Author(s): Jard Evans Garcia and James Abraham Lee
Herein, we present a case of 12-year-old male with ocular features of Marfan Syndrome. This case is of a twelve-year-old Filipino male seen in our institution with a five-year history of blurred vision. Ocular examination revealed poor visual acuity, high myopia, and ectopia lentis. Systemic examination revealed pectus carinatum, hypermobile joints, and arachnodactyly. There was high suspicion for Marfan Syndrome and the patient was subsequently referred to Pediatrics for further evaluation and management, where diagnosis was confirmed. This report stresses that a multidisciplinary approach is essential in the management of Marfan syndrome to improve vision and prevent complications, both ocular and systemic, brought about by the disease process
Marfan Syndrome is an autosomal dominant disease with a highly variable systemic tissue disorder affecting the cardiovascular, musculoskeletal, and ocular system [1]. It is the second most common inherited connective tissue disorder with an estimated incidence of 1 in 5000 around the world [2]. The gene (FBN1) encoding the connective tissue protein fibrillin-1 is seen mutated in most patients with Marfan Syndrome. Fibrillin-1, a glycoprotein, is an important component of both elastic and non elastic tissues. It also contributes to the formation of microfibrils and the extracellular matrix [3].
There are a number of systemic signs and symptoms that may point in making the diagnosis of Marfan Syndrome. Cardinal features of Marfan Syndrome as stated in the Revised Ghent nosology include Aortic root dilatation/dissection and Ectopia lentis with a scoring system for systemic features. In this revised nosology, FBN1 testing, although not required, has greater significance in the diagnostic assessment [4].
Almost 50% of patients are diagnosed with Marfan syndrome primarily as part of the examination for visual complaints [5]. Common causes of ophthalmic problems in patients with Marfan syndrome are ectopia lentis, refractive error, amblyopia, retinal detachment, cataract, and glaucoma. Given this significance of the ocular signs of Marfan’s syndrome, we established to report the case of a twelve-year-old Filipino boy with Marfan’s syndrome who presented with biltateral ectopia lentis and high myopia.
This is a case of a 12-year-old male who came in to our institution with a five-year history of blurring of vision described as difficulty in reading letters in the classroom. Patient was initially seen at the general ophthalmology clinic where basic ophthalmologic examination was done. Visual acuity is 1/60 for the right eye and 3/60 for the left eye. Best corrected visual acuity is 6/15 for the right eye and 6/20 for the left eye with a refraction of -15.00 () -2.50 x180 and -14.00 () -1.50 x 180 for the right eye and left eye respectively. Anterior segment findings, color vision, pupillary exam, and ocular pressure were unremarkable. On a dilated pupil exam, the lens is displaced in the superotemporal location with visible zonular fibers in the inferior area (Figure 1).
On physical examination, patient is tall and thin with long extremities (Figure 2). The patient also had long fingers (arachnodactyly) and hypermobile joints (Figure 3). Patient also presented with pectus carinatum upon examination of the chest (Figure 4). The height of the patient was 165 cm while the arms’ length was 170 cm.
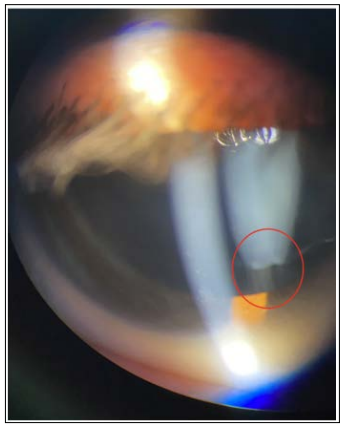
Figure 1: Displaced lens with visible zonular fibers
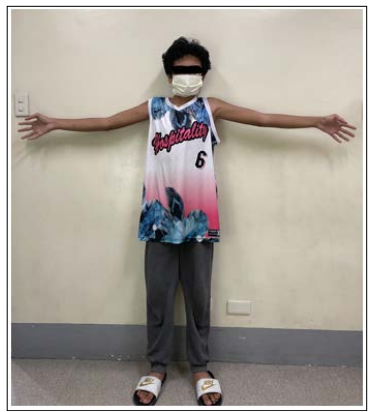
Figure 2: Full view of patient. Patient exhibits reduce elbow extension

Figure 3: Wrist and thumb sign
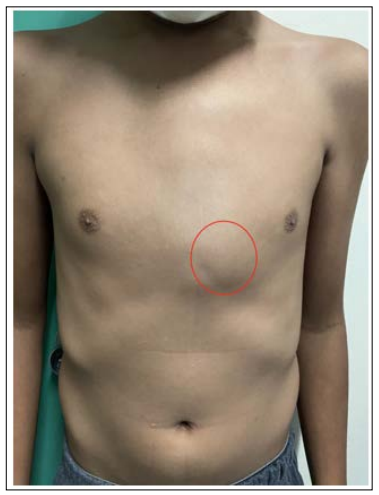
Figure 4: Pectus Carinatum
Patient was seen by Pedia-ophtha and Retina specialists with a diagnosis of Ectopia Lentis and High Myopia on both eyes. Management was to give refraction and annual ophthalmologic examination. Patient was also referred to Pediatric service for further evaluation and management and was requested to undergo cardio workup and genetic testing
Diagnosis of Marfan syndrome syndrome depends on a set of defined clinical criteria (Ghent nosology) to provide appropriate diagnosis of the syndrome and improve management. Cardinal features of the new diagnostic criteria include aortic root aneurysm and ectopia lentis. In the absence of one of these two cardinal features, the presence of an FBN1 mutation of positive systemic score is required (Figure 5) [4]. In our patient, due to the pending genetic and cardiology work up, the presence of ectopia lentis and a systemic score of 7 was attributed in making the diagnosis of Marfan Syndrome.
The most common ocular complication of Marfan syndrome is Ectopia Lentis. Abnormalities in fibrillin lead to zonular weakness with subsequent lens subluxation [7]. In this case, the subluxation occurred in the superotemporal direction which is frequently seen in Marfan patients. Visual symptom and treatment of ectopia lentis depends on the severity of lens malposition. Prescribing spectacles are the first step to improve the blurred vision secondary to subluxated lens [6]. In this patient, a conservative approach was done since it achieved a good corrected visual acuity. Indications for lens extraction are inability to achieve good corrected visual acuity, risk of amblyopia in children, posterior dislocation of the lens into the vitreous cavity, anterior dislocation of the lens with or without secondary glaucoma, impending to complete lens dislocation, lens induced glaucoma or uveitis, and cataract [7].
Amblyopia should also be monitored as Marfan patients at high risk due to the various ocular abnormalities. Romano et al, monitored the visual outcome of patients who had non-surgical treatment with hereditary ectopia lentis [8]. They concluded that early surgical intervention should be considered with patients who are nonresponsive to conservative management as almost half developed significant permanent functional amblyopia [9].
Peripheral retinal changes in Marfan Syndrome include myopic degeneration, lattice degeneration, atrophic holes, chorioretinal pigment proliferation, peripheral vitreous traction syndromes, and retinal breaks [7]. Due to these changes, they are at high risk of retinal detachment. For this case, patient was advised for a complete ophthalmologic examination once a year or earlier if with new ophthalmic complaint.
A case of Marfan syndrome with bilateral ectopia lentis and high myopia with musculoskeletal and chest deformities was presented. Ophthalmologists play an important role in the diagnosis of Marfan Syndrome due to the ocular signs and symptoms. Patients should be evaluated with repeated refraction, monitoring of ectopia lentis, peripheral retinal status, and amblyopia. A multidisciplinary approach is needed for monitoring and managing patients as to prevent visual loss and life-threatening complications.
