Author(s): Ashwini Kale* and Ashish kale
Endometriosis is defined as the presence of endometrial like stroma and glands outside the uterine cavity. Laparoscopy has been recognized as the gold standard for endometriosis diagnosis and has been used for the surgical treatment of endometriosis. Diagnosis of endometriosis is currently made following laparoscopic inspection of the pelvis, preferably with histological biopsy confirmation.
Any surgeon intending to perform laparoscopic surgery for endometriosis must have a complete understanding and a thorough knowledge of the anterior abdominal wall vascular anatomy. This knowledge will reduce vascular complications associated with laparoscopy especially trocar placement. Of particular concern are the superior and inferior epigastric vessels. The superior epigastric artery, one of the terminal branches of the internal thoracic artery, enters the rectus sheath first and then the rectus muscle coursing near its lateral border. This artery and its adjacent vein often can be visualized by transillumination of the abdominal wall with the laparoscope.
Visualization of the ventral abdominal wall laparoscopically will often locate the deep inferior epigastric vessels. The artery, a branch of the external iliac, and its accompanying vein course along the abdominal wall peritoneum just lateral to the rectus muscle until midway between the symphysis pubis and umbilicus, where it blends into the body of the rectus muscle. These vessels may be seen medial to the insertion of the round ligament at the deep inguinal ring. Therefore, placement of the trocar lateral to the deep inguinal ring and lateral border of the rectus muscle will avoid injury to these vessels.
If placement of the trocar is too far laterally, branches of the superficial circumflex iliac vessels may be injured. Again, transillumination of the anterior abdominal wall by using the laparoscope will assist in avoiding these vessels.
As a general guideline, the superficial and inferior epigastric vessels are located approximately 5.5 cm from the midline. The superficial circumflex iliac vessels are approximately 7 cm from the midline. Theoretically, a “safe area” would be 8 cm above the symphysis pubis and 8 cm from the midline. If transillumination is not effective due to a thick abdominal wall, the surgeon may consider insertion of a spinal needle through the abdominal wall at the selected trocar insertion site. If no bleeding is observed after removal of the needle, the location is likely safe for trocar placement.
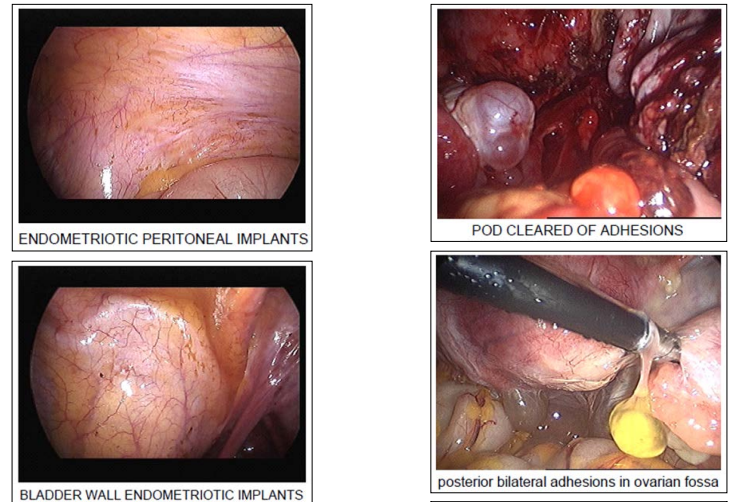
Laparoscopy in endometriosis is based on the visualization of superficial implants, endometriomas, adhesion distribution, bowel disease and ureteric disease. In doubtful cases, biopsies showing glands and stroma have been the basis of the diagnosis. Endometriotic lesions can vary in colour, mostly non-black, red, white or like burned powder. In clinical observation the age of a lesion can be estimated from the colour. It appears that clear papules are limited to a younger age group (17-31 years), than the red (16-43 years) and black (20-52 years) lesions.
In some cases asymptomatic women endometrial implants have been found in biopsies from normal peritoneum, resulting in the suggestion that mild endometriosis is not a disease and that all women have this mild form of endometriosis.
One-third of all diagnostic laparoscopies revealed endometriosis, one-third revealed no visible pathology, and the remaining onethird demonstrated a variety of other gynecologic conditions .Thus, two-thirds of all patients who undergo this invasive diagnostic procedure will not have endometriosis. To avoid false negative endometriotic lesion biopsy a multiple biopsy approach was proposed .
The American fertility Society proposed a new classification which was at that time simple and the most informative. Now a widely used classification of endometriosis (renamed as the revised American Society for Reproductive Medicine (rASRM) includes number, size and location of endometrial implants, endometriomas and if present adhesions. It is based on the appearance, size, and depth of peritoneal and ovarian implants;
on the presence, extent and type of lesions: red (red, red-pink, and clear), white (white, yellow-brown, and peritoneal defects) and black (black and blue); on the presence, extent, and type of adnexal adhesions and the degree of cul-de-sac obliteration. This helped to establish the stage of the disease as Stage I( minimal disease), Stage II ( Mild disease), Stage III ( Moderate disease) and Stage IV (Severe disease.
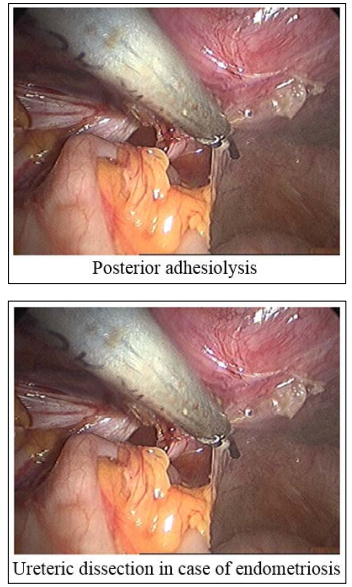
The severity of pain symptoms in minimal disease are found not to be correlated with findings at laparoscopy. Surgical approaches like resection of peritoneal endometriosis; or monopolar electrocoagulation/ablation may be used. In the early stages, surgical treatment seems to reduce pain symptoms as effective as by drug therapy. In the resection technique the peritoneum is incised near the lesion using a monopolar electrode and is dissected bluntly, separating healthy tissue from endometriotic tissue. Resection seems to be more efficient than diathermy coagulation, yet, it is more difficult, increases the time of the operation, and the cost. Monopolar electrocoagulation is done by applying a monopolar electrode to the visible endometriotic lesion. Extra care must be taken when treating the lateral pelvic side wall to avoid thermal damage to the ureter. To minimize this thermal effect, the peritoneum on the pelvic side wall could be opened and dissected to allow visualization of the ureter. Alternatively, ‘hydroprotection’ can be used. This involves injection of 0.9% saline under the diseased peritoneum, which elevates the peritoneum, allowing safe vaporization or diathermy.
For peritoneal endometriotic implants, a power setting of 40-50 W (laser CO2) is usually used using a continuous firing mode. To date, only one double-blind, RCT has been reported that examined the effect of laparoscopic treatment of endometriosis on pain (Sutton et al., 1994). This study has shown that laser excision of endometriosis significantly improves pain symptoms. However, this study has been criticized because the investigators performed semaltenously laparoscopic uterine nerve ablation and laser excision of the endometriosis and hence we cannot know which treatment has resulted in the pain relief. Sutton et al (1997) in a follow up study reported that 90% of responders had a pain relief for 1 year after laser excision, while 29% of patients had progressive disease and the same percentage (29%) had spontaneous regression. Finally, pain symptoms reported to be improved with the use of Helica TC (thermal coagulator) in women with stages I and II endometriosis. However, this approach requires further evaluation as part of randomized controlled trials.
Laparoscopic uterine nerve ablation (LUNA) and presacral neurectomy were also suggested as a treatment of pain symptoms. LUNA was found beneficial for dysmenorrhoea not associated with endometriosis (Johnson et al., 2004), while presacral neurectomy was found to reduce pain symptoms in endometriosis without significant side effects.
Laparoscopic uterine nerve ablation (LUNA) and presacral neurectomy were also suggested as a treatment of pain symptoms. LUNA was found beneficial for dysmenorrhoea not associated with endometriosis (Johnson et al., 2004), while presacral neurectomy was found to reduce pain symptoms in endometriosis without significant side effects.
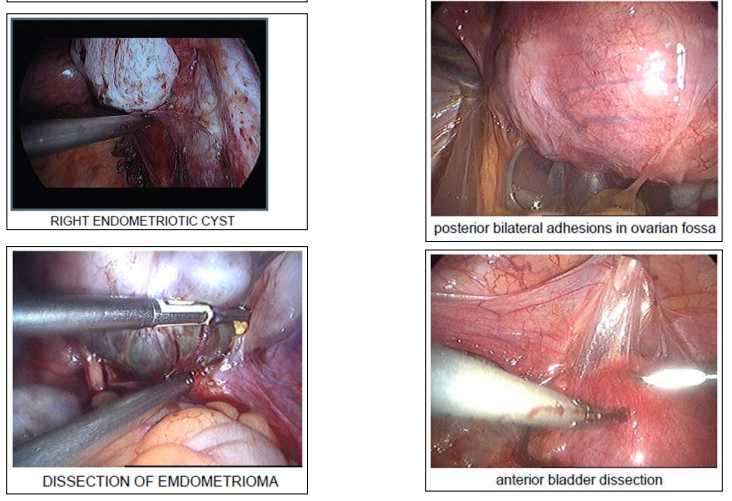
Operative laparoscopy should be the first choice for management of ovarian endometrioma whenever possible (Ruhlmann et al., 1996) and seems to be effective in alleviating pain associated with ovarian endometriomas (Yoshida et al., 2002). Medical therapy alone has not generally been effective in reducing endometrioma size and formed adhesions.
Deep endometriosis has been defined as endometriosis infiltrating deeper than 5 mm under the peritoneum (Koninckx and Martin, 1994). Unfortunately, the current classification of endometriosis is unsuccessful in predicting the major clinical outcomes, including pain symptoms.
Operative laparoscopy in terms of complete excision of the disease is efficient for the treatment of painful symptoms related to deep endometriosis infiltrating uterosacral ligaments. The segments of the rectum involved in the disease must be freed, leaving the deep endometriotic nodule attached to the posterior wall of the vagina. Resection of the whole lesion requires the posterior wall of the vagina to be resected and the vagina is usually opened, whereas ureterolysis is often unnecessary.
Because laparoscopic excision of deep bowel lesions has been associated with a residual of pelvic pain, laparotomy may sometimes be needed. Moreover, a new combined vaginallaparoscopic-abdominal approach was compared with laparoscopy, laparotomy and laparoscopy followed by laparotomy for bowel resection or laparoscopy followed by vaginal bowel resection for rectovaginal endometriosis. The new approach allows intraoperative digital bowel palpation to assess bowel infiltration and reduce unnecessary bowel resections and found to minimize complication rate, re-hospitalization rate, and hospitalization time.
The laparoscopic approach seems to have more favorable outcome than open approach in terms of quality of surgery and patients acceptance. Laparoscopic surgical management is now recognized as the best approach for endometriosis associated infertility treatment followed by assisted reproductive techniques. However, for endometriosis associated pain symptoms there is no general consensus regarding the best way of dealing with these symptoms. The problems of comorbidity and recurrence is still a problem and under great debate.
Infertility is common in endometriosis sufferers and is generally manifested as a reduced fecundity. Nevertheless, even in severe cases of endometriosis spontaneous successful conception and delivery of a healthy baby often occur. Despite enormous studies about the relationship between endometriosis and subfertility, this relationship still controversial issue. The main problems in those studies, that they don’t have a defined patient population, clinical features arising from different endometriosis types are not well defined and the fact that scientists investigating endometriosis are lacking enough clinical data about patients they are studying.
It seems that not one mechanism is responsible for the reduced fecundability in endometriosis it is rather a complex of several mechanisms rather than one mechanism. The problem of conflicting results in different studies about infertility in endometriosis may be due to the lack of proper characterization of patient population, the defects imbedded in the current classification of endometriosis and the difficulty of elimination of other factors that affect fertility such as sperm quality and different interpretation by different laboratories.
Laparoscopy is a widely used diagnostic and therapeutic means of treating endometriosis assosciated infertility.However,pregnancy outcome after laproscopy varies depending on preexisting tubal adhesions and endometriosis.minimal/mild endometriosis benifited the most from laproscopic manipulations when tubal adhesions were present .on the other hand ,IVF-ET outcome of patients who previously underwent laparoscopy was not influenced by prexisting tubal adhesions and endometriosis [1-25].