Author(s): Nithin AK* and Sagar Jose
A concussion could be a delicate variety of traumatic brain injuries (mTBI) caused by a bump, blow, or jolt to the head. The first injury in a very delicate concussion could be a contusion (bruising) the brain. However in moderate to severe cases, haemorrhage (bleeding) of the brain can occur. The most common causes of concussions are sports injuries, bicycle and automotive accidents, and falls.
Purpose: This study aimed to use activity and electrophysiological assessments to analyse the association between hearing disorder and traumatic brain injury.
Method: The current work describes the case of a 25-year-old male who was brought to the department with bilateral hearing impairment with no different otological symptoms. The patient’s history concealed that he had encountered a road traffic accident 2 weeks prior. The patient had no hearing issues prior the insult. The patient conferred during this case study underwent multiple tests including behavioural, physiological and electrophysiological analyses.
Conclusion: All analyses concluded that TBI will have a sway on the sensory system and may cause hearing disorders. This study highlighted the particular impact of TBI on the auditory system and so, the importance of receiving a full audiological assessment post TBI.
A concussion may be a delicate type of traumatic brain injury (mTBI) caused by a bump, blow, or jolt on the head. The first injury during delicate concussion may be a contusion (bruising) of the brain. However, in moderate-severe cases, haemorrhage (bleeding) of the brain can occur. The most common causes of concussions are sports injuries, bicycles and automotive accidents, and falls. Folks that have already sustained one concussion tend to be additional and at risk of having another. Although a concussion is not a critical injury and other people typically recover quickly, it can cause serious symptoms, including headaches, dizziness, and loss of consciousness, confusion, fatigue, and emesis. A concussion affects hearing and balance [1]. Hearing disorder will occur thanks to physical harm to the peripheral sensory system [2, 3]. Proprioception and balance difficulties, which can embody light-headedness, vertigo, nausea and visual impairments, when a concussion occur because of harm to the peripheral or central proprioception systems [4, 5].
Concussions have become a standard medical topic over the past 20 years. Medical specialists have realized that despite the degree of impact, a concussion will have a good array of symptoms and negative effects. A medicine analysis should be performed to live sensory and motor responses, as well as vision, hearing, balance, and coordination. The brain can be a terribly delicate organ that is protected by the bone. Accidents, falls, or abrupt impacts may result in concussion or traumatic brain injury (TBI). Due to the uncertainties concerning mild TBI, the main focus should not be on identification, diagnosis, or misdiagnosis, which will result in inappropriate treatment. Gentle TBI may be transient in nature; however, it can even cause vital disruption in employment, education, and relationships and it should not be reduced. Audiologists ought to conjointly note that sensory system manifestations of TBI will considerably affect treatment and rehabilitation outcomes, and area unit the explanation that audiologists ought to be a part of a knowledge-based approach to TBI care.
There have solely been a number of studies that have aimed toward describing the audiological standing of people plagued by TBI. The aim of the current study was to examine the hearing standing of a belligerent individual who suffered TBI during a road traffic accident and to visualize whether there is a link between TBI and hearing impairment. Elaborate audiological and concussion assessment tests were performed.
A 25-year-old male subject was referred to the department with bilateral deafness and no alternative otological symptoms. History from the patient explicitly hit the head during a road traffic accident fortnight ago. The patient had no hearing issues prior the insult. Furthermore, an elaborate history of the incident revealed that the patient had no apparent bone injuries, as discovered by temporal bone computed tomography (CT), and there was no loss of consciousness. The patient remained in the altered sensorium for 12 -14 hours. His Glasgow Coma Score (GCS) upon arrival at the hospital was 13 (E4, M5, V4), and the severity of his concussion was classified as grade II.
Ethical approval was obtained from the Institutional Ethical Committee before conducting the study, and informed consent was obtained from the participant explaining all the procedures involved in this study. An in-depth history was obtained, followed by that otoscopic analysis to observe the external acoustic meatus and eardrum standing. All audiological evaluations were performed in a sound-treated space. Pure tone audiometry was dispensed using the MAICO MA42 twin-channel measuring system. The air conductivity threshold and bone-conduction threshold were measured. The thresholds (minimum level of hearing) for air conductivity were measured a transducer TDH39 (770 Park Ave, Huntington, NY11743, US), with frequencies varying from 250 Hz to 8000 Hz with intensity minus ten dBHL to 120 dBHL, and also the pure tone average was measured by a mean of 4 frequencies, 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz. Bone conductivity was checked with test frequencies from 250 Hz to 4000 Hz with intensities from minus ten dBHL to seventy dBHL (Radio ear B71 bone vibrator). Speech audiometry was performed, as well as speech reception threshold measurement of foot words, and speech discrimination score, measurement of phonetically balanced words. The tympanogram and acoustic reflex thresholds were assessed using GSI tympstar instrument. The tympanogram was measured employing a 226 rate probe tone, with sweep pressures ranging from -200 dapa to +400 dapa. Ipsilateral and contralateral acoustic reflexes were obtained at 500 Hz, 1000 Hz, 2000 Hz & 4000 Hz at 90, 100, and 110 dBHL, respectively. The patient was requested to sit quietly and not move throughout the procedure. Distortion product Oto acoustic emissions (DPOAEs) were recorded using an IHS Jr instrument to ascertain the outer hair cell (OHC) performance. The twostimulus tone frequency F2/F1 had a quantitative relationship of 1.2. The intensities of the tone pairs were 65 and 55 dB SPL for L1 and L2, respectively. Two separate runs per ear were collected to determine repeatability. The validity and dependability of traditional outer hair cells performance were determined by analysing every distortion product frequency individually. The passing criteria were set 6-dB SNR. ABR testing was performed using IHS Jr. ABR Instrument. Three electrodes were placed on the vertex (non-inverted), ipsilateral mastoid (inverted), and contralateral mastoid (ground). The lay to rest conductor resistivity was set below 5kΩ. Clicks with 0.1 ms period were delivered in one ear through ER-3A insert earphones bestowed at a repetition rate of 31.1/second. Responses to 2048 clicks were preamplified and band pass between 100-3000 rates. The analysis time for the screen was set 12 millisecond. The conductor resistivity is often monitored. Recording was performed under sound proof conditions. Duplicate recordings were performed to ascertain dependability. ABR latencies for waves I, III, and V, as well as within the peak latencies (IPL) of waves I-III, III-V, and I-V, were measured.
Post-concussion tests were administered by a medical professional and the tests included were Post-Concussion Symptom Score (PCSS) and The Standardized Assessment of Concussion (SAC) respectively.
Post-Concussion Symptom Score: One of the most commonly used symptom evaluations. The PCSS consists of a battery of concussion-related symptoms (including headache, nausea, and vomiting) and a severity scale from 0-6 with zero being none and six being severe [6].
The Standardized Assessment of Concussion: This is a 5-10 minute paper and pencil check. It is an assessment tool developed to spot the results of gentle traumatic brain injury on the side line and does not require specific coaching in psychophysiology for administration or interpretation. This check assesses orientation, immediate recall, concentration, and delayed recall [7]. Performance on every element was summed for a complete attainable score of 30 with higher scores indicating higher functioning.
Otoscopic examination revealed a bilateral cone of light with no other abnormalities in the ear canal and tympanic membrane. Pure tone audiometry revealed Disclosed bilateral delicate to moderate sensorineural hearing impairment (Figure.1).
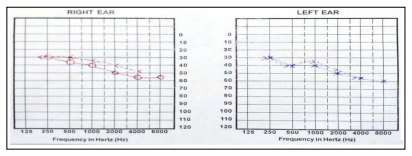
Figure 1: PTA findings
Speech Audiometry: SRT and SDS results are as follows (Figure.2)
| Ear | SRT | SDS |
|---|---|---|
| Right ear | 45dBHL | 85% |
| Left ear | 45dBHL | 85% |
Figure 2: speech audiometry results
Immittance and reflexometry revealed Bilateral ‘A’ type tympanogram with ipsilateral reflex present at 500Hz and 1000Hz and absent contralateral relexes suggestive of no middle ear pathology (Figure.3).
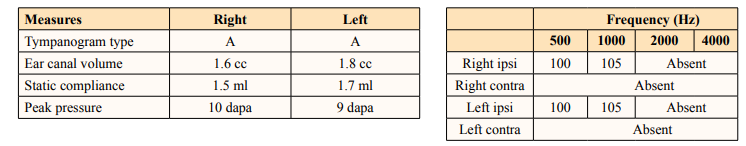
Figure 3: Immittance and Reflexometry results
Distortion product oto acoustic emission revealed bilateral absent oae’s suggestive of outer hair cell dysunction (Figure.4).
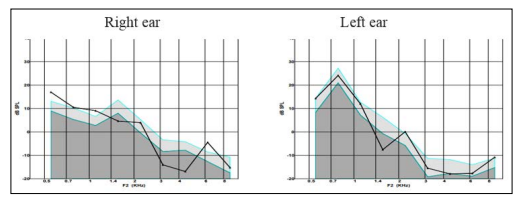
Figure 4: DPOAE findings of right ear and left ear respectively
Auditory brainstem responses revealed a bilateral clear and replicable Vth peak obtained untill 50 dBnHL which led to the impression of mild to moderate hearing loss (Figure.5). In addition, waves III and V within peak latenices I-V were prolonged in both ears
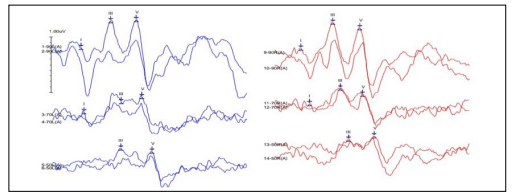
Figure 5: ABR waveforms of both right and left ears
i. Post-Concussion Symptom Score showed a Total PCSS score: 46 / 132 = 34.8 % which indicate presence of mild concussion symptoms.
ii. The standardized assessment of concussion showed an overall score of 20/30 (higher scores indicated better functioning).
Hearing loss typically occurs in conjunction with alternative invisible injuries, such as traumatic brain injury, or TBI. Hearing and balance problems are typically unmarked in polytrauma patients because of alternative visible wounds, which typically take medical priority. However, hearing disorders may mask or confuse the proper identification of alternative injuries. Given the interconnection between hearing disorders and alternative invisible injuries, understanding every condition is vital. An unknown case of hearing disorder interferes with the prognosis of patients with TBI. Factors related to each hearing disorder and TBI, such as attention, cognition, somatic cell loss, and noise toxicity, can cause misdiagnosis. Hearing disorders may exacerbate the social, emotional, and psychological symptoms of TBI. Additionally, in mild cases, customary neuroimaging is unlikely to search for structural brain injuries.
Audiological profiles of patients with TBI are rare. However, impairment could result from alterations in any part of the auditory pathway (external ear, middle ear, inner ear, nerves, trunk, neural structure, and plant tissue regions) in keeping with [8]. TBI causes a series of hearing losses that embody cochlear structural loss, proprioception alterations, and central auditory modifications.
In the current study, tone audiometry revealed bilateral, gentlemoderate sensorineural deafness. Evaluated hearing in sixty subjects with head injury and located out that on the kind of deafness, 8 cases(13.3%) has traditional hearing bilaterally, and thirty four cases(56.6%) of bilateral sensorineural, nine cases(15%) of bilateral or unilateral mixed, and three cases(5%) of unilateral semiconducting deafness were discovered [9]. Similarly, within their study conjointly reported that deafness when TBI occurs in the absence of bony injury seems to be a clinically vital but poorly characterised development [2].
Tympanometry results showed Bilateral ‘A’ type tympanogram with ipsilateral reflex present at 500Hz and 1000Hz and absent contralateral relexes suggestive of no middle ear pathology. The tympanometry results may vary depending on the type, site, and severity of the TBI insult.
DPOAE analysis unconcealed the bilateral absence of OAEs, and similar findings were seen in a very study by, who reported that if there was a delicate hearing disorder on PTA, there was an absence of emissions in 70 % at 1000 cycles per second, 69 % at 2000 cycles per second, 83 % at 4000 cycles per second [10]. They additionally advised that harm to the outer hair cells become more pronounced once there is a manifest hearing disorder on PTA.
ABR exposed mild to moderate hearing disorders with prolonged absolute latencies of waves III and V, as well as lay peak latencies of I-V in both ears. Reported similar findings in their study on 290 participants with TBI that showed positive associations between the severity of TBI and prolonged wave shape V and I-V interwave latencies [11]. The findings of their study indicate the involvement of the neural structure as a right away consequence of the severity.
The current study discovered that a participant with mTBI might experience sensory modality pathology within the peripheral and central sense modality systems, regardless of the quantity, type, and severity of TBI(s). Hence, it is important to receive a full audiological assessment post-TBI. This can be essential for designing interventions geared toward returning to activities of daily living, such as work, school, and leisure. Interventions can be tailored for every patient in keeping with the precise modality pathology, thereby increasing the probability of increasing the standard of life for patients with brain injury. Therefore, all patients with minor head injuries should undergo elaborate audiological analysis, even if they do not complain of hearing disorders.
I would like to thank the patient and his parents (especially his mother) for participating in this study and sharing their information and experiences.
The data that support the findings of this study are available upon request from the corresponding author; [N.A.K]. The data are not publicly available due to [restrictions such as containing information that could compromise the privacy of research participants.
Ethical approval was obtained from the Institutional Ethical Committee before conducting the study, and informed consent was obtained from the participant explaining all the procedures involved in this study.
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
N. A. K.: Study design, data collection, analysis and interpretation of results, and drafting of the manuscript. S.J.: Data collection, analysis, and interpretation of results.
The authors do not have any financial or her interests related to this study.
