Author(s): Mukta verma
Introduction: Schwannomas are benign, encapsulated, silent, and usually solitary tumors originating from Schwann cells of the peripheral nerve sheath. Tibial nerve Schwannomas are very rare hence we are reporting this case for the better understanding of this unusual clinical entity.
Case Presentation: A 53-year-old male patient, truck- driver by occupation, arrived to our Plastic Surgery Department complaining of swelling, pain and paresthesia in the upper part of his right leg. These symptoms were present for about 8 months and were more apparent at the end of the day. There was no evidence of any other medical comorbidity like peripheral vascular disease. There was no history of prior traumatic events related to right lower limb. Thorough clinical examination and MRI supported the diagnosis of a benign peripheral nerve tumor and patient was treated by microsurgical excision of the lesion which completely relieved the patient’s symptoms.
Discussion: Mechanical compression caused by the space occupying lesion resulted in aggravation of symptoms. Classical burning/shooting pain and paresthesia often manifested by nerve sheath tumors. An increase in intracompartmental pressure resulted in pressure over nerve which consequently led to episodic pattern of neurological symptoms (diurnal variation in pain and paresthesia). Microsurgical excision of the tumor cured the symptoms completely and again patient was able to resume his regular day- to- day activities without any discomfort.
Conclusion: We describe a rare case of a patient with an unusual tibial nerve Schwannoma clinical presentation. Microsurgical excision of the space occupying lesion preserving the nerve fascicles play an important role in achieving the good post- surgical outcome. Medical literature on this topic is scarce hence this case report intends to add further data about such pathological conditions.
Schwannomas, or neurilemmomas, are benign soft-tissue tumors, which arise from the Schwann cells of the peripheral nerve sheaths [1,2]. Although they represent the commonest benign peripheral nerve sheath tumors, the occurrence on the lower limbs account for 1% of all cases [2].While usually clinically silent, they might be detected incidentally or become symptomatic due to mass effect and may present with pain, swelling and paresthesia(neurological symptoms). The diagnosis thus relies on the clinical history, physical examination, electrodiagnostic and imaging studies [2,3,5]. Magnetic resonance (MR) neurography is the diagnostic tool of choice when studying these sort of pathologic findings. MRI delineates the relationship of the mass lesion with the surrounding structures and determines whether the lesion is intrinsic or extrinsic to the nerve. The availability of MR neurography may be limited, and the costs can be significant, therefore high resolution ultrasonography (schwannomas are seen as well defined hypoechoic mass) may provide an economical and accurate imaging modality in diagnosis and management of these cases [6,8].
Histologically, schwannomas are biphasic tumors with highly ordered cellular component[ Antoni A] that palisades[verocay bodies] plus myxoid hypocellular component[ Antoni B ].They show strong immunoreactivity for S100. Depending on the symptoms, surgical treatment is usually advised [7]. Studies indicate that a schwannoma can be removed by delicate enucleation with an acceptable risk of injury to the nerve trunk. Here, we present a case of a patient with a Schwannoma located on the tibial nerve, presenting as popliteal fossa swelling, intermittent leg and foot pain with paresthesia [8].
A 53-year-old male, truck driver by occupation, presented to the Plastic Surgery Department with a painful swelling over the upper part of his right leg for the last 6 months. He also complained of leg pain and numbness for the last 8 months. Swelling was gradually increasing in size. The pain was moderate to severe in intensity, burning / sharp shooting in character and paroxysmal in nature. It irradiated to the foot and was made worse by brisk walk, crossing legs and prolonged standing. Pain was worst in the evening or at night. There was no history of any trauma and any surgical intervention in the past. Clinical examination revealed a firm single well defined oval swelling measuring 3 cm x 2 cm in the popliteal fossa with little mobility in the horizontal plane. The skin overlying swelling was normal in color and temperature. Surface was smooth and it was firm in consistency. There was moderate tenderness on deep palpation. On gentle percussion over the lesion, tingling sensation was perceived upto the foot. There was no sensory or motor deficit distal to the swelling. There was no significant past medical, surgical and family history.
On contrast-enhanced MRI T2- weighted imaging, a well defined ovoid mass was detected, with low signal intensity at the center and high signal intensity at the periphery involving the tibial nerve and demonstrating the nerve continuity. Tumor was eccentric to the nerve.
Microsurgical excision was planned under tourniquet control in spinal anaesthesia. Adjustable surgical binocular loupes were used to attain a magnified view of the surgical field. A vertical’ lazy S’ incision was given over swelling and with subcutaneous dissection it was observed that the tumor was in close proximity and along the tibial nerve, nerve was looped and retracted. The swelling and the contiguous portions of the affected nerve were exposed (Figure 1). Swelling was arising from the nerve sheath and the nerve fibers were crossing peripherally to the swelling. A vertical split incision was carefully made in the epineurium with the help of a new surgical blade no.15. The epineuria layers were gently peeled out until the smooth light yellow surface of tumor was exposed. Care was taken to avoid injury to visible nerve fascicles. The entire tumor mass was subsequently shelled out under loupe magnification with microsurgical instruments without any damage to the fascicles & was sent for histopathological examination. Tourniquet was deflated and hemostasis was secured using bipolar coagulator. Wound was sutured in layers with vicryl 3-0 and nylon 4-0 with corrugated rubber drain. Sterile dressing was applied over the suture- line and limb was splinted with knee joint in extension to avoid post operative discomfort and seroma formation.
The postoperative period was uneventful, the patient’s symptoms diminished considerably, and three months later he achieved complete healing and a symptom free state. He was able to walk without assistance and without pain or paresthesia.

Figure 1: Operative photograph showing a schwannoma of Tibial nerve

Figure 2: Intra -operative photograph showing the intact nerve after schwannoma excision
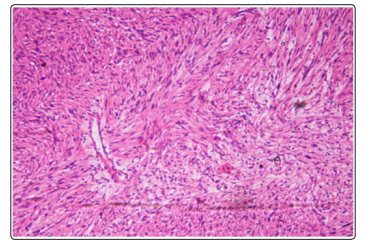
Figure 3: Histopathological photograph of Schwannoma showing characteristic Antoni A and Antoni B areas[H&E stain]
A Schwannoma, also known as neuroma, neurolemoma or Schwann cell tumor, is an encapsulated lesion that arises from the neurilemmal cells which normally produce the insulating myelin sheath covering peripheral nerves. Schwannomas are slow growing tumors that very rarely undergo malignant transformation [1,4].
Schwannomas most often occur in the fourth and fifth decade of life and seem to have a 1.6:1 female predilection. Schwannoms have been found to be present in such varied locations as the brachial plexus and the sciatic nerve [9]. Rarely, Schwannomas can be found in the leg or in the foot and ankle region. Schwannomas have a slow-growing pattern [10]. Usually they are clinically silent and present as an incidental finding. Patients may sometimes note cosmetic deformity or a palpable mass. Clear understanding of nerve structure and the peripheral nervous system aids diagnostic and therapeutic approaches to patients with peripheral nerve pathologic conditions [5]. The tibia nerve is a mixed motor and sensory nerve, supplies motor function to the intrinsic foot muscles, as well as sensation of the medial heel and plantar foot. Tibial nerve impairment symptoms may include paresthesia, pain and weakness of the knee or foot muscles.
In this case, the mechanical compression etiology is evident, since the pain and paresthesia were worsened after the prolonged standing, crossing legs and tensioning and or stretching themuscles of that anatomic region. In all these situations an increased pressure over the nerve resulted in an intermittent aggravation of symptoms. The evaluation of a patient with a suspected pathologic nerve condition mainly includes thorough history, clinical examination, and radiological investigations. Plain X-ray films may not reveal any changes whereas high resolution ultrasonography, computed tomography (CT), magnetic resonance (MR), especially MR Neurography, may exhibit a peripheral nerve tumor in a more detailed manner. Additional diagnostic tests, including electromyography (EMG) and nerve conduction study (NCS), evaluate neuromuscular function to assess denervation, preservation of motor units, or conduction loss [7,8].
On histopathological examination, Schwannomas appear solid or cystic and exhibit specific patterns: the Antoni A type has a spindle-cell array with collagen matrix arranged into palisading Verocay bodies; The Antoni B pattern exhibits a looser structure of mucinous matrix with fewer interspersed spindle cells; cellular Schwannomas display high cellular density and nuclear atypia, but contain fewer mitotic figures than malignant Schwannomas [7]. Differential diagnosis may include Neurofibroma, Leiomyoma, Leiomyosarcoma, Malignant melanoma and Malignant peripheral nerve sheath tumor (MPNST).All of them can be easily differentiated on the basis of histopathological findings and specific immunohistochemical stains [7,8].
Surgical excision is the treatment of choice. It should always be done under tourniquet control with magnification .Careful enucleation of schwannoma preserves most of the nerve fascicles and causes minimal nerve function impairment. Sometimes enucleaion of lesion may cause loss of few fascicles, in that case reconstruction with sural nerve graft can be done to restore the nerve function. Intra-operative nerve monitoring can also be done when feasible to achieve good post operative outcome, but it increases the cost and time of surgical procedure. Preservation of the nerve function and maintaining the continuity of the nerve is the main challenge [6,7].
In this clinical case, intermittent pain was a day-to-day normal activity limiting condition so surgical excision was done. Complete surgical resection of the tumor, while safeguarding the surrounding structures, resulted in complete cure.
One should consider schwannoma as a possible diagnosis for a well-defined, firm oval mass in patients with chronic pain and careful microsurgical dissection is needed under tourniquet control(for bloodless operative field) for excellent post operative results.
