Author(s): Aliyu S and Ningi AB*
Extra-hepatic billiary obstruction is a common disorder seen in surgical practice, and it greatly affects the quality of life of patients afflicted with such disorder. In its severe form, it may be life threatening due to complications such as, hepatic encephalopathy, Hepato-renal syndrome, fulminant cholangitis and jaundice related coagulopathy. Obstructive Jaundice is the most common presentation following extra-hepatic billiary obstruction and carcinoma of the head of the pancreas and choledocholithiasis are the most common malignant and benign causes. Most patients present with advanced disease where palliation is the only viable option. However, such patients may not be suitable for surgery under General Anaesthesia due to advanced age, poor nutritional state with hypolbuminaemia, extra-abdominal metastasis producing respiratory compromise or a high risk for hepatic encephalopathy.
Objectives: We aim to assess the safety and effectiveness of a palliative Cholecysto-Jejunostomy done under local Anaesthesia.
Methods: This is a prospective cross-sectional study of total of 54 patients, both males and females, aged 16 years and above, who presented at the General Surgery units of State Specialist Hospital Damaturu and General Hospital Potiskum, both in Yobe State Nigeria; with Obstructive Jaundice. All had clinical and Radiological evidence of extra-hepatic Billiary obstruction and were managed surgically with a palliative Cholecysto-Jejunostomy under local Anaesthesia involving infiltrative cutaneous field block and USS guided Oblique Subcostal Transversus Abdominis Plain Block (OSTAPB). It is a 6-year study done from January 2015-December 2020. Informed consent was obtained from all patients according to Helsinki guidelines and Ethical clearance was granted by the leadership of both hospitals. All data were analysed with SPSS 20.0 software for correlation of outcomes.
Results: The study population were 54 patients, 59.3% males and 40.7% females. The mean age is 50.5 years and an age range of 16-75 years. Malignant lesion is the most common cause of extra-hepatic billiary obstruction, with exocrine pancreatic cancer responsible for 48.1% of all causes. Chronic pancreatitis (16.7%) and impacted common bile duct (CBD) stones at 14.8%, are the two most common benign causes. All the patients had an abdominal USS for diagnosis or non-contrast enhanced abdominal CT Scan if there is ambiguity. A total of 77.8% had palliative Cholecysto-Jejunostomy done under local Anaesthesia involving cutaneous field block with Lignocaine with Adrenaline at a standardised dose of 4mg/kg body weight and USS guided Subcostal TAP Block. The remaining had a palliative Cholecystostomy or no surgery done. All abandoned cases were because of an involved or fibrosed Gallbladder. The most common post-operative complications are Surgical Site Infection (SSI) at 24.1%, excessive Primary Haemorrhage and reactionary haemorrhage, at 9.3% each. The total fatality rate was 7.4%.
Conclusion: Palliative Cholecysto-Jejunostomy is safe, operative mortality rate is 7.4% and is effective in providing billiary drainage with limited post-operative morbidity.
Pancreatic head cancer and peri-ampullary cancer are the most common malignant causes of extra-hepatic billiary obstruction globally [1]. Despite advances in the management of pancreatic cancers, survival remains poor and late presentation is the norm [2]. It was estimated that about 80% of patients with pancreatic cancers are not eligible for curative treatment, with palliative treatment as the mainstay of care [2]. Most palliative treatments are aimed at relieving obstructive jaundice, gastric outlet obstruction and pain. Pruritus, one of the most troubling symptoms seen in obstructive Jaundice can be relieved through an effective biliary drainage. The relief of jaundice and other symptoms of extrahepatic billiary obstruction improves quality of life and may even enhance the life expectancy of patients with unresectable malignant biliary obstruction [3]. Biliary drainage techniques have evolved over time, from open internal by-pass to endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous transhepatic biliary drainage [4,5]. For the palliation of obstructive jaundice, a biliary bypass should be selectively done for the relatively fit patients. A surgical biliary bypass, in comparison to endoscopic stenting, provides an effective drainage and a potent long-term prevention of biliary obstruction [6]. Endoscopic stenting is however, preferred in patients with a relatively short life expectancy (<6 months). Such Surgical drainage should preferably be by a Choledocho-jejunostomy or Cholecysto-jejunostomy [7]. A gastric bypass is often done at the same sitting to prevent gastric outlet obstruction due to tumour infiltration of the C-loop of the duodenum or due to extrinsic compression [7]. Newer methods of by-pass of gastric outlet obstruction are routinely used, such as endoscopic duodenal stenting and open/laparoscopic gastroenterostomy. The benefits of these procedures are however being questioned, as the patients do not live long enough to require them and their effect is yet to be validated in controlled trials [8,9]
Giant strides have been made in the Western world in the management of extra-hepatic billiary obstruction. Pereires and Burchart in 1978 pioneered internal billiary drainage using stents and since then open surgery is no longer the preferred method of drainage in the West [10]. The percutaneous transhepatic route was successfully used for internal drainage of the billiary channels using small calibre endo-prostheses. The introduction of the wider, larger calibre stents that can be endoscopically placed safely has reduced the complication rates of the stent drainage [10]. Despite improvement in structure, the use of endo-prostheses for billiary drainage is still bedevilled with stent migration and occlusion [11]. Several Randomised Controlled Trials have compared the two palliative billiary drainage procedures: surgical bypass and biliary stenting for malignant extra-hepatic obstructive jaundice [12-15]. Either a percutaneous transhepatic or endoscopic stenting was used [12]. Both the operative and the non-operative billiary drainage procedures were found to be optimally effective [12-15]. Non-operative biliary stenting is however, associated with lower operative mortality and a shorter duration of hospital stay. Some argued that there is no much difference in the cumulative days of hospitalisation, because, those with stents left in situ often require re-admissions for stent occlusion [16]. What has remained consistent is the 30-day mortality rate. It is higher for surgical by-pass, placed between 15%- 24% [16].
In Nigeria, as high as 82.4% of patients with malignancy present late, with symptomatic obstruction of hollow viscera that will require palliative relief of the obstruction [17]. The use of less invasive techniques such as endoscopic or image guided percutaneous placement of endoluminal stents, laser channelisation, and use radiotherapy are often not feasible. It is either these techniques are not readily available or there is no requisite expertise to undertake them [17]. The Surgeon is often left with no option but the surgical by-pass for the relief of billiary obstruction [17]. Even in Africa though, the surgical by-pass should be for patients expected to live longer than 6 months [16]. The inherent advantage for the surgical by-pass is the reduced procedure-related late morbidity. It has been reported that the morbidity rate for patients with an endoprosthesis in situ is 61%, compared to 5% for those with a surgical bypass [10]. Recurrence of jaundice post-procedure is also higher for patients with stents at 20%-50%, than those with surgical bypass at 1%-15% [10].
Biliary drainage by Cholecysto-jejunostomy is not fail-proof. The anastomotic stump may occlude from tumour involvement of the cystic duct in cases of Cholangiocarcinoma [10]. The comparison of Cholecysto-jejunostomy with Choledocho-jejunostomy for biliary bypass has been done in many controlled trials [18,19,20].
Choledocho-jejunostomy has been reported to provide better drainage and fewer operative morbidities such as, billiary leak, post-procedure cholangitis and recurrence of jaundice due to obstruction [21]. Cholecysto-jejunostomy is however, the most preferred surgical by-pass by many surgeons. Because, it can be quickly done without need for dissection of the extrahepatic biliary tree [18,19,20]. This is the preferred method of palliative billiary drainage for most African Surgeons also [17]. A Surgical bypass is contraindicated in the presence of the following: multiple liver metastases, a hepatoma, or a carcinoma of the gall- bladder. Also, when the tumour involves the gall-bladder or porta hepatis or when there’s an advanced tumour of the stomach, or colon, etc. These are considered indicators of inoperability [19,20].
The greatest challenge for the African Surgeon is in choosing the right patient for such surgical procedure. The patients’ suitability for the surgery is to be determined by the expertise of the Surgeon, available equipment for anaesthesia and the surgery, the patient’s physiologic fitness for surgery and anaesthesia; and expected benefit to be achieved from the surgery [21,22]. Obstructive Jaundice often results in Cholestatic liver diseases, which are marked by increased formation of hepatotoxic substances, mitochondrial damage and a significant dysfunction of liver antioxidant mechanism. The hepatotoxicity is said to result from intra-hepatic accumulation of insoluble bile acids with an attendant effect of cellular dysfunctions, such as the mitochondrial energy production failure. Both mitochondrial metabolism impairment and hydrophobic bile acids accumulation are associated with increased production of oxygen free radical species and development of oxidative damage [23]. These pathophysiologic changes make the administration of General Anaesthesia hazardous to the patients. The increased levels of circulating direct bilirubin are known to result in decreased cardiac contractility, reduced left ventricular pressure, Impaired response to beta agonist drugs and decreased peripheral vascular resistance. It also causes bradycardia, due to direct effect of bile salts on the SA node resulting in a Hypotensive patient with exaggerated hypotensive response to bleeding; who is prone to postoperative shock following administration of General Anaesthetic agents [24,25].
This observation prompted our interest in performing these palliative surgeries under Local Anaesthesia, especially in our sub-optimal hospitals where the full armamentarium of a General Anaesthesia and Peri-operative resuscitation is inadequate, as is the practice in most developing countries [26,27].
This is a non-randomised, non-controlled clinical trial of 54 patients admitted in to the General Surgery Units of State Specialist Hospital Damaturu and General Hospital Potiskum, both in Yobe state Nigeria; with clinical and Radiological diagnosis of Obstructive Jaundice secondary to extra-hepatic billiary tree obstruction. All the patients are adult males and females, aged 16 years and above. Clinical symptoms of a progressive or intermittent jaundice associated with pruritus, passage of dark coloured urine, pale, bulky, foul smelling stool that floats in the lavatory or is difficult to flush, are taken as proof of an extra-hepatic obstructive jaundice. The presence of weight loss, abdominal mass, pain radiating to the back, worse with lying supine and progressively deepening jaundice was considered to be suggestive of pancreatic head cancer. Deep jaundice (with a greenish hue) with fluctuating intensity, occasional Melena or passage of Aluminium paste stool was considered to be due to a peri ampullary cancer. A palpably enlarged gall bladder is the most important clinical criteria for inclusion. The exclusion criteria are patients with WHO/ECOG performance status of 4, those with multiple liver metastases, a hepatoma, or a carcinoma of the gall- bladder. The presence of tumour involvement of the gall-bladder or porta hepatis, a fibrosed gallbladder or when there’s a malignant ascites or carcinomatosis peritonei are also reasons for exclusion.
A Urinalysis for absence of Urobilinogen, Liver function Test for evidence of increase in both total and direct bilirubin, Serum Blood sugar measurement to rule out new onset Diabetes Mellitus and a Clotting profile for deranged INR and deficiency of Vitamin K dependent clotting factors were done for all patients. All patients had an abdominal USS for diagnosis and a confirmatory noncontrast-enhanced abdominal CT Scan where there is doubt. Special measures are taken in all the patients undergoing surgery to mitigate these specific risks: infections (cholangitis, septicaemia, wound infections), bleeding (non-coagulant acarboxyl derivatives of vitamin K dependent factors), Hepato-renal failure, hepatic encephalopathy, fluid and electrolyte abnormalities. All the participants gave informed consent and additional consent was sought from few to take their pictures with the faces showing to demonstrate the state of wakefulness (Figure 8).
All patients were admitted in to the ward 24 hours prior to the surgery day, a venous access secured and a urethral catheter passed for monitoring urine out-put. They are given glucose rich intravenous fluids, at least 4 litres/24 hours, to deliver 200g of glucose/day. Intramuscular injection of Vitamin K1 at 10mg daily for 5 days for all those with deranged INR. An INR of 1.3 is the minimum requirement for surgery. All were given a prophylactic dose of a third generation cephalosporin, 1g of Rocephin. Oral lactulose at 30-50 ml four times a day was given. Sedatives like benzodiazepines and opioids were avoided.
An infiltrative cutaneous field block is initially done over the right subcostal region, covering a 20cm wide radius using Lignocaine with adrenaline at a standardised dose of 4mg/kg, made up to 40mls with normal saline. A total of 20mls is used for infiltrating the skin and the subcutaneous tissue using 10 ml syringe with 27G needle and the remaining 20mls for infiltrating in-between the external and internal oblique muscles to achieve the field block. A USS guided Oblique Subcostal Transversus Abdominis Plain Block was done using a 5MHz Ultrasound probe. A full resuscitation tray is kept available and patient monitoring is done using pulse oximetry and manual Blood Pressure measurement. Antiseptic skin preparation is achieved with initial 2% Chlorhexidine cleaning followed by 10% povidone iodine painting. A high-concentration, low-volume technique of analgesia was used using a short bevel (30o) block needle (50 - 100 mm) over a 20 ml syringe and 0.25% Levobupivacaine is used at a standardised dose of 0.3-0.6 ml/kg. The plane of block between the rectus abdominis and transversus abdominis was confirmed using hydro dissection technique as described by Hebbard. Patients are placed in supine position with a slight left-lateral tilt, operative field preparation and draping is as it is done under general anaesthesia. The procedure is started after a sensory test using a toothed-dissecting forceps and the remaining operative steps are as outlined in standard operative texts for Cholecysto-Jejunostomy under general anaesthesia except for choosing jejunal length to site the side-side anastomosis. The first small bowel loop delivered through the operative wound is used for anastomosis to reduce unnecessary drag on the jejunal loop and minimise atmospheric exposure. Continuous communication is kept with the patient throughout the procedure and patients are asked to rate intra-operative pain on a numerical rating scale (NRS) of 2-10. Only ten of the patients required a salvage dose of weak opioid analgesia and anxiolytics due to agitation. The average time of the procedure is 30-45 minutes, with two cases extending to one hour due to excessive primary haemorrhage. The average intra-operative pain score using the NRS was 2-4. They are postoperatively placed on nil per oral, intravenous fluids, analgesia and antibiotics.
All patients were kept in the ward under close monitoring for 48 hours and were asked to grade their right hypochondriac pain using NRS. Pulse rate, blood pressure and oxygen saturation were monitored using oximetry. Patients were discharged home after an uneventful postoperative recovery and a full return of bowel function. They are advised to report to the emergency room (ER) if they notice: an increasing or spreading abdominal pain, postural dizziness, bleeding from the incision site, progressive abdominal distension or fever. These may herald a significant secondary haemorrhage or billiary peritonitis.
A total of 54 patients were recruited for the study, 59.3% were males and 40.7% were females, a male-female ratio of 1.5-1. The mean age is 50.5 years and an age range of 16-75 years. Malignant lesion is the most common cause of extra-hepatic billiary obstruction, with exocrine pancreatic head cancer and periampullary carcinoma responsible for 48.1% of all causes. Chronic pancreatitis (16.7%) and impacted common bile duct (CBD) stones at 14.8%, are the two most common benign causes. Cholangiocarcinoma (5.6%) and obstructing primary duodenal cancers (9.3%) are rare (Table 1).
Table 1: Showing Distribution of Causes of Obstructive Jaundice| Diagnosis | Frequency | Percent |
|---|---|---|
| pancreatic head cancer | 12 | 22.2 |
| periampullary carcinoma | 14 | 25.9 |
| chronic pancreatitis | 9 | 16.7 |
| duodenal cancer | 5 | 9.3 |
| CBD stone | 8 | 14.8 |
| cholangiocarcinoma | 3 | 5.6 |
| gastro-duodenal TB | 3 | 5.6 |
| Total | 54 | 100.0 |
A total of 77.8% had palliative Cholecysto-Jejunostomy, 20.9% had a palliative Cholecystostomy and 1.9% had no surgery done. The abandoned case was because of an involved and fibrosed Gallbladder (Figure 1). All surgeries were done under local Anaesthesia involving cutaneous field block with Lignocaine with Adrenaline at a standardised dose of 4mg/kg body weight and USS guided Subcostal TAP Block using 0.25% Levobupivacaine at a standardised dose of 0.3-0.6 ml/kg. The average time of the procedure is 30-45 minutes, with two cases extending to one hour due to excessive primary haemorrhage. The average intra-operative pain score using the NRS was 2-4. Only ten of the patients required a salvage dose of weak opioid analgesia (pentazocine) and anxiolytics (midazolam) due to agitation. No anaesthesia related complications were recorded. Intraoperative pictures showing the operative procedures were taken (FIGURE 2-8). The most common post-operative complications are Surgical Site Infection (SSI) at 24.1%, excessive Primary Haemorrhage and reactionary haemorrhage, at 9.3% each. Billiary leak and bile peritonitis occurred at 7.4% and 1.9% respectively. No recorded cases of recurrent jaundice or subsequent Gastric Outlet Obstruction were seen. The average hospital stay was 6-7 days. The total fatality rate was 7.4% (Table 2)
Table 2: Showing the Distribution of Postoperative Complications| Complications | Frequency | Percent |
|---|---|---|
| primary haemorrhage | 5 | 9.3 |
| secondary haemorrhage | 5 | 9.3 |
| billiary peritonitis | 1 | 1.9 |
| billiary fistula | 4 | 7.4 |
| wound infection | 13 | 24.1 |
| death | 4 | 7.4 |
| NONE | 21 | 38.9 |
| OTHERS | 1 | 1.9 |
| Total | 54 | 100.0 |
The management of pancreatic carcinoma is quite tasking even in the best of centres. Presentation has been mostly late, diagnosis is often missed, because, most of the symptoms are vague initially; or mimic other common upper gastrointestinal diseases. Most patients benefit from palliative care, especially, in developing countries, where there are no robust screening programmes for early detection and diagnosis. Although a relatively infrequent tumour, it is increasingly seen worldwide now, considered the fifth leading cause of cancer death in the West [28]. Out of the 54 patients that were recruited for the study, 59.3% were males and 40.7% were females, giving a male-female ratio of 1.5-1. This is similar to reports from the Western world where the male to female ratio is also 1.5:1 and it is postulated that increase in cigarette smoking habits among women is responsible for the rise in the female-related incidence [16]. Its incidence increases sharply after the age of 45 years [29]. The mean age in our study is 50.5 years with an age range of 16-75 years. Perhaps, because we studied all causes of extra-hepatic billiary obstruction, made up of gamut of pathologies, both benign and malignant. Almost in half of the cases, the extra-hepatic billiary obstruction results from pancreatic head and periampullary carcinomata [Table 1]. This is similar to reports from other developing countries of the Indian subcontinent and South-East Asia, e.g. Nadkarni, Kar et al and Phillipo Chalya et al [30-32]. Reports from the SouthWestern part of Nigeria are also similar [33]. This is in stark contrast to other studies that reported benign causes as the most common [34,35]. The benign causes are quite varied, chronic pancreatitis and common bile duct stones are however, the most reported in our study [Table 1]. All the benign causes often result in a billiary stricture and there is a major difference between the developed and developing nations in the causes of the stricture [36]. The most common cause of benign billiary strictures in the West is iatrogenic injury - following operations on the gallbladder and the biliary tree. laparoscopic cholecystectomy, the most common cause in the West, initially resulted in an increase in operative trauma to the bile ducts from an incidence of 0.1-0.2% to 2%. The steep learning curve of laparoscopic procedures was initially accused, but, despite widespread adoption of laparoscopic cholecystectomy, the incidence of operative trauma still remains higher than that of an open cholecystectomy at 0.2-0.7% [36]. The Non iatrogenic causes of benign strictures are the most prevalent in developing countries, and these include inflammatory conditions and subsequent fibrosis related to chronic pancreatitis, cholelithiasis, choledocholithiasis, sclerosing cholangitis, stenosis of the sphincter of Oddi, or infections of the biliary tract [36].
Majority of the patients present with an already advanced and unresectable disease carrying a dismal prognosis with palliation being the only option available. Palliation involves relief of the extra-hepatic obstruction for the alleviation of pain, cholangitis, and pruritus or in some patients to prepare them for chemotherapy or intrabiliary brachytherapy [37,38]. A surgical biliary bypass, in comparison to endoscopic stenting, provides an effective drainage and a potent long-term prevention of biliary obstruction [6]. Endoscopic stenting is however, preferred in patients with a relatively short life expectancy (<6 months). Such Surgical drainage should preferably be by a Choledocho-jejunostomy or Cholecysto-jejunostomy [7]. These palliative measures do not only prolong longevity but also improve the quality of life, and is responsible for their wide acceptance [39]. In this study, a total of 77.8% had palliative Cholecysto-Jejunostomy, 20.9% had a palliative Cholecystostomy and 1.9% had no surgery done. The abandoned case was because of an involved and fibrosed Gallbladder (Figure 1).
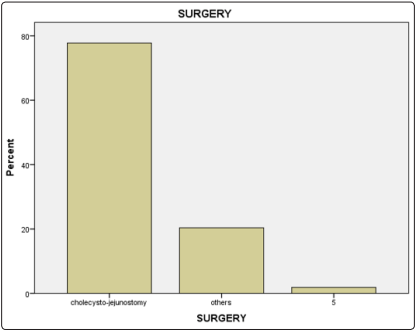
Figure 1: Showing the Distribution of Surgeries Performed
The improvement of endoscopic drainage procedures in the West has significantly reduced the role of surgical bypass, because of its associated higher morbidity and mortality. Surgical bypass is however the procedure of choice in patients with unresectable disease, those with gastric outlet obstruction and in those whose life expectancy is less than six months [40-44]. Comparison of surgical bypass with endoscopic stenting by several Randomised Controlled Trials (RCT) has found no significant difference in the efficiency for relieving jaundice, mortality and median survival between the two methods [45]. Some have reported morbidity as significantly higher following surgical bypass, especially; bile leak and pneumonia [46,47,48,49]. It was though reported that, recurrent obstructive jaundice due to stent occlusion or stent migration was higher in the endoscopic stenting group-17%-38% necessitating two or more stent replacement in life time [47,50,51,52]. The reports also indicated that 26% of the endoscopic stenting group developed gastric outlet obstruction in their later life requiring palliative intervention [45,51,52]. In Nigeria, it is either the endoscopic or percutaneous stenting techniques are not readily available or there is no requisite expertise to undertake them [17]. The Surgeon is often left with no option but the Surgical by-pass for the relief of billiary obstruction [17]. The pathophysiologic changes in those with obstructive jaundice make the administration of General Anaesthesia hazardous. The increased levels of circulating direct bilirubin are known to result in decreased cardiac contractility, reduced left ventricular pressure, Impaired response to beta agonist drugs and decreased peripheral vascular resistance. It also causes bradycardia, due to direct effect of bile salts on the SA node resulting in a Hypotensive patient with exaggerated hypotensive response to bleeding; who is prone to postoperative shock following administration of General Anaesthetic agents [24,25].
Several attempts have been made to provide palliative billiary drainage for this patients under regional or local anaesthesia [53]. The procedure of choice is however, a percutaneous trans hepatic biliary drainage (PTBD) by interventional radiologist under local anaesthesia [54]. In this study, all surgeries were done under local Anaesthesia involving cutaneous field block using Lignocaine with Adrenaline at a standardised dose of 4mg/ kg body weight and USS guided Subcostal TAP Block using 0.25% Levobupivacaine at a standardised dose of 0.3-0.6 ml/kg. The Transversus Abdominis Plane (TAP) Block, a form of local anaesthetic block was developed by Anaesthetists to provide analgesia to the anterior and lateral abdominal wall. The pioneers in this field include Rafi et al and McDonnell et al [55,56]. They are credited with providing a detailed description of the anatomical landmarks for the infiltration technique and demonstrated proof of both sensory and motor blockade to the mid/lower thoracic and upper lumbar spinal nerves that traverse the fascial plane between the transversus abdominis and internal oblique muscles [55,56]. Hebbard, et al. in 2007 described an ultrasound-guided approach to the TAP block and also described the method of identifying the plane of block between the rectus abdominis and transversus abdominis using hydro dissection technique [57]. The oblique subcostal TAP block is a modification of classical TAP block using USS guidance to identify plane between the rectus abdominis and transversus abdominis muscle near the costal margin [57]. It provides upper abdominal wall analgesia blocking T7-L1 dermatomes [57]. The Hebbard USS guided technique of oblique sub costal TAP block has proven over time to be an effective anaesthetic blocking tool for various drainage procedures around the upper part of the abdomen. It has been regularly and safely used in Percutaneous Trans hepatic billiary Drainage in patients where the administration of general anaesthesia is considered hazardous [53]. In countries like Nigeria, where the health sector is not developed, most rural hospitals lack facilities for general anaesthesia or the drugs and other paraphernalia for smooth intubation is unavailable [58-61]. Often, patients in rural areas travel hundreds of kilometres to hospitals with better equipped health care system to have major operations done [59]. Majority in Nigeria pay out of their pockets for health services, because; the National Health Insurance coverage is not universal and medical bill in many of the tertiary health centres is out of reach of the rural populace [61]. The common complications associated with general anaesthesia, such as nausea, vomiting and altered consciousness are obviated with use of regional anaesthesia. The use of adrenaline containing lignocaine minimizes bleeding and the need for transfusion and improves surgical field visibility. The analgesic effect continues postoperatively. This is thought to reduce the intensity of the systemic inflammatory response to the stress of surgery and ensures early post-operative recovery and probably, shorter hospital stay [59]. The average time of the procedure in this study is 30-45 minutes, with two cases extending to one hour due to excessive primary haemorrhage. The haemorrhage occurred despite achieving an adequate stabilisation of the INR at 1.3 for all patients. This may perhaps result from a clerical error in the reporting of the INR or an idiosyncratic reaction. The average intra-operative pain score using the NRS was 2-4. Only ten of the patients required a salvage dose of weak opioid analgesia (pentazocine) and anxiolytics (midazolam) due to agitation. The Wilson sedation score is often 1-2, which is quite safe [5] No anaesthesia related complications were recorded. Intraoperative pictures showing the operative procedures were taken (Figures 2-8).
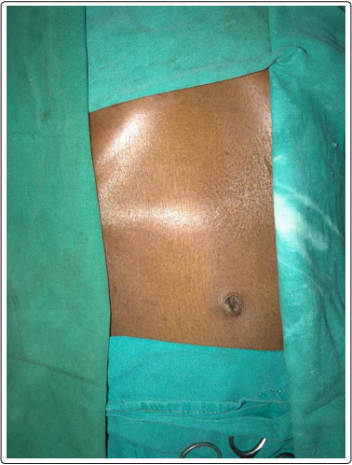
Figure 2: Showing the Prepared Operative Area with a Visibly Distended Gallbladder
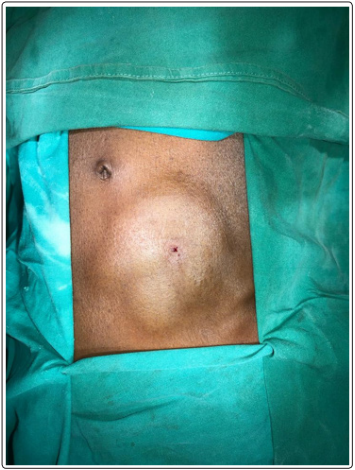
Figure 3: Showing the Infiltrative Cutaneous Field Block Given

Figure 4: Showing a slaty gray liver and a distended gallbladder picked by a rampley’s forcep
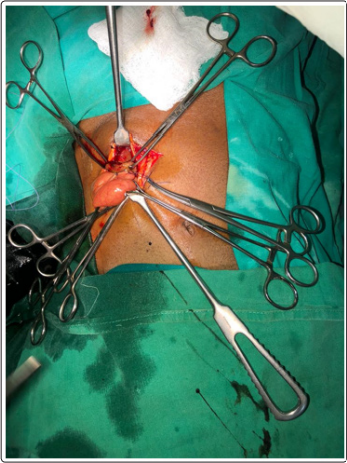
Figure 5:: Showing a Jejunal Loop apposed To the Gallbladder for Anostamosis

Figure 6:: Showing Abdominal Defect Closure

Figure 7: Showing the Sutured Operative Area

Figure 8: Postoperative Picture
The most common post-operative complications are Surgical Site Infection (SSI) at 24.1%, excessive Primary Haemorrhage and reactionary haemorrhage, at 9.3% each. Billiary leak and bile peritonitis occurred at 7.4% and 1.9% respectively. No recorded cases of recurrent jaundice or subsequent Gastric Outlet Obstruction were seen [TABLE 2]. However, most reports on the postoperative morbidity where comparing Surgical bypass with endoscopic stenting. This has been reported to be significantly higher after surgical bypass i.e., 31% (range 6%-56%) compared to the early post-procedure morbidity of 21% (range 8%-34%) after endoscopic stenting [40,62,63]. Surgical biliary bypass can be done by Cholecysto jejunostomy, choleodochoduodenostomy or hepaticojejunostomy. The reported Operative morbidity and mortality are almost similar for both cholecystojejunostomy and hepaticojejunostomy, they only markedly differ in their efficiency to alleviate jaundice. This was reported to be higher for hepaticojejunostomy than for cholecystojejunostomy (97% vs. 87%) [40]. Recurrent jaundice and cholangitis are also reported to be 8% for cholecystojejunostomy and 0% for hepaticojejunostomy because of late involvement of the cystic duct by a cholangiocarcinoma or pancreatic cancer [21,64]. No recorded cases of recurrent jaundice or subsequent Gastric Outlet Obstruction were seen (Table 2). This may perhaps be due to the relatively short life expectancy of less than 6 months in most patients. The total fatality rate was 7.4% (Table 2). In a case series from Johns Hopkins, a total of 118 patients were found to have unresectable periampullary malignancy at the time of surgery, surgical palliation was accomplished with 2.5% hospital mortality and an overall mean survival of 7.7 months [42]. Their mean postoperative hospital stay was only 14 days and most patients return to a regular diet at approximately 10 days. Our average hospital stay was 6-7 days. This may perhaps be due to the use of local anaesthesia and its related benefit of early recovery, shorter hospital stays and faster return to work [65]. There is dearth of data on survival and prognostic factors of hepaticojejunostomy and gastrojejunostomy surgery, particularly, from Africa. A study from central Asia found that the pooled median survival of pancreatic cancer bypass surgery was 6.7 months [8]. Other studies from the West indicated that the mortality and morbidity of palliative bypass surgery was 6.5% and 29% each and the median survival was about six months [66,67]
A palliative billiary by-pass is safe under regional/local anaesthesia, effective in providing adequate billiary drainage and associated with faster postoperative recovery and shorter hospital stay
It is a non-randomised, non-controlled clinical trial. A controlled arm of the same procedure under general anaesthesia would have brought the advantages to the fore.
Conflict of Interest: Non declared
