Author(s): Mahesh S* and Kripa Angeline A
Plummer-Vinson syndrome is a classical triad of dysphagia, iron-deficiency anemia and esophageal webs, Plummer-Vinson or Paterson-Kelly syndrome occurs. There is no exact data on the epidemiology of the condition; the syndrome is extremely rare. Most of the patients are middle-aged white women, but the syndrome has also been identified in children and adolescents in the fourth to seventh decades of life. Over the years, dysphagia is typically painless and sporadic or incremental, restricted to solids and often related to weight loss. The association with upper alimentary tract cancers is one of the most significant clinical aspects of Plummer-Vinson syndrome. Etiopathogenesis is unknown due to Plummer-Vinson syndrome.
Plummer-Vinson syndrome is defined by the classic triad of dysphagia, iron-deficiency anaemia and esophageal webs. Although the syndrome is very rare nowadays, its identification is significant because it recognizes a group of patients who are at elevated risk of pharyngeal and esophageal squamous cell carcinoma. In the past fifty years, the incidence of Plummer-Vinson syndrome has plummeted and this is likely associated with the rising rarity of severe iron deficiency anaemia, although the definite cause of remains unknown. A series of 1000 patients who had their hypopharynx and cervical oesophagus cineradiography failed to find a single case of syndrome of Plummer-Vinson. The condition is Plummer- Vinson syndrome can be treated easily and effectively with iron supplementation and dilation therapy. Iron replacement therapy can dramatically improve dysphagia, especially in patients with non-substantially obstructive web conditions. If there is significant obstruction of the esophageal lumen by the esophageal web as well as persistent dysphagia, balloon dilation of the web should be performed. With endoscopy or under fluoroscopy control, dilation therapy can be easily done. Most common in Caucasian women, usually from the age group of 30s to 60s [1-5].
A 28 years old female Mr. X, dysphagia for 2 years for both solid and liquid which is aggravated for past 3 months. Haematological tests showed the presence of iron-deficiency anaemia (serum Fe 10 μg/dL, ferritin 2.19 ng/mL, haemoglobin [Hb] 4.5 g/dL, haematocrit [Ht] 26.5%). The patient was treated with the oral ferrous sulfate agent, 256 mg, and twice each day for three months. She is also having dyspnoea on exertion, indigestion and nausea after taking the foods. No evidence of any co morbid illness. On 2009, 2 units of PRBC transfused due to the low level of haemoglobin (4.5 mg/dl).
On admission patient is afebrile, difficulty is swallowing for both solid and liquids foods. Rinne test is positive. Cold spatula test and cotton wool test, para nasal sinuses, Vestibular function test and fistula test was negative. In neck examination, enlargement in thyroid gland, laryngeal crepitus is there. Pulse rate of 80 beats per minute, Blood Pressure-130/70 mmHg. CVS - S1, S2 heard no murmurs. Respiratory system- Normal Vesicular Breath Sound heard. No added sounds.
ECG (baseline): Normal sinus Rhythm with 70 beats per minute, normal axis, PQRST normal, no significant ST- T changes.
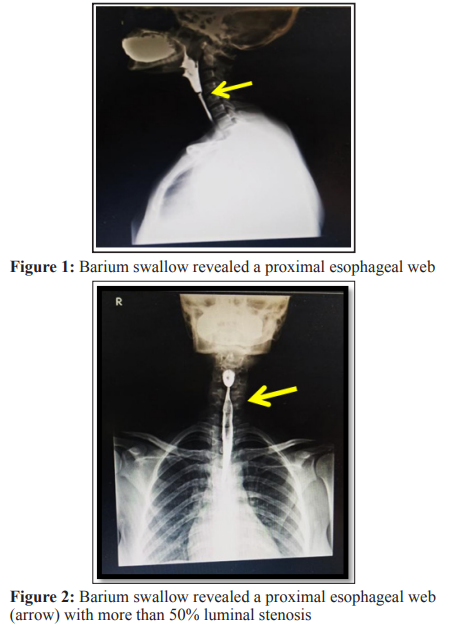
Barium swallow study: about 80 ml of barium suspension was given to the patient orally in small amounts and serial fluoroscopic spot exposures of the neck and thorax were made during the act of deglutition in AP/LAT.
Impression: cricopharyngeal web involving the anterior and lateral walls of the pharango-esophagus segment causing near total circumferential narrowing at the level of c4 as described [6-10].
After the diagnosis patient plan for Rigid Esophagoscopy under general anaesthesia with oesophageal web dilation.
Oesophageal web dilation procedure was explained by the surgeon a day before and consent was obtained. Patient was in Nil per Oral for 6 hours. Patient was intubated and stabilized in boyle’s position, pillow under the shoulder, neck flexed & head extended at atlanto-occipito joint. Rigid oesophagoscope was introduced and uvula was visualized. Scope was pushed further and epiglottis and endotracheal tube was visualized. Oesophagoscope is passed below the endotracheal tube and after that arytenoids are visualized. Upper oesophageal sphincter was seen and scopy was passed once the sphincter opens. Oesophageal web was seen at the cricopharynx and dilated using rigid oesophagoscopy. Finally patient was extubated and shifted to surgical intensive care unit for observation. Post-operatively, she was on IV fluids of normal saline 75 ml/hour and RL 75ml/hour. In addition to that inj. Ciprofloxacin 100 mg, injection diclofenac, T. Levogen added up to prevent the complications. Monitor for the complications like bleeding from the oral cavity, intracapsular pain, chest pain, dyspnoea, tachycardia and hypotension [11-15].
Patient has been following up regularly, prognosis was good. Patient was advised follow up for first 3 months and then the interval of 3- 6 months intervals.
The pathogenesis of this syndrome is not exactly understood but the most probable mechanism is iron deficiency. Other factors have not been shown to play an exact role in the pathogenesis of the syndrome, such as genetic predisposition, malnutrition and autoimmunity, while celiac disease, thyroid disease and rheumatoid arthritis have been documented with PVS. Whatever the source of the iron deficiency, this theory is based on the rapid loss of iron-dependent enzymes. Reduction of these enzymes may cause mucosal degenerations, atrophic changes and web formation and may even lead to cancer of the upper gastrointestinal tract. Previous studies have shown that iron deficiency has reduced the amplitude of oesophageal muscle contraction, resulting in impaired motility. Although iron deficiency anaemia is not uncommon in our country, we find very few cases of Plumer-Vinson Syndrome reported from India. Exact number of reported cases in children is not available. In contrast to adults Plummer-Vinson syndrome is rare [16-20].
Plummer Vinson Syndrome is best managed by an inter-professional team comprised of a primary care practitioner and gastroenterologist. Although esophagagastro duodenosocpies are often performed as the initial evaluation in patients presenting with dysphagia, abnormalities such as rings or webs may be missed and such patients should be evaluated further with a barium esophagogram.
The following advantages are provided through an oesophagus
expansion:
• Fast recovery, easy recovery
• Can easily resume food, drink and other activities
• Small malaise or pain
• Effective for oesophageal stringency relief.
• Lateral effects are typically small (such as a sore throat)
After the procedure is completed, the patient may switch to the intensive care unit for observation and discharge within a week.
It will take around a day for the pain in your throat to go down. If the pain is gone, a special diet might be required. The next day, you should be able to go back to your usual activities.
This case has been raised because of its rareness. Patients and primary care physicians need to be mindful of the slight risk of malignancy associated with this disorder and, if new symptoms such as persistent dysphagia or weight loss occur, such patients require long-term follow-up with timely evaluation. We assume that PVS should be examined for any patient presenting with symptoms of dysphagia and iron deficiency. The prognosis is strong, but frequent follow-up is important due to the risk of malignant transformation. Treatment, especially when it is not associated with carcinoma, is very promising [21-24].
