Author(s): Rodríguez-Rivas Ricardo, Vazquez-Guevara Damaris, Monternach-Aguilar Felipe and Rodríguez-Leyva Ildefonso
Secondary central nervous system lymphoma is a complication from non-Hodgkin lymphoma not very well known. NHL can present in a variety of neurological clinical presentations varying from primary central nervous system lymphoma to complications from a systemic disease like metastasis or peripheral nerve involvement. We present a case of a 78-year-old male with Diffuse large B-cell lymphoma, treated with Cyclophosphamide, Doxorubicin, Vincristine, and Prednisone. Six months later of the diagnosis, the patient presented to the emergency department, complaining of five days with progressive weakness in the left upper limb, and two days before the weakness developed in the left lower limb. On the neurologic examination with inattention, dysarthria, left central facial nerve palsy, severe weakness on the left hemibody with hyperreflexia, and left extensor plantar response. Brain Magnetic resonance imaging reported three metastatic lesions, with a final diagnosis of secondary central nervous system lymphoma.
Secondary central nervous system lymphoma (SCNSL) is a complication from non-Hodgkin lymphoma (NHL) not very well known. NHL can present in a variety of neurological clinical presentations varying from primary central nervous system lymphoma (PCNSL) to complications from a systemic disease like metastasis or peripheral nerve involvement. The prevalence varies from different studies; especially, it is being described in follow up patients with aggressive lymphoma subtypes being described as a relapse from 2.8 % to 10.1% [1-3].
A 78-year-old male patient with no medical history. Approximately six months before, the patient presented with a loss of more than 10% of body weight and fatigue. During the workup, the abdominal computed tomography revealed a mass on the ileum. The patient underwent exploratory laparotomy, and a biopsy of ileum, cecum, and ascending colon were taken. The pathology report revealed Diffuse large B-cell lymphoma, and the immunohistochemistry was positive for CD20, CD10, CD5, BCL2, BCL6, CD43, 90% positive K167, and negative Cyclin D1.
The patient was referred to a Hematologist, the investigation for staging was a bone marrow biopsy with no infiltration, and the Fluorodeoxyglucose-positron emission tomography/computed tomography scan showing the cervical, thoracic, abdominal and inguinal lymph nodes and extranodal lesions in bones, lungs, and spleen. The diagnosis was a diffuse large B-Cell lymphoma Ann Arbor IV; after one week, then the patient received the first chemotherapy with Cyclophosphamide, Doxorubicin, Vincristine, Prednisone.
Six months later, the patient presented to the emergency department, complaining of five days with progressive weakness in the left upper limb, and two days before the weakness developed in the left lower limb. On the neurologic examination with inattention, dysarthria, left central facial nerve palsy, severe weakness on the left hemibody with hyperreflexia, and left extensor plantar response. Brain Magnetic resonance imaging (MRI) reported three metastatic lesions. The biggest was localized on the periventricular region of right parietal lobe with size 4.0x 3.7cm with necrosis inside, other on the parasagittal region of left occipital lobe with size 1.7x1.6cm, and the third one was on left parietal lobule with size 0.7x0.9cm, all lesions enhancement with gadolinium and shows restricted water on Diffusion-weighted imaging. The cerebral spinal fluid reported eight cells, 77.4 mg/dL proteins, 66.9 mg/dL glucose, and the cytology was reported negative for malignant cells, with a final diagnosis of secondary central nervous system lymphoma (SNCSL). However, two weeks after diagnosis, the patient died due to nosocomial pneumonia.

Figure A: Coronal (right), axial (left) postcontrast T1-weighted MRI shows a contrast-enhancing lesion on the periventricular region on the right parietal lobe
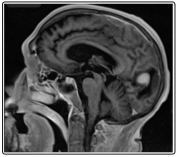
Figure B: Sagittal postcontrast T1-weighted MRI shows a contrast-enhancing lesion on the left occipital lobe
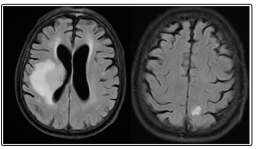
Figure C: Axial fluid-attenuated inversion recovery (FLAIR) MRI shows edema around the lesions
There are many differential diagnoses in the spectrum of confounders for central nervous system lymphomas. Tumors like high-grade gliomas and meningioma, granulomatous and demyelinating diseases, as well as vasculitis, have been described as diagnosis possibilities. Metastatic disease from systemic malignancies, as well as an infectious disease within the neuraxis, can also present similarly and must be ruled out. Additionally, infectious etiologies such as cerebral toxoplasmosis must be considered possibilities in immunocompromised patients [4].
Initial treatment is focused on the improvement of the CNS symptoms like headaches, radicular pain, and seizures. Dexamethasone is often given with this purpose, improving radicular pain, headache, and lowering of vasogenic edema; however, the use of steroids can alter histopathologic studies and delay/alter diagnostic tests. Anticonvulsant treatment should be used in patients presenting with seizures as in other CNS tumors, but as in the later, anticonvulsant medications prophylaxis is not indicated or has not proved any benefit in quality of life. Systemic therapy with methotrexate and cytarabine has been used for SCNSL involvement with good results, but it has the risk of systemic toxicity, and it is levels in CNS are not as elevated as in intrathecal therapy. Recently stem cell transplant after high dose chemotherapy has been used in different clinical trials showing more prolonged survival. Intrathecal therapy (Via Ommaya reservoir over lumbar puncture (LP)) is preferred in patients with leptomeningeal involvement, cytarabine, methotrexate, and hydrocortisone have demonstrated effects on this complication. Radiation therapy should be considered in patients who are not candidates for high dose systemic chemotherapy. Rituximab has not yet shown satisfactory results as the first-choice therapy for secondary CNS non-Hodgkin lymphoma [5,6].
There are a variety of factors that increase the chance of secondary CNS involvement in non-Hodgkin lymphoma. Histologic subtypes, especially high-grade lymphomas (Burkitt lymphoma, lymphoblastic lymphoma, large B cell lymphoma, and mantle cell lymphoma), have been described. The primary site has also been studied as a risk factor. However, only lymphomatous involvement of testicles, paranasal sinuses, patients with retroperitoneal lymph nodes and primary mediastinal large B cell lymphoma have been found to have an apparent risk augmentation. Hollender described a group of independent risk factors: Age > 60 years, elevated lactic dehydrogenase (LDH), albumin < 3.5 g/dL, retroperitoneal lymph node involvement, and involvement of >1 extra-nodal site. If a patient has 4/5 of them, the risk of CNS involvement in the next five years was higher than 25%; some of these five risk factors have been studied separately and been found to have a lower but increment in CNS recurrence [3,7-9].
The survival rate of secondary CNS lymphoma is reduced. Median survival after the diagnosis of CNS lymphoma varies from 2 to 6 months. One study at the University of Rochester Medical Center, Rochester, New York, showed a median survival of 3 months and only two months if the patient had Diffuse large B cell lymphoma subtype. Chemotherapy plus hematopoietic stem cell transplantation has shown different results from not improving survival rate to extending life expectancy [10-12].
The course of clinical presentation typically appears in an acutesubacute fashion, with symptoms appearing and evolving from days to weeks, varying from a pyramidal syndrome, hemiparesis, headache, meningeal-encephalitic syndrome, radicular and medullary syndrome [2,13].
The most common form of CNS is leptomeningeal metastasis in 4-8% of patients. However, the true incidence is believed to remained unmasked because of under-recognition; typical clinical presentation shows as multiple cranial neuropathies in 80% of lymphomatous meningitis, especially involving cranial nerves II, III, V; VI, VII, VIII, and XII. The leptomeningeal syndrome can involve meninges, spinal cord, and roots with few case reports of equine cauda syndrome around world literature. Seizures, hydrocephalus, papilledema, and hypothalamic dysfunction has also been reported. Diagnosis of this complication it has made with CSF cytology examination, with the recommendation of examination of at least three tubes with 10cc of CSF and it should be processed immediately; however, this technique has a low rate of success detecting malignant cells, with a reported 60% rate of detection with just an LP, with an increased rate to 93% with a second LP. Other recommendations are the use of flow cytometry and PCR techniques to help confirm the diagnosis. Also, it has been reported a higher diagnosis rate depending on the place where the CSF was obtained according to clinical presentation (Ommaya reservoir vs. LP)1[13-16].
Parenchymal brain metastasis is the second most common typical presentation, with some studies showing an increase in the prevalence of this complication, and reports from PCNSL being the most common site of CNS involvement. A typical presentation will depend on localization, seizures, motor, sensory deficits, and depressed level of consciousness if ICP is high. Localization is most common supratentorial in more than 80% of cases, being periventricular white matter and basal ganglia, the most commonly reported followed by ependymal extension, the later of great importance for differential diagnosis in imaging [17-19]. Classical MRI appearance shows single or multiple lesions isointense or hypointense in T1WI, homogenously isointense or hypointense to the cortex in T2 and enhancing lesion with contrast. Diffusionweighted magnetic resonance imaging shows restricted water intramedullary spinal dissemination (IMD) it is rarely described in the literature, one of the most extensive reviews of IMD published that only 7.6% of 79 patients with this complication of cancer of any time was due to non-Hodgkin lymphoma infiltration. Secondary intramedullary dissemination it is explained by hematogenous dissemination, venous spreading through Batson’s plexus of lymphatic spread. Described symptoms for spinal cord lymphomas are weakness, sensory loss, spasticity, pain, and bowel or bladder incontinence, with no reported clinical difference with primary or secondary CNS lymphoma. MRI is the study of choice for diagnosis of IMD, classical presentation shows the isointense signal to the spinal cord in T1 and hyperintensity in T2 and STIR signal (Short T1 Inversion Recovery), which is characteristically different to the low T2 intensity seen in intracranial lesions. The majority of cases show lesions that enhance homogenously with contrast, but sometimes it has been described that the enhancement is mild and typical ring pattern may be absent. The rest of the workup studies include, just like in lymphomatous meningitis CSF analysis and flow cytometry. Biopsy of the spinal cord has not been described as a classic alternative, and it should be made just in cases where laboratory and imaging are inconclusive [20,21]
Neurolymphomatosis secondary to CNS lymphoma secondary invasion is a rare complication. It presents with the direct involvement of peripheral nerves, typically affecting cranial nerves or spinal nerve roots. In a case series review, diffuse large B cell lymphoma was the histological type most related to NonHodgkin lymphoma, and painful neuropathy was the most reported complication. CSF analysis and nerve conduction studies do not seem to help improve diagnosis of this complication, being nerve biopsy and PET-SCAN the most helpful [22].
1. Secondary central nervous system lymphoma is a not very well-known complication from LNH with a myriad of neurological clinical presentations.
2. There is a wide number of differential diagnoses that can simulate this pathology.
3. Systemic therapy with methotrexate and cytarabine has been used for secondary CNS non-Hodgkin lymphoma involvement with good results, but it has risk of systemic toxicity, and it is levels in CNS are not as elevated as in intrathecal therapy.
4. Independent risk factors for involvement of CNS: Age > 60 years, elevated LDH, albumin < 3.5 g/dL, retroperitoneal lymph node involvement, and involvement of >1 extra-nodal site.
5. The survival rate of secondary CNS lymphoma is reduced.
