Author(s): Somashekharayya Hiremath
Microwave ablation (MWA) is a new and improved thermal ablation technology that uses electromagnetic waves to accurately target tissues. Conventional thermal ablation techniques, such as radiofrequency ablation (RFA), are less efficient and precise than MWA in treating tumors and other pathological conditions. Technology’s ability to generate higher temperatures without requiring grounding pads minimizes complications, while advancements in thermal control systems and real-time navigation platforms enhance procedural accuracy. In this paper, the mechanisms, applications, and effects of MWA are discussed while comparing it with the conventional methods and the increasing use of MWA in minimally invasive therapies. With its capacity to manage bigger tumors, lower rates of recurrence, and new clinical applications, MWA is changing the face of today's modern medical treatments.
Thermal ablation has been developing fast in the last few decades to meet the demand for non-invasive yet highly effective treatment options for different medical conditions, especially in oncology. Among heat-based technologies, microwave ablation (MWA) has emerged as a promising alternative to traditional modalities such as radiofrequency ablation (RFA) and high-intensity focused ultrasound (HIFU) [1, 2]. Unlike these methods, MWA utilizes electromagnetic waves to induce dielectric heating, achieving higher tissue temperatures and larger ablation zones in shorter timeframes [3, 4]. This capability has positioned MWA as an ideal solution for treating larger tumors and anatomically complex regions [5].
The unique mechanisms of MWA, such as dielectric hysteresis, allow it to bypass limitations associated with tissue impedance, making it particularly effective in high-water-content tissues like the liver and kidneys [6, 7]. This paper delves into the MWA system, its mechanisms, applications, challenges and scope, providing a comprehensive understanding of microwave ablation medical devices role in modern medical treatments.
Traditional thermal ablation techniques face significant challenges. These challenges include limited thermal penetration, susceptibility to heat sink effects caused by adjacent blood vessels, and reliance on tissue electrical conductivity for energy delivery, which restricts their applicability in certain anatomical regions [4, 6]. Additionally, the need for grounding pads increases risks like burns and procedural complications, which further threaten patient safety and procedural efficiency [8]. As a result of its special heating system and innovative control systems, MWA is found to be a better alternative in order to address these constraints [7, 9]. MWA does not depend on electrical conductivity for its action, so it provides more uniform and deeper penetration into the tissue with less heat loss due to perfusion than other ablation methods [5, 9]. MWA works at higher temperatures and generates bigger and more predictable ablation zones, which makes it more appropriate for use in treating larger and anatomically more complex tumors [2, 11].
Microwave ablation (MWA) is a groundbreaking tissue ablation technology that leverages electromagnetic energy in the microwave spectrum (300 MHz to 300 GHz) to achieve precise and effective thermal ablation [6, 11]. This innovative approach introduces several technological advancements that address the limitations of traditional thermal ablation technologies [1, 3].
The core mechanism of MWA is based on dielectric hysteresis, a process in which electromagnetic waves interact with polar molecules, such as water, in the target tissue [2, 9]. As these polar molecules attempt to align with the rapidly alternating electric field, their oscillation generates kinetic energy converted into frictional heat. This localized heat leads to the destruction of targeted tissues [4, 9]. Unlike RFA, which relies on electrical currents and is limited by tissue impedance, MWA produces a propagating electromagnetic field that enables uniform heating and significantly higher temperatures [5, 11]. This unique mechanism allows MWA to effectively treat tissues with high water content, such as the liver and kidneys [7, 8].
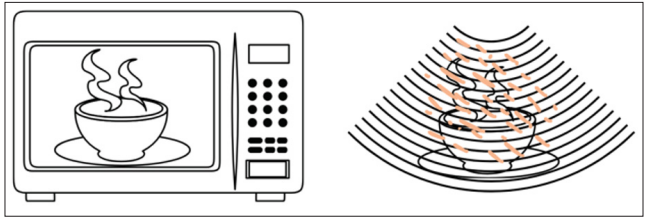
Figure 1: Microwave Technology
Figure 1 visually represents how Microwave Frequency Technology facilitates Active Heating through Field-Based Heating.
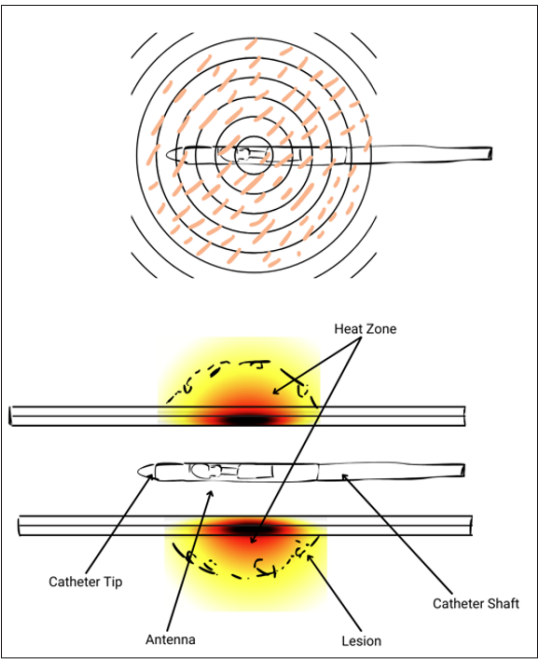
Figure 2: Microwave Ablation Device Mechanism of Action
Figure 2 showing the Circumferential MICROWAVE Technology operates through a MECHANISM OF ACTION based on heat- based ablation, where microwave energy is used to destroy targeted tissues. A centrally deployed MW radiator dielectrically heats tissue in a toroidal volume surrounding the artery without contacting the artery wall, ensuring precise and controlled ablation.
Thermal control systems such as Thermosphere Technology are an advancement that has increased the safety and efficacy of MWA [6]. This system integrates three critical components for the optimization of energy delivery and thermal management [4]. Field control is the maintenance of the electromagnetic field to ensure that energy delivery to the targeted area is constant [2]. Thermal control prevents heat leakage to the surrounding healthy tissues to minimize collateral damage [11]. Wavelength control adjusts energy delivery based on the electrical properties of the target tissue for effective ablation [3]. All these controls eradicate problems like the heat sink effect, a major issue in highly perfused tissues, and produce well-defined, spherical ablation zones for better treatment results [9, 8].
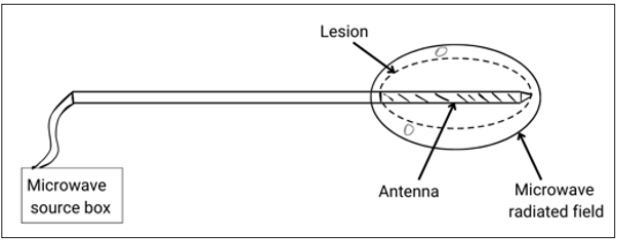
Figure 3: Microwave Ablation System
Figure 3: Microwave Ablation (MWA) system consists of primary components: a generator, power distribution system, and antenna, all working together to deliver microwave energy to targeted tissues.
Real time 3D navigation systems have further revolutionized MWA procedures by improving procedural accuracy and safety [7]. MWA systems provide advanced features, including three- dimensional visualization of the tumor and surrounding anatomy, real-time tracking of antenna placement, and predictive modeling of ablation zones [9, 12]. In addition to ensuring full tumor coverage and reducing the possibility of harming non-target tissues, these features allow surgeons to make intraoperative modifications and monitor the process in real time [5].
MWA is positioned as a groundbreaking tissue ablation method because of its unique energy distribution characteristics, enhanced thermal control systems, real-time navigation platforms, and complex mechanisms [1, 8].
Microwave ablation (MWA) is a flexible technique for treating cancerous and non-cancerous disorders because of its numerous uses in different medical specialties [3]. MWA has demonstrated remarkable efficacy in the treatment of solid tumors in oncology [4]. For example, it provides a minimally invasive option with encouraging results when used to treat liver metastases in patients who are not candidates for surgical excision [6, 12].
Its usefulness in treating non-small cell lung cancer has also been shown by trials showing its effectiveness in treating lung cancers, such as the MARK 1A Series (NCT02673021) [7]. MWA is also viable for treating thyroid nodules, providing a minimally invasive solution for benign and malignant thyroid lesions [2, 11]. MWA has shown remarkable success in treating osteoid osteomas and metastatic bone cancers in bone tumors, where traditional surgical approaches might be more invasive and complex [3, 9]. Beyond oncology, MWA has significant applications in non-oncological conditions [11]. It has been employed in renal denervation procedures to treat resistant hypertension by disrupting sympathetic nerve activity in the renal artery, thereby reducing blood pressure [9]. MWA also manages cardiac arrhythmia in cardiology by ablating pathological cardiac tissues responsible for abnormal rhythms, restoring normal cardiac function [5].
The adoption of microwave ablation (MWA) is revolutionizing patient care by addressing many limitations of existing thermal ablation technologies [2, 8]. Its transformative impact is evident in several critical areas. The first benefit of MWA is that it increases treatment effectiveness because it can reach higher tissue temperatures, more than 100°C to destroy targeted tissues and thus significantly lower recurrence rates [4]. Also, its characteristic of producing larger ablation zones makes it suitable for the treatment of tumors up to 5 cm in size, more than the current modalities [3, 6]. As a safer alternative for therapy, it reduces harm to nearby healthy tissues, increases procedural precision, and consequently, the risk of complications is reduced [5]. Another outcome of MWA is a significant reduction in cost. Healthcare expenses decrease because successful ablation requires fewer sessions and shorter treatment duration [7].
The potential of microwave ablation (MWA) expands its clinical applications while propelling innovation in medical device technology. Personalized medicine represents a significant area of advancement because antenna designs and energy delivery systems match individual patient anatomy along with their specific tumor characteristics [11, 9]. Customization during procedural steps leads to better outcomes because treatment becomes more precise and effective [4]. The integration of artificial intelligence (AI) with MWA systems brings unique transformative capabilities. AI-driven models can optimize treatment planning, accurately predict ablation outcomes, and provide real-time adjustments during procedures, significantly improving safety and efficacy [6, 9].
MWA procedures produce high heat, which may raise the temperature of non-target tissues, thus increasing the chances of complications [1, 3]. Antenna cooling systems and field control mechanisms that help maintain heat within the targeted region are critical in reducing the probability of healthy tissue ablation [11, 9]. Uniform energy distribution across varied tissue types is another complexity in MWA. Microwave energy can only achieve uniform heating when tissues of varying properties, moisture levels, and density are present because the properties of these tissues affect how energy is absorbed and spread [5]. The consequence of this variation is that some residual viable tissue may remain, which can lead to treatment failure or recurrence [7, 12]. Therefore, the development of methods to provide uniform energy delivery through diverse tissue types is essential for the effective application of MWA in varied tissue environments [8].
Another challenge is the absence of real-time monitoring systems that can be used to make intraoperative adjustments [4, 6]. Real- time monitoring of the ablation process is essential in dynamic and variable anatomical environments. Real-time imaging technologies and navigation platforms give the clinician continuous feedback on the ablation zone, antenna position, and tissue response, which can help to increase the accuracy of ablation [2, 9]. These systems provide for exact adjustments to be made during an operation to guarantee that the ablation process is both accurate and effective [3]. These challenges need to be overcome for the full potential of MWA to be realized as a groundbreaking technology in current medical treatment protocols [5, 11].
Microwave ablation represents a paradigm shift in heat-based medical treatments. Due to the overcoming barriers of conventional methods and implementation of new management and guidance solutions, MWA has become the best choice for oncologic and non-oncologic purposes. Microwave Ablation technology's potential to provide speed, safety, and treatment efficacy makes it a promising technology for current and future applications in medical practice. AI integration, personalized antenna designs, and expanded applications will enhance the position of MWA as a cornerstone of minimally invasive therapies in the future. As feature research refines its mechanisms and clinical applications, microwave ablation is a testament to medical technology's power to revolutionize patient care and redefine therapeutic standards.
