Author(s): Sharath Reddy Annam*, Anil Krishna, Vaibhavi Polavarapu, Bhavan Prasad A and Hansika Sharma
Chronic total occlusion intervention of ostial left anterior descending artery lesion without clear cap poses challenges for wiring. Intravascular ultrasound guided antegrade cap puncture and guide extension assisted reverse controlled antegrade and retrograde tracking away from ostium would minimize inflow injuries. This case report explores inflow injury and its detection by imaging in ostial LAD CTO PCI.
CTO intervention of ostial LAD/LCX lesions without clear cap poses challenges for wiring due to angle of entry and unclear entry. Ostial LAD CTO, by being in a location supplying significant portion of myocardium, increases the risk of PCI due to inflow injuries like LMCA dissections or Intramural hematoma (IMH) [1]. In one of the large-scale analysis of ostial LAD CTO PCI in 13 centers of Korea, it was observed that cap is ambiguous in 43% of cases and apparent dissections requiring rescue procedures were noted in 5.2% cases [2]. Ostial LAD CTO is a different animal to tame due to the special operator attention needed to prevent intraprocedural catastrophes like dissection or IMH of LMCA or LCX [3]. IVUS guided cap puncture followed by using this wire position for antegrade preparation to receive the retrograde wire beyond the ostium of LAD minimizes aforementioned complications and makes procedure as predictable as possible[4]. We report a case of ostial LAD CTO intervention in which LMCA intramural hematoma complicated the stenting strategy
60 - year- old male hypertensive, diabetic treated for acute ST elevation Inferior wall myocardial infraction (IWMI) with primary angioplasty with stent to mid RCA fig 1A, 1B, 1C.
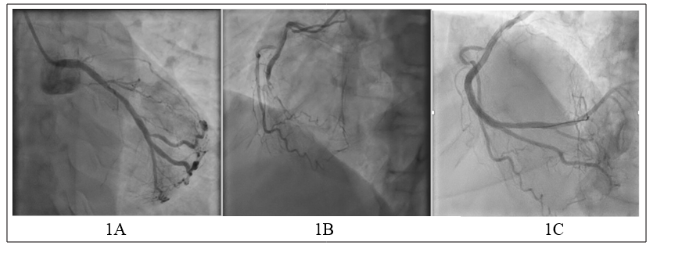
Figure 1A - 1C: (A) RCA angiogram before primary PCI - Total thrombotic occlusion of mid RCA, (B) Left system - Ostial LAD chronic total occlusion with mild LCX disease, (C) Post Primary PCI to RCA - Dominant RCA with normal distal branches.
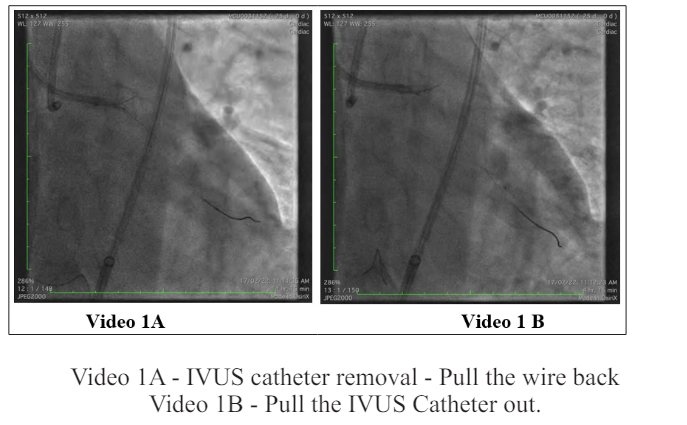
Admitted for ostial LAD CTO PCI. As the proximal cap was not clear IVUS guided antegrade cap puncture was planned followed by retrograde if needed. IVUS guided antegrade cap puncture was done using double lumen catheter (Crusade, Kaneka Corporations, Japan) and IVUS catheter (Opticross, Boston scientific) on the same work horse wire through 8 FR guide (fig 2A). Initial cap puncture with Hornet 10 (Boston scientific) was sub intimal (fig 2B), however, in subsequent attempt wire could be navigated into proximal cap successfully (fig 2C). Work horse wire on which Opticross is positioned into LCX was pulled back till the tip of the wire was out of the IVUS catheter monorail exit. Then, IVUS catheter was withdrawn (video 1A & 1B) followed by double lumen catheter exchanged to corsair XS (Asahi Intecc) (fig 2D) on LAD wire into and beyond the ostium of LAD to consolidate the position achieved.
Antegrade wire de-escalated to GAIA II (Asahi Intecc) and advanced further but halted because of ambiguous vessel course in retrograde injection. Retrograde wiring through septal collateral was done with caravel 150 mm (Asahi Intech) through the guide extension in 7 FR JR guide. After caravel positioned into the LAD contrast injected through it to delineate course of LAD for further wiring (video 2A). To our surprise, contrast injection created subintimal dissection with retrograde extension to ostial LAD. Conventional reverse cart (Video 2B) with 3.5 x 12 mm balloon over GAIA II in the ostial LAD and hornet 10 retrograde wire was done successfully followed by confirmation of intimal wire entry from LAD into LMCA by IVUS (Video 2C). After externalization pre-dilatation of lesion was performed followed by antegrade wiring of distal LAD through the double lumen catheter on the externalized wire. Retrograde wire is removed followed by IVUS imaging done from LAD for stenting strategy. IVUS revealed IMH (fig 2E) extending into distal LMCA. Stenting done from ostial LMCA into LAD with 2.75x38 mm & 3.5x28 mm stent with overlap at no branch zone of proximal LAD. After POT for LMCA and optimization of LAD stent by post dilatation, IVUS from LCX revealed MLA of 2.3 mm2 against the base line of 5.6 mm2 (fig 2F, 2G). TAP stenting done with 3.0 x 28 mm stent into LCX followed by bifurcation optimization (fig 2H).
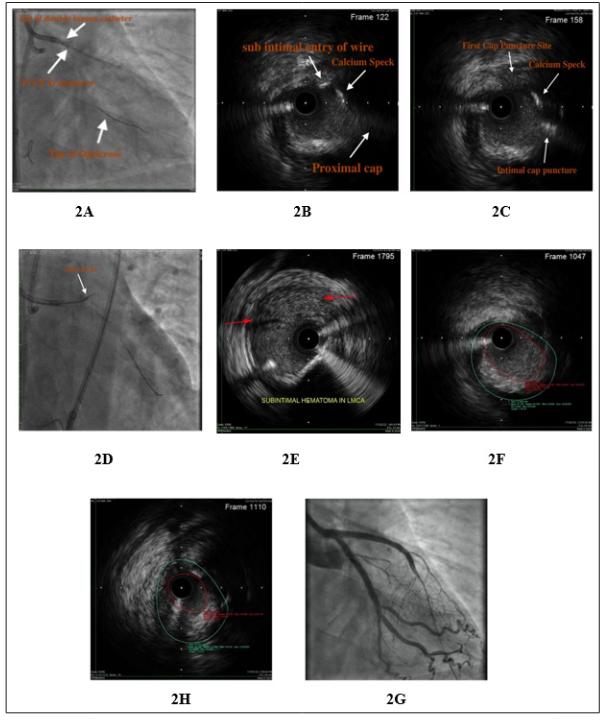
Figure 2A - 2H: (A) IVUS guided cap puncture - IVUS catheter, (B) IVUS showing antegrade wire entry at sub intimal plane away from cap, (C) IVUS - HORNET 10 in proximal cap, (D) Fluro - HORNET 10 in proximal cap, (E) IVUS - Intramural hematoma compressing true lumen, (F) Ostial LCX MLA in IVUS before LM TO LAD stent (MLA: 5-6 mm2), (G) Ostial LCX MLA after LMCA to LAD stent followed by POT (MLA: 2-3 mm2), (H) Final angiogram result.
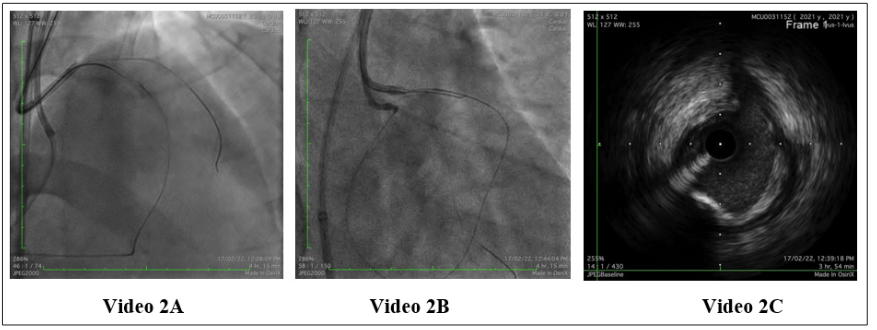
Video 2A - Check for wire positioning
Video 2B - Reverse CART with retrograde wire and 3 mm balloon - HORNET - 10 after failed re-entry with GAIA - 2, 3
Video 2C - IVUS confirm retrograde wire entry
Ostial LAD CTO poses challenges due to abnormal angle of attack with the antegrade wire. Furthermore, presence of ambiguous cap, seen in 43.3 % of cases in Korean data, amplifies the technical challenges for antegrade wiring [2]. Graphic 3 A, B, C illustrates the ideal wiring strategy for ostial LAD CTO with ambiguous cap to minimize inflow injury.
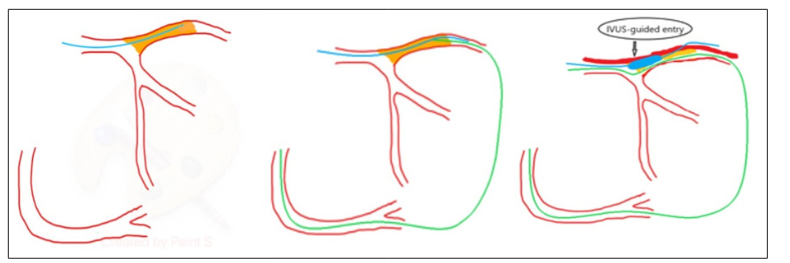
Figure 3A - 3C: Steps for Ostial Lad Cto Pci with Ambiguous Cap
(3A) Step 1 - IVUS guided cap puncture, (3B) Step 2 - Going Retrograde, (3C) Step 3 - Reverse CART, beyond the ostium with
guide extension.
Indeed, same Korean study showed 5.2% incidence of inflow dissections requiring stenting of LMCA or LCX2. Understandably, Inflow vessel injury/dissection was more frequent in patients with LMCA disease or ambiguous proximal cap. The presence of both anatomic factors would have additive impact on the incidence of dissection. Other factors in antegrade wiring which might affect inflow injury are angle of attack, type and shape of the wire used, type of microcatheter and use of imaging. Increasing angle of attack, attempting ambiguous cap puncture without imaging and microcatheter positioned away from the proximal cap increases the chances of dissection [5]. Double lumen catheter with live IVUS would increase the accuracy of targeted cap puncture with lesser chances of inflow injury. Antegrade Preparation with complete IVUS guided cap puncture is considered Achilles heel of ostial LAD CTO [3]. After antegrade cap puncture under IVUS, wire position achieved must be consolidated by advancing microcatheter into and beyond the ostial LAD. In the event of failure of antegrade wire reaching the distal true lumen, parallel wire with the double lumen catheter positioned into the LAD in such a way that second wire also goes through the same ostial LAD entry or retrograde wiring can be used. When retrograde wiring is used reverse CART should be performed beyond the ostial LAD, preferably, with guide extension assistance to make sure retrograde wire enters LMCA through the antegrade entry created under IVUS. Caution should be taken to stay distal and away from LAD ostium with retrograde wire during reverse CART.
Directed reverse CART with retrograde wire directed onto distal tip of antegrade balloon would minimize the proximal LAD injury in presence of shorter length of antegrade space created. If guide extension can’t be used intimal entry of retrograde wire into LMCA should be confirmed by IVUS before externalization. In situations of retrograde wiring without antegrade preparation, retrograde wire navigation into LMCA must be done under IVUS for ideal entry in to LMCA without creating inflow injury. In a rare situation, when a high tip-load guidewire is needed to puncture the proximal cap retrogradely but is less controllable (either by poor microcatheter support or severe vessel angulation), elective stenting from the LMCA to the LCX may facilitate direct wiring while ensuring the safety. However, this strategy should be justified by other indications for LMCA - LCX stenting, such as the presence of LMCA disease or ostial LCX disease [2]. Inflow injury is mostly noticed after CTO wiring but sometimes can be seen after predilation of ostial LAD. Therefore, LMCA anatomy must be analyzed carefully by IVUS from LAD and/or LCX after the lesion preparation before embarking on stenting strategy. Any inflow dissection or intramural hematoma extending into LMCA warrant’s two stent strategy. Consider placing LMCA stent from ostium to avoid proximal lumen compromise by IMH shift.
Ostial LAD CTO PCI constitutes a special subset due to larger area of myocardium at risk. Careful wiring both antegrade & retrograde to prevent inflow injuries, and meticulous analysis of LMCA anatomy in IVUS to identify inflow injuries before embarking on stenting strategy are quintessential to prevent catastrophe.
The authors have nothing to disclose
The authors have no financial disclosure
I would like to acknowledge Dr. Chandana for drafting the manuscript and submitted to journal.
