Author(s): Bruno Riccardi*, Sergio Resta and Rita Storelli
Numerous evidence and clinical trials have been published in recent years on the role of silicon for the maintenance of general well-being and of bones in particular. However, no study has so far investigated which fundamental contribution to health could provide silicon when taken with other trace elements in cases, very frequent, of their insufficient contribution. In this work we present a preliminary open-air study on a group of patients, using an original and innovative formulation containing organic SI G5 plus other trace elements, for the prevention and treatment of osteoarticular diseases of various origins.
Silicon is the chemical element that has as its symbol “Si” with valence 2, 4, 6 and atomic number 14. There are two kinds of silicon in nature: mineral silicon and organic silicon. Mineral silicon is the main component of the earth’s crust (27.80%) immediately after oxygen (46.60%). Mineral silicon is composed of a silicon atom bound two oxygen atom Fig.1.
Figure 1: Mineral silicon structure formula
Organic silicon has a structure different from mineral one. In fact, it has one or more carbon atoms associated with hydrogen (Fig. 2)
Figure 2: Organic silicon structure formula G5
Organic silicon is an essential element for all living matter. In the
human organism it is found in large quantities in tissues.
Compelling evidence continues to accumulate indicating that
silicon is a beneficial trace element and contributes to health.
Data from human, animal, and in vitro studies demonstrate that
dietary silicon increases bone mineralization, collagen synthesis,
improves structural integrity of skin, hair and nails, modulates
the immune system and inflammatory response, and mitigates
the risk of atherosclerosis.
Silicon deficiency as shown in animal studies induces deformities
in skull and peripheral bones, poorly formed joints, reduces
cartilage and collagen, and disrupts mineral balance in the femur
and vertebrae. Silicon is one of the essential elements of living been
and, after iron and zinc, is the third most abundant trace element
in the human body. Silicon is found in all cells and tissues but is
especially prevalent in connective tissues [1-4]. Numerous studies
suggests strongly that silicon is, in fact, a necessary, and likely
essential, dietary element. Connective tissue is a vital component
for the health of every organ throughout the body. Connective
tissue makes up a variety of physical structures including joints,
cartilage, bones, skin (nails and hair) and blood vessels including
the heart. Therefore, organs require silicon to restore or conserve the
healthy homeostasis and equilibrium but with the ageing process the
concentration of silicon present in the organs diminishes. Because
silicon deprivation has not been shown to interrupt the life cycle
in mammals, or to have a defined biochemical function, silicon is
not generally accepted a san essential nutrient for higher animals
and humans. However, 40 years of research shows that silicon has
beneficial effects, especially on the formation of connective tissue
and bones, in higher animals and in humans.
There are different types of silicon, of vegetable or synthetic origin, which are proposed on the market as supplements in different concentrations and formulations. There are also various silicon polymers proposed for the synthesis of bone implants. To date, the form of silicon that has shown the best absorption and bioavailability for the integration is the organic silicon G5. The human being is unable to transform the ingested mineral silicon into organic silicon. Only micro-organisms and plants are capable of directly assimilating minerals. Only organic silicon produced by micro-organisms has the characteristics of bioavailability and is directly assimilable. In fact, microorganisms generate an important percentage of organosilicates in the biological cycle that becomes organic and bioavailable.
Organic silicon G5 is the most bioavailable form of silicon. A comparative study on the absorption of silicon published by the British Journal of Nutrition, and conducted on volunteers at the St. Thomas Hospital in London, confirmed the very high bioavailability of organic silicon. The study used organic silicon G5® (MMST) produced by LLR-G5 and showed that the absorption of silicon was high (about 60% in general and up to 70% in some subjects). Fig.3
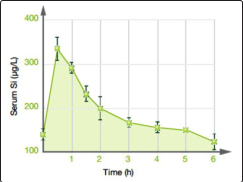
Figure 3: Absorption of Organic Silicon G5
The absorption of organic silicon G5® as Fig 4 shows, is considerably higher than the other known silicon supplements, at least four times higher than the other known forms of integration [5-9].
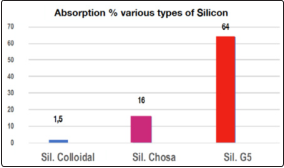
Figure 4: Comparison of absorption of various types of silicon
Organic silicon G5® is not only very easily absorbed by the organism, but is also metabolized as biological silicon (“orthosilicic acid”) (*)
Collagen, which is present in connective tissue, is the most abundant of all proteins in higher vertebrates, accounting for up to one-third or more of the total body protein. Silica in its bioactive forms, plays an important role in collagen synthesis. Collagen contains 12% of the aminoacid proline and 9% of 4-hydroxyproline. Silica increases synthesis of proline from glutamic acid. In the presence of iron and vitamin C, silica enhances markedly hydroxylation of proline residues of procollagen to form collagen. Silica also promoted the formation of extracellular matrix (ground substance) with a concomitant increase in interstitial fluid, due to hydration of the extracellular substances. Si function as a biological crosslinking agent and contribute to architecture and resilience of connective tissue. Fig. 5 [10-12].
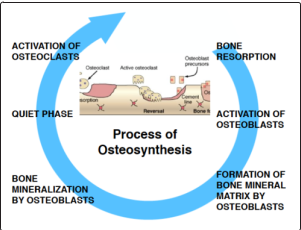
Figure 5: Silicon activates the prolyl-hydroxylase enzyme, present in the granular endoplasmic reticulum of the osteoblast cytoplasm. The enzyme governs the formation and bone mineralization
Silicon is an element that is increasingly appreciated for is important roles in improving bone matrix quality and facilitating bone mineralization. In addition, silicon increases BMD and improves bone strength Fig.6 [13-14].
(*) MMST is an amphiphilic, and highly permeable organosilicon molecule [Si(OH)3CH3] that shows stability even at concentrations above 20 mM (millimoles) at room temperature and possesses rapid/high absorption and no adverse effects have been reported. After its intestinal absorption, MMST is converted into biologically active orthosilicic acid.
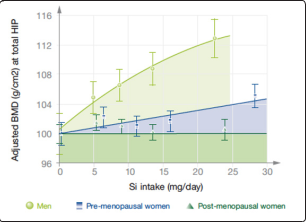
Figure 6: The relationship between silicon intake and bone mineral density
In the last decade, epidemiological studies and clinical trials showed micronutrients can potentially have a positive impact on bone health, preventing bone loss and fractures, decreasing bone resorption and increasing bone formation. Consequently, optimizing micronutrients intake might represent an effective and low-cost preventive measure against osteoporosis. Several authors have proposed different macros and micronutrients to be used for the prevention of osteoarticular diseases, with particular attention to osteoporosis. Based on their experience, and/or scientific background, the different authors have listed and analyzed the effects of specific nutrient associations that may find useful application as supplements [15-21]. Based on these experiences we tested the effectiveness and safety of the association of G5 organic silicon with other trace elements in nutraceutical formulation, on a case study of patients with different osteoarticular diseases. The objective of the work is to demonstrate the synergistic effectiveness of nutrients in the prevention of osteoarticular degenerations and in the control of inflammation and pain associated with them. Let’s list briefly, the effects of individual nutrients on bone metabolism reported in the literature and the expected synergy effect. In addition to the effects of organic silicon G5 already described, the other substances present in our formulation have demonstrated the following activities:
Direct and indirect mechanisms contribute to the effects of low magnesium on bone density: low magnesium can directly affect the bone by altering the structure of apatite crystals; magnesium deficiency is also associated with reduction of PTH and 1, 25(OH2) D levels and low grade inflammation and endothelial dysfunction, with a well-known relation between inflammation and bone loss.
Zinc is a cofactor in many metalloenzymes and is an extremely important element from the point of view of bone health. Zinc is fundamental in the regulation of bone homeostasis. Many zinc- related proteins are found to involve in the regulation of cellular function in osteoblasts and osteoclasts, in addition stimulates mineralization in osteoblasts through gene expression of various proteins including type I collagen, alkaline phosphatase, and osteocalcin. Inhibits osteoclastic bone resorption suppressing osteoclastlike cell formation, and stimulates gene expression in osteoblastic cells.
Vitamin D3 is the most important among vitamin D forms, which are a group of lipid-soluble secosteroids in the human body. The final metabolite of vitamin D3, calcitriol (1,25-dihydroxyvitamin D3), binds to the intranuclear vitamin D receptor in the intestines, bones, kidneys, and parathyroid gland cells. Vitamin D3 modulates calcium metabolism, including intestinal absorption, renal excretion, and bone resorption. Vitamin D can be synthesized in the human skin by a photochemical process but the capacity of production decreases with age.
Vitamin K is a group of fat-soluble vitamins that includes two types: vitamin K1 (Phylloquinone) and vitamin K2 (Menaquinone). Menaquinone synthesized from phylloquinone in the human body; thus, vitamin K1 deficiency generally results in vitamin K2 deficiency. The menaquinone family of K2 homologs is a large series of vitamins containing normally unsaturated isoprenyl side chains that vary in length. Menaquinone-4 (menatetrenone) is the most-studied, active form of vitamin K2 and is considered to aid the -carboxylation of osteocalcin, which is produced by osteoblasts during bone matrix formation.
Experimental evidence suggests that bromelain’s action as an anti-inflammatory is mediated via the following factors:1) by increasing serum fibrinolytic activity, reducing plasma fibrinogen levels and decreasing bradykinin levels (which results in reduced vascular permeability) and hence reducing oedema and pain; 2) by mediating prostaglandin levels (by decreasing levels of PGE2 and thromboxane A2); and 3) through modulation of certain immune cell surface adhesion molecules (16-20), which play a role in the pathogenesis of arthritis [27-30]. We have summarized the expected synergy effect with our formulation. Fig.7
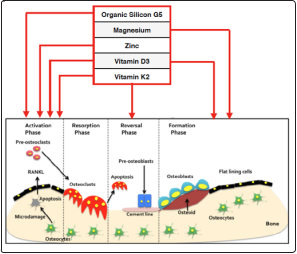
Figure 7: Synergistic Action assumed of the Nutrients involved in bone remodeling
Some authors reported negative experience with the use of antiosteoporotic drugs, which have not shown significant efficacy and the presence of some side effects [31-36]. This further encouraged us to undertake our preliminary investigation with the use of alternative treatments to traditional drugs, based on natural substances, on a group of patients, to test their efficacy and tolerability.
Our supplement consists of the following components Tab.1:
Organic silicon G5: 300 mg, Magnesium: 400 mg, Zinc: 35 mg, Vitamin D3: 1000 U.I. Vitamin K2: 35 mcg and gastro-protected Bromelain: 100 mg (2.500 GDU/g), administered with sachets containing soluble powder.
Table 1: Supplement Composition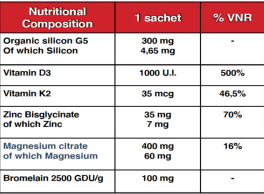
The work is an observational survey conducted in Italy by basic doctors on 300 patients distributed in different geographical areas of Italy in view of the different socio-economic and territorial conditions of the patients examined. The survey began in January 2019 until March 2020, even during the COVID19 pandemic.
The aim of this work is to evaluate the effectiveness and tolerability of a supplement based on Organic Silicon G5, microelements and vitamins, in adults to prevent and/or treat deficiencies from insufficient intake of these nutrients. Simple open-label works with control of haematological and functional parameters (Data on reserved files)
Administration of a questionnaire for an anamnestic survey. The first part of the questionnaire relates to personal history, with regard to predisposing diseases.
Age, ethnicity, smoking, physical activity, BMI, food (Some of these data are not reported)
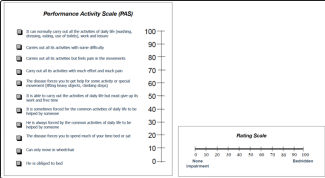
300 osteopenic, but otherwise healthy, Caucasian with a PAS -score < 40
Patients 60 years or more of age; of both sexes who have been asked for informed written consent; Patients enrolled with various degrees of Osteoarthritis and other musculoskeletal diseases were checked with routine examinations at the beginning and end of treatment by physicians.
Joint pain; Functional impairment; Stiffness in movements: To which was assigned a semi-quantitative value from 100 to 0, where 100 is good - 0 is bad: Table I
Patients were excluded according to the following criteria: Patient with infectious diseases of any nature, blood transfusions, renal failure as defined by serum creatinine > 200μmol/L, abnormal serum ferritin level (normal range: 11-250μg/L), concomitant medication treatments like: Anti-inflammatory and antiosteoporous drugs were excluded, those in treatment with anti-inflammatory drugs have been subjected to a two-month wash-out period before starting treatment. However in some subjects with marked painful symptoms, we maintained an initial treatment with anti- inflammatory to contain pain, which were completely eliminated when the painkiller effect of our product began.
Patients were treated for six months at the dosage of one sachet a day. Patients with ineffective previous treatments have been included too.
All study methods and procedures were conducted in accordance with the ethical standards of the Declaration of Helsinki and Good Clinical Practice guidelines.
A basic clinical examination was performed at each visit including measurement of body weight, height, systolic and diastolic blood pressure and heart rate. Blood samples and single void urine samples were collected from fasting subjects at baseline and after 6 months supplementation to evaluate the safety parameters. All serum and urine parameters were measured at baseline and after 6 months supplementation.
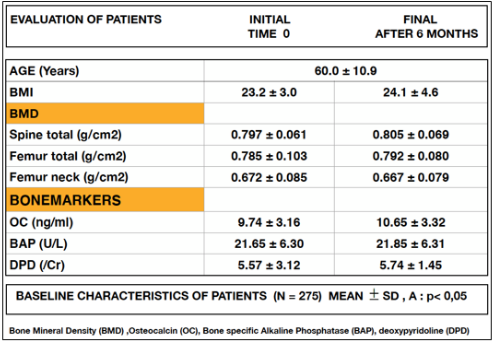
Bone Mineral Density (BMD) by Dual-Energy X-ray Absorptiometry (DEXA), Osteocalcin (OC), Bone specific Alkaline Phosphatase (BAP), and deoxypyridoline DPD were measured by a competitive immunoassay ELISA method.
Of the 300 Patients randomised into the study, only 275 completed the study. Reasons for withdrawal were unforeseen illness/ medical (COVID 19) conditions. All treated subjects showed clear improvements in osteoarticular functional parameters. The first follow-ups planned three months after the start of the experiment (not reported in the study) showed an increase in muscle work done in everyday life with a conspicuous reduction in pain and tenderness of the various bone segments affected by degenerative phenomena of arthrosis. The use of NSAIDs was reduced in the first three months of experimentation until their use was almost completely abolished six months after the start of therapy. The results show that the blood chemistry parameters examined described in the Measurements section were found to be normal, and did not undergo any particular changes during the treatment. While Biochemical markers of bone formation, despite the variability between the various subjects, showed a significant improvement. Tab.
Table
In our study we mainly evaluated the effects found on the morphofunctional parameters, obtained with the treatment, rather than on those of the haematochemical values and on the pathogenetic markers. Among these, the reduction of pain and the improvement of mobility (Performance Activity Scale -PAS and Rating Scale), are of fundamental importance and clinical significance in the evaluation of the results obtained, according to international guidelines [37-40]. On the basis of the results obtained using the rating scales in Table 1, we found an improvement in the PAS which went from a value of 60 to 80 and in the Rating Scale from 45 to 18, followed by a significant functional recovery. The follow-ups planned three months after the start of the experiment showed an increase in muscle work done in everyday life with a conspicuous reduction in pain and tenderness of the various bone segments affected by degenerative phenomena of arthrosis. We believe that this effect is due to the concomitance of two factors: 1) the effectiveness of the supplement’s active ingredients; 2) parallel muscle rehabilitation synchronous to the improvement of joint excursions dependent on an increase in muscular function. Among the beneficial effects attributable to supplementation, mention should also be made of the anti-inflammatory action mediated by bromelain in synergy with Vitamin D3 and K2. Vitamins filled chronic and dangerously asymptomatic deficiency syndromes, while bromelain ensured a periarticular anti-edema effect which, in addition to the “restitutio ad integrum” of the affected bone segments, also favored an antithrombotic effect on the locoregional circulation forced by the perilesional edema a consistent flow slowdowns. We believe that: for the benefits achieved in terms of articular excursion, for the net reduction of pain and tenderness of the bone joints, for the reduction of lesional edema, the supplement becomes a valid therapeutic support aimed at recovery functional osteoarticular. Autors’s declaration: This is an open-access article distributed under the terms of the Creative Commons Attribution Non- commercial License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited, the use is noncommercial and is otherwise in J Biotechnol Bioinforma Res, 2021 compliance with the license. See: http://creativecommons.org/ licenses/by-nc/3.0/ and http://creativecommons.org/licenses/by- nc/3.0/legalcode
The authors report no conflicts of interest in this work.
1. Martin KR (2018) Dietary Silicon: Is Biofortification
Essential?, Journal of Nutrition and Food Science Forecast.
2. Forrest H Nielsen (2014) Update on the possible nutritional
importance of silicon, Journal of Trace Elements in Medicine
and Biology 28: 379-382.
3. Elisa Borsani et al. (2005) Histochemical and
immunohistochemical evaluation of gingival collagen and
metalloproteinases in peri-implantitis, Acta histochemica
107: 231-240.
4. George R Beck et al. (2012) Bioactive silica based
nanoparticles stimulate bone forming osteoblasts, suppress
bone esorbing osteoclasts, and enhance bone mineral density
in vivo, Nanomedicine 8: 793-803.
5. Supannee Sripanyakorn et al. (2009) The comparative
absorption of silicon from different foods and food
supplements, Br J Nutr 102: 825-834
6. Anderson Oliveira Ferreira et al. (2018) Anti-Aging Effects
of Monomethylsilanetriol and Maltodextrin-Stabilized
Orthosilicic Acid on Nails, Skin and Hair; Cosmetics 5: 41.
7. DV Scholey et al. (2018) Bioavailability of a novel form of
silicon supplement, Scientific Reports 8: 17022.
8. Anna Prescha et al. (2019) Dietary Silicon and Its Impact on
Plasma Silicon Levels in the Polish Population, Nutrients
11: 980.
9. David M. Reffitt et al. (1999) Silicic acid: its gastrointestinal
uptake and urinary excretion in man and effects on aluminium
excretion, Journal of Inorganic Biochemistry 76: 141-147.
10. Klaus Schwarz A (1973) Bound Form of Silicon in
Glycosaminoglycans and Polyuronides (polysaccharide
matrix/connective tissue), Proc Nat Acad Sci USA 70: 1608-
1612.
11. Meng Dong et al. (2016) Biological Silicon Stimulates
Collagen Type 1 and Osteocalcin Synthesis in Human
Osteoblast-Like Cells, Biol Trace Elem Res.
12. Jugdaohsingh R et al. (2004) Dietary silicon intake is
positively associated with bone mineral density in men and
pre-menopausal women of the Framingham Offspring cohort.
Journal of Bone and Medical Research 19: 297-307.
13. Charles T Price et al. (2013) Silicon: A Review of Its Potential
Role in the Prevention and Treatment of Postmenopausal
Osteoporosis International Journal of Endocrinology, Article
ID 316783: 6p.
14. R. Jugdaohsingh (2007) Silicon and bone Health, Nutr Health
Aging 11: 99-110.
15. DM Reffitt et al. (2003) Orthosilicic acid stimulates collagen
type 1 synthesis and osteoblastic differentiation in human
osteoblast-like cells in vitro. DM Reffitt, Bone 32: 127-135.
16. G Della Pepa, ML Brandi (2016) Microelements for bone
boost: the last but not the least; Clinical Cases in Mineral
and Bone Metabolism 13: 181-185.
17. Alberghini Maltoni A, G Suffritti (2018) The Determining
Role of Silicon in Bone Formation: Review and Clinical
Results; Journal of Clinical Medicine and Therapeutics 1: 05.
18. Yuichiro Ukon et al. (2019) Molecular-Based Treatment
Strategies for Osteoporosis: A Literature Review, Int J Mol
Sci 20: 2557.
19. Mariangela Rondanelli et al. (2013) Update on nutrients
involved in maintaining healthy bone. Endocrinol Nutr 60:
197-210.
20. Charles T Price et al. (2012) Essential Nutrients for Bone
Health and a Review of their Availability in the Average North
American Diet, The Open Orthopaedics Journal 6: 143-149.
21. Tim D Spector et al. (2008) Choline-stabilized orthosilicic
acid supplementation as an adjunct to Calcium/Vitamin D3
stimulates markers of bone formation in osteopenic females:
a randomized, placebo-controlled trial, BMC Musculoskeletal
Disorders 9: 85.
22. Sofie Hertz R∅nn et al. (2016) Vitamin K2 (Menaquinone-7)
prevents age-related deterioration of trabecular bone
microarchitecture at the tibia in postmenopausal women,
European Journal of Endocrinology 175: 541-549.
23. MHJ Knapen et al. (2007) Vitamin K2 supplementation
improves hip bone geometry and bone strength indices in
postmenopausal women, Osteoporos Int 18: 963-72.
24. Celia Rodrguez-Olleros Rodrguez and Manuel Daz
Curiel (2019) Vitamin K and Bone Health: A Review on
the Effects of Vitamin K, Hindawi Journal of Osteoporosis,
Article ID 2069176: 8p.
25. Guangliang Hao et al. (2017) Vitamin K intake and the risk
of fractures, A meta-analysis, Medicine 96: 17.
26. Aleksandra Niemiec et al. (2020) Multi-faceted function
of vitamin K with particular consideration of vitamin K2 -
literature review, Pomeranian J Life Sci 66: 39-44.
27. Bromelain Monograph (2010) Alternative Medicine Review
15: 4.
28. HR Maurer (2001) Bromelain: biochemistry, pharmacology
and medical use, CMLS, Cell. Mol. Life Sci 58: 1234-1245.
29. Bitange Nipa Tochi (2008) Therapeutic Application of
Pineapple Protease (Bromelain): A Review, Pakistan Journal
of Nutrition 7: 513-520.
30. Sarah Brien et al. (2004) Bromelain as a Treatment for
Osteoarthritis: a Review of Clinical Studies, eCAM 1: 251-
257.
31. Pablo Alonso-Coello and colleagues (2018) Drugs for pre-
osteoporosis: prevention or disease mongering?, BMJ 336.
32. IR Reid (2015) Efficacy, effectiveness and side effects ofmedications used to prevent fractures, Journal of Internal
Medicine 277: 690-706.
33.Morton Scheinberg et al. (2018) Efficacy and safety of a
fixed-dose combination of nimesulide/pantoprazole compared
to naproxen/esomeprazole for pain relief in patients with
osteoarticular diseases and dyspeptic symptoms, Drug Design,
Development and Therapy 12: 2775-2783.
34.Eduardo de Almeida Macêdo et al. (2018) Efficacy and Safety
of a Fixed-Dose Combination of Nimesulide/Pantoprazole
Compared with Naproxen/Esomeprazole for Pain Relief
in Patients with Osteoarticular Diseases and Dyspeptic
Symptoms , American College of Rheumatology, Meeting
Abstracts Number 422.
35.Hamid Reza Farpour et al. (2020) Efficacy of Piroxicam
Mesotherapy in Treatment of Knee Osteoarthritis: A
Randomized Clinical Trial, Evidence-Based Complementary
and Alternative Medicine, Article ID 6940741: 8p.
36.Wei Zhang et al. (2019) Emerging Trend in the Pharmacotherapy
of Osteoarthritis, Frontiers in Endocrinology.
37.Irena Kafediska et al. (2009) Association between
Osteoarticular Scores and Acute Phase Reactant Levels In
Rheumatoid Arthritis, JMB 28: 116-121.
38.Umberto Tarantino et al. (2017) Clinical guidelines for
the prevention and treatment of osteoporosis: summary
statements and recommendations from the Italian Society
for Orthopaedics and Traumatology, J Orthop Traumatol
18: S3-S36.
39.Ranuccio Nuti et al.; Guidelines for the management of
osteoporosis and fragility fractures, Internal and Emergency
Medicine 14: 85-102.
39.Nicola Lamberti et al. (2018) Home-based exercise for
elderly patients with intermittent claudication limited by
osteoarticular disorders - feasibility and effectiveness of a
low-intensity programme, Vasa 47: 227-234.
