Author(s): Monira Alzaheani, Nourh alghtani, Jawaher alsahabi, Alia Alkhelb and Afaf Felemban*
Conventional laparoscopic myomectomy (LM) has inherent limitations due to its rigid structure. The robotic system is a newly developed technology equipped with a flexible EndoWrist that offers good performance in delicate motions. Our objective was to share our clinical experience in the management robotic myomectomy
| Parameter | Patients (n=42) |
| Mean age | 37 years old ( 29-50) |
| Mean BMI | |
| Size of the Myoma Median size (greatest dimension) of resected lesions | 7.5 cm ( 4 -20cm ) |
| Type of myoma | 71 % (30 /42 ) IM ,21 % ( 9/42 SS) 7% / , 3/42 SM |
| Operation time | 153 minutes ( 89-275 minutes ) |
| EBL | 100 ml ( 50 -800 ml ) |
| Complications | None |
| Conversion to laparotomy | None |
| Histopathology Hospital stay |
Benign Myoma 3 nights ( 2-3 nights) |
Uterine fibroid is very common gynecology tumor world wide. In regards to kingdom of Saudi Arabia Hanan Y. 2016, published a paper showed high prevalent rate of leiomyomata in reproductive age group with incidence percentage of (21.2%) further more, that the incidence of fibroid is increasing during reproductive age and with women grow older with multiple bleeding and pelvic pain symptoms [1]. However, agreed treatment for patient considering uterine preservation is myomectomy with known superiority of minimal invasive techniques. Laparotomy is the traditional procedure used for myomectomy. However, laparotomy was responsible of aftermath, such as adhesions and heavy post surgery symptoms (bloodloss, pain, long hospitalization duration.) [2,3].
Further more, Minimal invasive surgery is rapidly replacing laparotomy in the field of gynecologic surgery. In otherhand Robotic assisted myomectomy can provide low mobidity and short hospital stay, and it is not difficult for skilled endoscopic surgeon to cross the threshold as long as they aer familiar with robotic operating arms (T). Generally, there are limited data concerning the utility of robotic surgery myomectomy. Specifically, in Saudi Arabia, a third-world country, data are further limited. The purpose of this study is to retrospectively report our robotic assisted laparoscopic myomectomy experience in terms of feasibility, safety and perioperative outcomes.
All cases referred to One expert surgeon in minimal invasive gynecology surgery and robotic as case of symptomatic fibroid in terms of pelvic pain , menorrhagia , infertility . cases were suspicious of malignancy were excluded and referred to gyneoncolcogy for laparotomy .Cases were screened and if case was challenging either by the size or the site were scheduled for robotic myomectomy rather than laparoscopy myomectomy
The study took place at National guard health affairs, Riyadh, Saudi Arabia. From April 2009 to feb 2018, all Robotic assisted laparoscopic myomectomy procedures were analyzed for pre-, intra- and post-operative details.
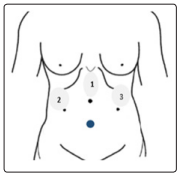
Surgical Approach was as Follow: after adequate general anesthesia patient will be positioned in dorsal lithotomy. Cleaning and draping will be done as hospital local protocol. Then uterine manipulator will be introduced. three trocars were used, first one above the umbilicus l by 8 cm and the size will be 8mm for the scope, second one will be 10 mm third one will be 5mm size trocars at left and right subcostal areas as shown in Figure 1. Then, central docking of the robot will be utilized and the surgeon will proceed with the surgery while sitting on the console. All cases under went myomectomy four cases had concurrent procedure, two had ovarian cystectomy and another two cases required hysteroscopy for submucosal fibroid or polyp excision
Myomectomy was started with Vasopressin injection in the capsule with conventional laparoscopy then myomectomy would be done through enucleation of the myoma out of the capsule, using bipolar and nonpolar scissor. After that suturing will be done via V’ lock stitch in one to three layers according to the depth of dead space. Anti-adhhesions material will be placed on the scar to prevent adhesions. Myoma was removed via power morcelleator.
A total of 42 records were analyzed. Patients Demographic data including age, BMI, type and size of myoma, Operative time, EBL and complications. Additionally, evaluation histopathology has been done . two case operative time details were missing.
Data were analyzed with Microsoft Excel 2013. Whenever possible, data were presented as percentages, median and range values.
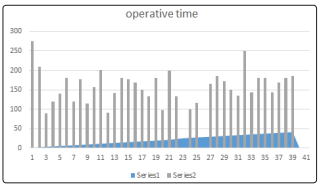
Operative time was 153 min; range ( 89-275 minutes ) .median of estimated blood was reported as 100 ml ( 50 -800 ml ), hospital stay was 2 nights with few cases kept one day more mostly for patient request, no cases required conversion to laparotomy all histopathology came as benign myoma.
The characteristics of myomas size was 7.5 cm (4 -20cm ) types as 71 % (30 /42 ) IM ,21 % ( 9/42 SS) 7% / , 3/42 SM.
Laparoscopy has clearly shown its short-term benefits in several studies, compared to laparotomy, such as reduced postoperative pain, shorter hospital stay, and faster recovery. It also proved its similar therapeutic efficacy and safety (for myomas of≤6cm diameter and if their number did not exceed four myomas). However meidan size of the myoma in our data was 7.5 cm. As 2015 FDA approved robotic use for gynecology since then experience with robotic myomectomy has been improved and myomectomy can be safely and effectively done with larger size and may be with multiple as well. Especially, laparoscopy is a more difficult procedure for surgeons, when>8cminsize. Sutures are difficult to place and require well trained and experienced surgeons [4].
Ranes M et all in 2016 and Advincula AP in 2007 emphasis in the significant difference in operative time as drawback of Robotic myomectomy when compared to other routs while he reported mean time of 239.7 minutes and 231 mintues respectively , however in our local experience Operative time was 153 min; range ( 89-275 minutes ) [5].
Further more, it is known that robotic surgery has Short learning curve for that we tried to look for our experience in time line as shown in the chart 1, with Case 32was accompanied with adhesolysis, bowel was adherent to the posterior uterine wall and anterior abdominal wall, uterus was 14 weeks size as well, 21 4to 5 fibroids largest 10 by 8 cm , 11 10 by 8 cm im fibroid in 23, 36 operative time was missing in the cahrts [6].
In the retrospective study of Advincula et al. (12) that compared conventional laparotomy and robotic laparoscopy, the robotic surgery needed longer operating time but with this technique blood loss and length of hospital stay were significantly reduced; laparotomy was associated with higher rates of morbidity. The longer operating time associated with the robotic technique is related to the time necessary to setup the robot and to myoma extraction by morcellation [7,8].
Our study results demonstrated that RALM is a safe and effective method for handling myomectomy, operative time can be improved in experts’ hands.
