Author(s): Ahmed Abdulhussein Kawen*
A new type of coronavirus family (SARS-CoV-2), that has been detected in individuals with several clinical symptoms named (COVID-19), was recognized as a pandemic on March 11, 2020. Numerous researches have been conducted on manifestations of skin disease related to COVID-19, i.e. rashes, pityriasis rosea (PR), vascular markings, and lesions as pimple-like.
A new type of coronavirus family (SARS-CoV-2) has been detected in individuals with several clinical symptoms. This virus was discovered in the late 2019 in China (Wuhan) and named (COVID-19). This virus has been spread throughout the whole world rapidly and was recognized as a pandemic on March 11, 2020 [1]. There are many research about the cutaneous findings of theCOVID-19 [2]. Numerous researches have been conducted on the manifestations of skin problems related to COVID-19, i.e. rashes, (PR) , vascular markings or lesions as pimple-like [3]. (PR) is a papulosquamous trouble described firstly by (Robert Willan) in 1798, but under another terminology [4]. (PR) is described by a skin eruption with initial popping spots and then followed along division dermatoses lines appearing as minimal, separate, oval to round lesions of skin on collarbone area. Such lesions influence chiefly proximal and trunk sides. Spontaneous remission typically takes place during rash appearance of 6-12 weeks. (PR) is thought to associate with viral infections, particularly human herpes virus (HHV) 7 [5].There were many names for (PR) as it was later named herpes maculosus and roseola annulet [6]. It surprises typically with huge erythematous scaly plaque evolution which is termed mother patch or herald patch on neck or trunk, then followed multiple secondary tiny erythematous scaly lesions rash predominantly located on the trunk and following split lines on back [7]. Since Corona Virus is closely related to (PR), we can predict the infection in the begining, as it is considered an early diagnostic sign. However, there is no evidence that the Corona virus is the cause of (PR) due to different types of rashes that appeared on the infected area[8]. It is very common. The incidence filed from 0.39 to 4.8 per 100 dermatology patient [5]. The etiology of (PR) is unknown; lesion histopathological alterations are nonspecific for (PR). They contain focal spongiosis caps, vascular dilation, infiltrates as perivascular lymphocytic and parakeratosis as patchy. These cytological changes are close to viral infections i.e., varicella zoster and herpes simplex [9]. The goal of the current work is to observe if Coronavirus is a risky factor in (PR) development where it might be considered as a trigger for other types of infection, including (PR). It can be considered a symptom of infection with the virus.
A case series descripting the dermatological finding of COVID-19 in Thi-Qar Governorate, collective samples in this study were gathered from inpatients, outpatients, emergency unites of Al Hussein Teaching Hospital, and inwards of Al-Shefaa’ Isolation Hospital; The study has been done over a four-month period (June-September, 2020.), in which a total number of 19 patients, 10 females and 9 males, is included. All cases were proved to have COVID-19 by positive post nasal or pharyngeal swab for PCR technique. A verbal consent was taken from each patient with a full description of the aim and benefit of the study. A skin lesion was firstly identified by a dermatologist: skin scraps were taken from the lesion of those who were infected with Covid-19 and diagnosed with histo-pathological changes. Even though they were nonspecific for (PR), they were highly suggestive. Most of the lesions contain focal spongiosis caps, vascular dilation, infiltrates as perivascular lymphocytic and parakeratosis as patchy. Samples were classified by internist into mild, moderate and sever cases of COVID-19 according to WHO criteria, and they were also categorized as typical and atypical according to (PR). Statistical analysis was done by using SPSS version. There were 26 describing cases according to their presentation regarding their mean age, gender, severity of COVID-19 and subtypes of (PR). ANOVA and Fischer Exact Tests had been used for cross-tabling to study the association of the variables of interest, P value <0.05 was of great significance
Nineteen patients in total (10 females, 9 males), who were infected with Coronavirus and were suffering from (PR), were included in this study in which the highest percentage of females was 52.6% and males 47.4%.

Figure 1: Distribution according to gender
Figure two demonstrates the distribution of patients according to the incidence of (PR) in typical and anomalous manner. The highest percentage was 77.9% for typical and 21.1% for abnormal.
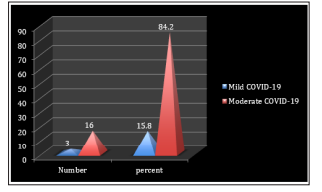
Figure 2: Distribution according to (PR) subtypes
The distribution of infected people was observed according to the COVID-19 sub-category. the highest percentage was in moderate COVID-19 (84.2%) while in mild COVID-19 it was ( 15.8%)
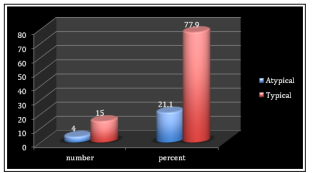
Figure 3: Distribution according to COVID-19 sub-category
Table 1 refers to the Mean age distribution according to gender in which there is no significant statistical difference while big statistical differences can be seen in P.Rosea and COVID-19 categories.
| Variables of interest | Mean | Std. Deviation | ANOVA, p value, Eta |
|---|---|---|---|
| Sex | .547 | ||
| Male | 26.2222 | 4.54911 | .470 |
| Female | 28.0000 | 5.77350 | .177 |
| P.Rosea | |||
| Typical | 28.1333 | 5.26263 | 2.792,0.113 |
| Atypical | 23.5000 | 2.88675 | .376 |
| COVID-19 severity | |||
| Mild | 27.0000 | 5.60952 | .090, 0.768 |
| Moderate | 28.0000 | 1.73205 | 0.073 |
| Total | 27.1579 | 5.16681 | |
| Sex | COVID | Total | Fischer Exact | |||
|---|---|---|---|---|---|---|
| Mild | Moderate | |||||
| Male | P.R Typical | No. % |
5 71.4% |
2 28.6% |
7 100.0% |
.735e .583 |
| Atypical | No. % |
2 100. 0% |
0 0.0% |
2 100.0% |
||
| Total | No. % |
7 77.8% |
2 22.2% |
9 100.0% |
||
| Female | P.R Typical | No. % |
8 100.0% |
0 0.0% |
8 100.0% |
4.444 .200 |
| Atypical | No. % |
1 50.0% |
1 50.0% |
2 100.0% |
||
| Total | No. % |
9 90% |
1 10.0% |
9 100.0% |
||
| Total | P.R Typical | No. % |
13 86.7% |
2 13..3% |
15 100.0% |
.323a .433 |
| Atypical | No. % |
3 75.0% |
1 25.0% |
4 100.0% |
||
| Total | No. % |
16 84.2% |
3 15.8% |
19 100.0% |
||
There are no significant statistical differences in the gender distribution for the subtypes of COVID-19 according to pit. Rosea subclass

Figure 4: Different presentations (PR)
Coronavirus disease has had several influences on dermatology practiced routinely [10]. It is obvious that we would witness development in this field and more accurate data would be collected about the relation between dermatology and COVID-19 in the coming days. Cutaneous symptoms might be classified under 5 chief groups: livedo and necrosis , lesions as urticarial, eruption being maculopapular, pseudo-chilblain, rash as vesicular [2] .At the moment, the skin diseases which accompany people with Coronavirus remain as unresolved mystery. In the current research, it was observed that the average PR patients, who have applied to outpatient dermatology clinic through the period of pandemic, augmented more times in the current year compared with last year at the same time. (PR) has been highly linked with people with Herpesvirus 6 and 7reactivation while other etiology such as viral, stress being psychological, vaccination, and drugs were involved as the reaction cause [11].
In many sources, it may be one of the factors leading to herpes viruses activation in which Corona viruses can be the cause of (PR) . Or perhaps another cause of stress and psychological pressure caused by the period of the epidemic[12]. In the previous study, it was shown that the rashes and skin diseases, associated with those who were infected with Corona virus, differed dramatically according to the geographical location[13]. In the previous research conducted by Enguix et.al,2020, when people with (PR) performed a Corona virus test using PCR, a positive result was obtained which is consistent with the current study. The coronavirus disease influences systems of multiple organ to pro-inflammatory chemokines and cytokines uncontrolled release, causing in manifestation clinically excluding symptoms of respiratory system [15]. This is the first study in Thi-Qar, Iraq that shows (PR) throughout the period of pandemic. We believe that such elevation is associated with HHV-6 reactivation. It is possible that (PR) is a symptom of the Coronavirus.
Coronavirus disease still remains as an unresolved mystery, however there are numerous publishing articles about the clinical symptoms and side effects. More studies are needed based on antibody Polymerase and PCR which should be implemented to search if specific dermatologic diseases are connected to cases of asymptomatic Covid-19 [16].There aren’t adequate studies so far in order to enable clinicians to recognize definite patterns of skin problems relating to Covid-19. Therefore, it is important to state these cases in order to increase the knowledge regarding such symptoms, particularly because they can be the only infection signs and confused with other viral infection and skin diseases. We also presume the importance of distinguishing between different mechanisms like physiological and temporal patterns; i.e. to underrated of whether there is a viral relationship of synergistic or symbiotic with other processes such as erythema, infection, herpes zoster and other skin diseases. Moreover, we highlight the importance of screening the precarious skin diseases in patients infected with Covid-19. More studies are needed to evaluate whether or not these lesions are associated with the virus. More accurate cutaneous manifestation of Covid-19 is required to increase presentation of these diseases as well as epidemiological knowledge. In the previous study conducted by Haha, it has been shown that being infected with (PR) have no relationship to people with Coronavirus. It is imperative for all healthcare professionals to be well-versed in such elevated manifestations of COVID-19. Surgeons should be also aware of such lesions, as they appear on feet, hands, and torso so often. Further COVID-19 standardized studies of rash are warranted for additional valid diagnosis and such visible endings utility [17].
(PR) infection increased during the COVID-19 outbreaks. This increase may be related to intense stress during the pandemic period or as a marker in COVID-19 patients. It is possible that altered immunity during the COVID-19 pandemic increased the frequency of (PR) infection. Moreover, we should keep in mind that (PR) infection may be accompanied by COVID-19. One limitation of the current work was the incapability for collecting standardized and complete sets of data to permit comparisons indepth among subgroups of rash. In a previous study conducted by Català et al., (2020), it showed that the infection with (PR) was related to the Coronavirus, as the percentage of patients reached 30%.In conclusion, a description of (PR) related to COVID-19 might help doctors approaching patients who have such disease and recognizing cases of little symptoms. Ehsani et al reported (PR) in a patient with COVID-19. A scaly annular rash over arms and trunk was observed in the twenty-seven-year-old man. The lesions were pruritic and spread over five days[19].
Mawhirt, et al.2020 confirmed that there is no relationship between COVID-19 and skin infections such as (PR). The reason of the appearance of (PR) spots might be just the activation of a specific virus relating to retrospective work. We did not have information about the individual’s quality of life, levels of anxiety, their treatments, and the risk of COVID-19. The current work is trying to understand the reason why patients with minor dermatological diseases visit hospitals while a worldwide fatal pandemic is occurring at the same time[21]. The rash of (PR) may be a direct result of virus-organ interaction or the result of an immune system activation [22].It is necessary to emphasize such patterns for clinical diagnosis. Furthermore, we suggest that researches should be enriched by conducting extra COVID-19 tests for diagnoses, as well as describing some collected markers and the clinical link between them.
The (PR) is one of dermatological finding related to COVID-19 that doesn’t have a clear role in its distribution according to the biography of the patient. It has not distributed significantly according to the severity of COVID-19. It might be triggered by COVID-19 and be completely cured with the clearance of disease.
More accurate cutaneous documentation of Covid-19 is required to increase presentation of these diseases as well as epidemiological knowledge.
