peritoneal inclusion cyst [8].
Although commonly benign, malignant forms of mesenteric cysts have been rarely reported. Malignancy presents in only 3% of the cases [5,8,9]. These cases were having a malignant cyst lining or a focus of gastrointestinal stromal tumor. In addition, serous cystadenocarcinoma of the mesentery and malignant transformation of benign mesenteric cyst were also seen [8]. Rare cases of pseudomyxoma peritonei followed the rupture of a hitherto benign mesenteric cyst after its malignant transformation were also reported. For this reason, excision of the intact cyst without rupture should be the primary goal. In addition, following excision of the cyst, the thorough histological examination is mandatory to specify its type and more importantly, to exclude the rarely encountered malignant forms [8].
Treatment of choice for the mesenteric cysts are the complete surgical resection either by open laparotomy or laparoscopically. In 20 to 60 percent of cases, resection and enteric anastomosis (Figure 5 A to D) to may be required in addition to the resection of the cysts [9]. In the rare cases, where full intestinal retention is not possible after en-bloc intestinal resection, temporary ileostomy is an appropriate option [9]. In a few cases, such cysts have been treated through ultrasound drainage and ethanol sclerotherapy [9].
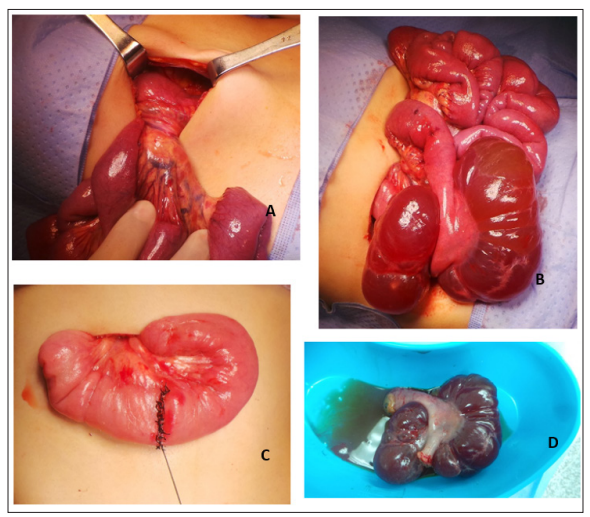
Figure. 5: A & B. Operation findings of the Mesenteric cyst attached to the mesentery of small bowel. C. resection of the cyst and enteric anastomosis done. D. The resected small bowel segment with its mesentery and the attached cyst
Due to its rarity, mesenteric cysts continue to be challenging for radiologist, pathologist and surgeons. However, the complete surgical resection of the intact cyst along with extensive sampling and the through histopathological examination of the cyst is the main primary goal of treatment. This is achieved by open lapratomy approach. However, in the era of minimally invasive surgeries, laproscopic approach is nominated to replace it. Wherever the approach is, caution should be exercised to avoid cyst wall rupture, which may lead to recurrence if part is left behind, or dissemination of malignancy, if the cyst was of the rare malignant variant or a malignant mimicker.
